More Information
Submitted: February 05, 2021 | Approved: February 15, 2021 | Published: February 16, 2021
How to cite this article: Nikhra V. Living with ‘Long COVID-19’: The long-term complications and sequelae. Int J Clin Virol. 2021; 5: 011-021.
DOI: 10.29328/journal.ijcv.1001030
ORCiD: orcid.org/0000-0003-0859-5232
Copyright License: © 2021 Nikhra V. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: COVID-19; Long COVID; Long haulers; Post-COVID myocarditis; Pulmonary fibrosis; Brain fog; Chronic fatigue syndrome; Holistic care
Living with ‘Long COVID-19’: The long-term complications and sequelae
Vinod Nikhra*
Senior Chief Medical Officer and Consultant, Department of Medicine, Hindu Rao Hospital and NDMC Medical College, New Delhi, India
*Address for Correspondence: Dr. Vinod Nikhra, Senior Chief Medical Officer and Consultant, Department of Medicine, Hindu Rao Hospital and NDMC Medical College, New Delhi, India, Email: drvinodnikhra@gmail.com; drvinodnikhra@rediffmail.com
Introduction - the perennial pandemic: It is being increasingly realised that the COVID-19 may have become the new reality associated with human existence world over and the mankind may have to live with it for years or even decades. Further, the grievous nature of the disease is evolving further with the genomic changes in the virus in form of mutations and evolution of variants, with enhanced infectivity and probably virulence. There are serious challenges posed by the SARS-CoV-2 virus and COVID-19 as the disease.
COVID-19 as acute and chronic disease: On exposure to the SARS-CoV-2 virus, not all patients develop a disease. Further, for those who develop the disease, there is a large variation in disease severity. The known factors including the constituent factors and several still unknown factors influence the disease manifestations, its course, and later the convalescent phase as well. In fact, substantial continuing morbidity after resolution of the infection indicates persisting multisystem effects of COVID-19.
The ‘long COVID-19’ or ‘long haulers’: The patients who continue to suffer with persisting symptoms have been described as long haulers and the clinical condition has been called post-COVID-19 or ‘long COVID-19’. The diagnosis should be entertained if various symptoms and signs linger well beyond the period of convalescence in COVID-19. With the chronicity, there occur inflammatory changes and damage in various organs, and the extent of organ damage determines the long-term effects.
Management of ‘long COVID’ syndrome: The ‘long COVID’ syndrome has multi-system involvement, variable presentation, and unpredictable course. Following clinical and investigational assessment, the patients should be managed as per clinical manifestations, extent of organ damage and associated complications. The findings from various studies indicate that preventing further organ damage in ‘long COVID’ is crucial.
The long COVID’s prognostic challenges: As apparent, the ‘long COVID’ afflictions are more common than realized earlier. The symptoms can escalate in patients with co-morbid conditions. The persistent symptoms among COVID-19 survivors pose new challenges to the healthcare providers and may be suitably managed with a combination of pharmacological and non-pharmacological treatments, and holistic healthcare.
The perennial pandemic
It is being increasingly realized that the COVID-19 may have become the new reality associated with human existence world over. The mankind may have to live with COVID-19 for years or even decades [1]. Following infection, the C19 virus becomes an intracellular entity that has penetrated the cell walls. It may not be possible to destroy the intracellular virions. Further, while we continue to explore the agent factors, disease transmission dynamics, pathogenesis and clinical spectrum of the disease, and therapeutic modalities, the grievous nature of the disease is evolving further with the genomic changes in the virus and pathophysiological alterations and clinical manifestation. The future of the disease, of course, is stated to depend on various known and unknown factors, many of them may not be modifiable. Let us learn to live with this reality.
Apart from being a pandemic, COVID-19 has become a perennial disease. There are serious challenges posed by SARS-CoV-2 virus and COVID-19 as the disease that are further increased by mutations and evolution of variants with enhanced infectivity and probably virulence. The significance of viral mutations needs to be highlighted and investigated further, which may help in designing therapeutics to combat the disease as well as developing effective vaccines for its prophylaxis. In addition, the fields of improving the immune response to the infection and vaccine shots and the immunity in general are to be explored and harnessed. Looking forward, let us hope that the today’s unmet challenges are resolved in near future [2].
Acute COVID-19: The clinical spectrum
Being exposed to the SARS-CoV-2 virus, not all infected patients develop a disease. It may be remembered a significant number of those get infected with the SARS-CoV-2 virus are asymptomatic: In fact, a recent systematic review has documented that at least one-third of SARS-CoV-2 infections occur in people who never develop symptoms, highlighting the substantial prevalence of asymptomatic infections [3]. The study included serologic surveys from more than 365,000 people in England and more than 61,000 in Spain. When analyzed, a similar proportion of asymptomatic cases 32.4% in England and 33% in Spain was noted.
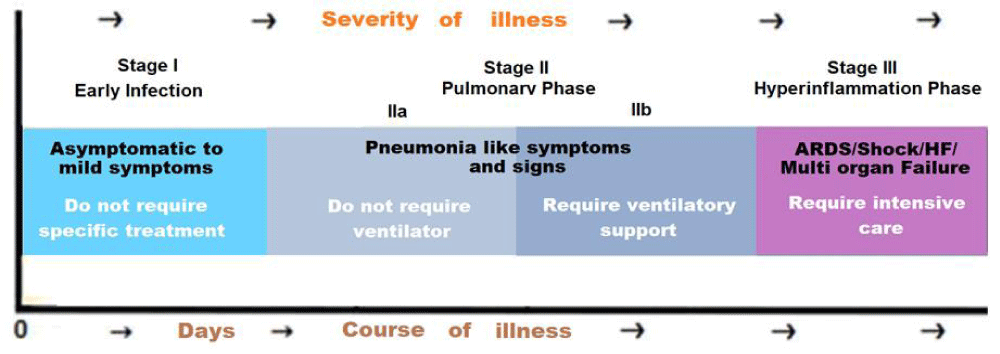
Further, for those who develop the disease, there is a large variation in disease severity, one component of which may be due to the genetic variability in the response to the virus [4]. The individual response following the SARS-CoV-2 exposure and the vulnerability of individuals to infection, and the clinical spectrum of COVID-19 is greatly variable (Figure 1).
Figure 1: The clinical spectrum of COVID-19.
The clinical manifestations of COVID-19 patients have been grouped based on the need for hospitalization, need for oxygen supplementation, and progression to respiratory failure, or mortality. Presently, considering the post-illness symptoms and manifestations, the resolution phase can be added to this.
Factors influencing the disease course
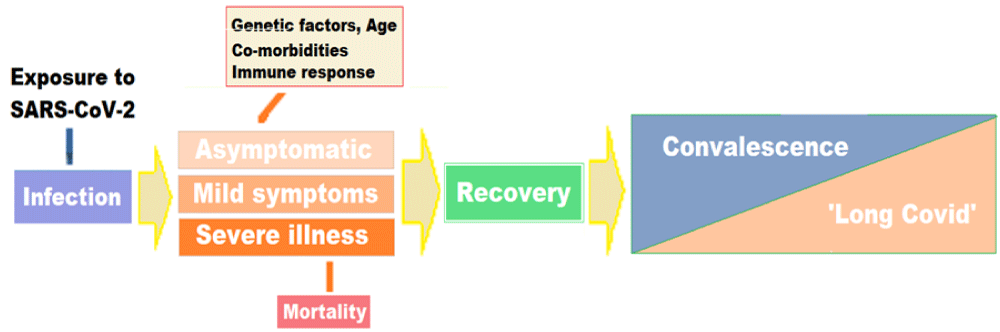
Further, it is becoming clear that apart from the advanced age and pre-existing conditions, such as diabetes, cardiovascular, pulmonary, and renal diseases, certain constituent factors render some patients more vulnerable to the more severe forms of the diseases, as is apparent from the rate of hospitalization of younger and apparently healthy individuals. The known factors including the constituent factors and several still unknown factors may influence the disease manifestations, its course, and later the convalescent phase as well. From the clinical perspective, knowledge of host constituent factors, including the genetic variations, could lead to improved care for patients with COVID-19 during the acute phase of the disease as well as during the resolution phase encompassing convalescence and ‘long COVID’ phase. The host genetic factors have been linked to the variable clinical manifestations of the disease following exposure to the virus at the individual level as well as in various population groups [5]. In fact, a model to understand several related factors such as the age, associated co-morbidities and genetic factors including human genomic variants linked to COVID-19 outcomes can be conceived as a continuum from ultra-rare to common (Figure 2).
Figure 2: The factors related to the disease - clinical course, convalescence, and ‘long COVID’.
The genetic factors and pathways related to COVID-19 involve the ACE2 gene encoding the ACE2 surface receptor associated with SARS-CoV-2 virus. The specific variants in the genes and pathways leads to inter-individual COVID-19 susceptibility and response. The genetic polymorphisms in the ACE2 gene, which encodes the ACE2 receptors and allelic variants of the ACE2 may influence the virus binding subsequent invasion of the cell. In addition, the genetic factors and pathways also include the polymorphisms of cellular proteases, which facilitate the entry of SARS-CoV-2 into the cell, along with furin and TMPRSS2. The TMPRSS2 variants and resulting expression may also influence COVID-19 severity, as well. Other genes of interest include genes associated with ABO blood group [6].
There is a possible association between the genetic variability in histocompatibility complex (MHC) class I genes (human leukocyte antigen - HLA A, B, and C) and the susceptibility to the virus and disease severity [7]. In particular, the HLA-B*46:01 gene product exhibits the low binding capacity to SARS-CoV-2 peptides resulting in the individuals with this allele being more susceptible to COVID-19 due to reduced capacity for viral antigen presentation to immune cells. On the other hand, the HLA-B*15:03-encoded protein has a high binding capacity to SARS-CoV-2 peptides and present to immune cells leading the patients with this HLA genotype to develop better immunity. The human genomic factors can also be linked to variability in the protective immune response through the inflammatory and immune response pathways such as IL-6 pathway, and genes involved in hypercoagulability and acute respiratory distress syndrome. The variable immune response has implications for vaccination strategies and for optimally selecting patients for novel therapeutic treatments and trials.
To track the acute as well as long-term impact of the disease on health, the project called the COVID Human Genetic Effort, aims to find genetic variants that compromise the immune systems and making certain individuals more vulnerable to the risk of developing COVID-19. In addition, it aims to document the genetic variations which make some individuals resistant to the SARS-CoV2 infection [8]. In nutshell, the project aims to discover – (1) Monogenic inborn errors of immunity (IEI), rare or common, underlying severe forms of COVID-19 in previously healthy individuals, and (2) Monogenic variations which make certain individuals resistant to the SARS-CoV2 infection despite repeated exposure, and (3) decipher the molecular, cellular, and immunological mechanisms by which they cause resistance to viral infection or predisposition to a severe form of the disease.
COVID-19 delayed and long-term effects
There is a growing evidence of persisting multisystem effects of COVID-19, indicating substantial continuing morbidity after resolution of the infection [9]. While most people recover quickly and completely from the virus, persistent and troubling symptoms are frequently seen and reports from cohort studies suggest that one in three people have not fully recovered several weeks after initial illness and a smaller but still substantial proportion have symptoms and difficulties that persist for months [10]. Further, the long-term effects of COVID-19 are seen in the younger population also, though the risk of ‘long COVID’ increases with age. People who suffer with severe form of the disease, experience long-term inflammation and damage in lungs, heart, immune system, brain, the vasculature, and other organs. These long-term effects can last for months and years. The ‘long COVID’ is not contagious and result of the body’s response to the virus infection continuing beyond the initial illness. Thus, the unmitigated COVID-19 infection has impact on the health of all groups and the strategies for prevention and suppression of COVID-19 should focus the older people or those with comorbidities, but also the younger population.
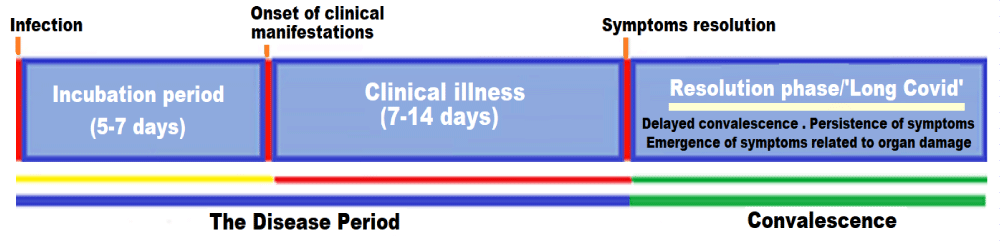
Most COVID-19 patients recover within a few weeks without significant complications. But some patients, even those who had mild versions of the disease, including the younger people afflicted with mild or asymptomatic disease and those who did not suffer with serious disease or require hospitalization, may continue to experience symptoms after their initial recovery [11]. These patients have been described as long haulers and the clinical condition due to persisting or continuing symptoms has been called post-COVID-19 syndrome or ‘long COVID-19’. The clinical condition encompasses a delayed convalescence or recovery, persistence of symptoms, and emergence of symptoms related to the organs involved and damaged, and incapacitating complications and sequelae (Figure 3).
Figure 3: The abnormal convalescence or resolution phase following COVID-19 illness: delayed convalescence, persistence of symptoms, and emergence of symptoms related to organs affected, and prolonged recovery and incapacitating complications and sequelae.
Often the symptoms may go un-noticed, as they are vague and nonspecific, but persist making the patients to suffer with the COVID-19-related ordeals. Further, of various the facets of the disease, this one may ultimately prove to be the most difficult to deal with. The long-haul COVID patients carry their symptoms well beyond the normal course of recovery lasting for weeks and months or longer. These symptoms are often varied and relatively common and may defy a COVID-related diagnosis. Several patients who are expected to recover, continue to suffer for a variable period of weeks and months with various general symptoms such as fatigue, dizziness, memory lapses and other cognitive issues, digestive problems, erratic heart rates, headaches, fluctuating blood pressure, and muscular and joint pains, which are often considered by the patient himself and family members as related to the weakness developed following the disease.
The older people and those with serious co-morbid medical conditions are the most likely to experience lingering COVID-19 symptoms, but even young, otherwise healthy people can continue to suffer and feel unwell for weeks to months after infection. These patients are reporting weeks and months-long symptoms that affect various organs. Given the multitude of COVID-19 cases worldwide, the prevalence of ‘long COVID’ is expected to be substantial and likely to increase with the recurrent outbreaks of the disease. It is feared that the ‘long COVID’ with debilitating and prolonged illness may have profound impact on health of people, their social life and livelihoods, and the economy.
The presentation of ‘long COVID’ symptoms
The occurrence of persistence or appearance symptoms related to ‘Long-COVID’ are being increasingly reported. Over the past few months evidence has mounted about the serious long-term effects of COVID-19 and it is estimated that we probably have way more than five million people with long COVID. The worldwide percentages of infection suggest that many of those people are living and suffering in the U.S. The ‘long COVID is neither well-defined nor well understood, partly because the related research is still in its infancy. The syndrome has vastly emerged from self-reporting and appears to be a real clinical entity with the chronic health manifestations. The symptoms persist or develop outside the initial viral infection, and the duration and pathogenesis are unknown. Late sequelae have been described even in young, healthy people who had mild initial infection, and there is often a relapsing and remitting pattern. There are vague to severe incapacitating symptoms.
The syndrome has been documented to affect a significant number of individuals. Further, the post-COVID symptoms tend to be more common, severe, and longer-lasting than other viral illnesses, such as influenza. The cause of ‘long COVID’ is not known. It may be due to an immune-inflammatory response gone berserk or related to persistent viraemia due to weak or absent antibody response and the ongoing viral activity. Other factors like and psychological factors such as post-traumatic stress and deconditioning may be involved leading to neuropsychiatric sequelae. The long term respiratory, cardiovascular, and musculoskeletal injuries have also been described for SARS and MERS, and the post-acute COVID-19 is likely to have similar pathophysiology. The etiology is likely to be multifactorial and may involve overzealous immune responses, cardiopulmonary or systemic inflammation, vascular inflammation and coagulation disorders, and a direct cellular damage from viral replication during acute illness. Further, there is little known about the prevalence, risk factors, or possibility to predict about the protracted course early in the course of the disease. In general, the ‘Long COVID’ is characterised by symptoms of fatigue, headache, dyspnoea, and anosmia and likely to increase with age, higher BMI, and female sex. Further, as documented experiencing more than five symptoms during the first week of illness is associated with ‘Long-COVID’.
In a study with online survey data involving over 4,000 COVID-19 patients, about 13.3% of all ages suffered with the symptoms lasting > 28 days, whereas 10% of those aged 18-49 years had the related symptoms 4 weeks after acquiring the infection. Further 4.5% of all ages suffered with the symptoms for more than 8 weeks, and 2.3% of all ages for more than 12 weeks. The study was conducted by health-science firm Zoe Global Limited in conjunction with Biomedical Research Centre based at GSTT NHS Foundation Trust and supported by the UK Research and Innovation [12]. The analysis and inference derived from similar studies could be used to identifying individuals with ‘Long-COVID’ may help to reduce long-term complications and sequelae and planning health education, guidance, and rehabilitation services [13].
Diagnosis and manifestations of ‘long COVID’
As a matter of fact, medical advice should be routinely sought for all the patients having delayed recovery and persistence or emergence of symptoms. There is a multitude of adverse physical and mental health effects due to COVID-19. The evidence from other coronavirus infections such as the severe acute respiratory syndrome (SARS) and MERS epidemic suggests that these COVID-19 afflictions may last from months to years. This being the other side of the disease, a prolonged medical follow-up of COVID-19 patients is essential. According to a study published in the Lancet, which included 1,733 people tested positive for COVID-19 and followed for 4 months, found that more than 75% of the people who were hospitalized for COVID-19, suffer with at least one symptom 6 months after recovery. Further, it was noted that about 76% of them experienced lingering symptoms of COVID-19 long after being cured of the illness [14].
From the clinical perspective, the COVID-19 incubation period and clinical phase involves 3 weeks, the post-acute COVID can be described as the illness extending beyond three weeks from the onset of first symptoms, and the chronic COVID-19 as extending beyond 12 weeks. Around 10% of patients who have tested positive for SARS-CoV-2 virus remain unwell beyond three weeks, and a smaller proportion for further period. The diagnosis of the ‘Long COVID’ or ‘Long haulers” should be entertained for various symptoms and signs linger well beyond the period of convalescence in COVID-19.
• The most common of persisting signs and symptoms of post-COVID-19 illness include:Extreme tiredness (fatigue), giddiness, paraesthesia, and joint and muscle pains
• Chest pain and tightness, palpitations, shortness of breath and Cough
• Persistence of Loss of smell or taste
• Gastrointestinal upsets such as anorexia, nausea, vomiting, diarrhoea, and stomach aches
• Headache and neurocognitive difficulties related to memory and concentration (‘brain fog’)
• Mental health conditions such as anxiety, insomnia, and depression, and post-traumatic stress syndrome
• Metabolic disruptions such as altered thyroid function, poor control of diabetes, etc.
• Seizures, facial paralysis, impaired vision and hearing, and tinnitus and earaches
• Skin rash like vesicular, maculopapular, urticarial, or chilblain-like lesions and hair loss.
The post-exercise malaise following physical activity and chronic fatigue are the commonest symptoms witnessed in ‘long COVID’ during a follow up of 6 months. It has been experienced by a substantial number of patients that the relapses are triggered by stress or exercise and they are unable to work at full capacity (about 45% required a reduced work schedule and about 22% were not working at all) prior to the infection. Another most insidious long-term effect of COVID-19 is cognitive dysfunction (or ‘brain fog’). Following the infection, a significant number of patients report crippling exhaustion and malaise and find ordinary activities like getting out of bed or going to work tiresome. In a study of 143 COVID-19 patients discharged from a hospital in Rome, about 53% complained of fatigue and 43% of shortness of breath [15].
Further, the patients with severe COVID-19 disease commonly experience sequelae affecting their respiratory status, physical health, and mental health for at least several weeks after hospital discharge. A study of patients in China showed that about 25% of them had abnormal lung function after 3 months, and that 16% were still fatigued [14]. The symptoms resemble chronic fatigue syndrome, also known as myalgic encephalomyelitis (ME). Since there being no biomarkers, diagnosis is based on symptoms. Further, the chronic fatigue is not limited to severe cases and common in even those who had mild symptoms. The persistent low-level inflammation triggered by infection appears to be the cause partly. The treatment is only imperative.
The study by Davis et al. surveyed more than 3,700 people from 56 countries who had contracted COVID-19 between December 2019 and May 2020 [16]. There were recorded 205 symptoms across 10 organ systems and traced 66 symptoms over 7 months. Over 65% of respondents experienced symptoms for at least 6 months. The most often reported symptoms were fatigue and post-exercise malaise, in addition to vague neurological sensations, headaches, memory issues, muscle aches, insomnia, palpitations, shortness of breath, dizziness, gait imbalance and speech disorders. In general, the long-term neurological symptoms were common even among patients with less severe disease. The less common manifestations of ‘long COVID’ reported are seizures, facial paralysis, impaired vision and hearing, prolonged loss of taste and smell, and some form of allergies [17,18].
In another recent study, Carvalho-Schneider, et al. followed-up of 150 adults with only mild to moderate COVID cases for two-month and found that two thirds of them were still experiencing symptoms, most commonly shortness of breath, loss of smell and taste, and/or asthenia and fatigue [19]. Another study by Italian researchers, covering 143 COVID patients who had been discharged from the hospital, found that only about one in eight was completely free of symptoms 60 days from the beginnings of the illness [20]. The King’s College London study, one of the largest surveys so far, reported that around 10 percent of patients had persistent symptoms for one month, with 1.5% to 2% having sustained symptoms at three months. Further, the study documented that long COVID was twice as common in women as men, and the older people, and those with more than five symptoms during their first week of illness were more likely to develop ‘long COVID’ [12].
The organ involvement in ‘long COVID’
COVID-19 as a disease primarily affects the lungs, but the virus can attack and injure other organs and cause some a multitude of symptoms. COVID-19 often strikes the lungs first, as the cells in upper and lower respiratory tracts richly harbour the ACE2 receptor which is the major target of SARS-CoV-2 virus. In addition, the infection can harm the immune system, which pervades the whole body. Some people who have recovered from COVID-19 could be left with a weakened immune system. For a long time, they are likely to be immunosuppressed and vulnerable to other infections.
In general, the extent of organ damage determines the long-term effects. The organs and systems affected by COVID-19 include:
• Lungs - The lung involvement in COVID-19 cause alveolar damage depending on the disease severity [21]. The alveolar damage is followed by pulmonary fibrosis resulting in long-term respiratory symptoms [22]. In the light of the pathophysiology of COVID-19, as the disease begins and primarily affects the respiratory system, the lungs are the obvious place to check for long-term damage [23].
The lung damage associated with the ‘long COVID’ on the chest scans reveals that even in the early weeks following recovery from COVID-19 infection, some patients have distinct signs of alveolar tissue damage leading to scar and fibrosis. As noted by Gholamrezanezhad, et al, in majority of the confirmed COVID-19 patients, computed tomography (CT) examinations yield a typical pattern with the sensitivity of 97% [24]. On follow up, in more than one-third of patients after one month, the tissue damage leads to visible scars and these patients representing with intermediate-term lung damage are likely to experience lasting respiratory symptoms. In an Italian study, a large proportion of patients (over 70%) with COVID-19 presented during follow up with symptoms including cough, fever, dyspnoea, musculoskeletal symptoms (myalgia, joint pain, fatigue), gastrointestinal symptoms, and anosmia/dysgeusia [9].
The persistent shortness of breath and not being able to carry out the usual exertional activities like climb up a few flights of stairs, without getting breathlessness are common symptoms seen in ‘long COVID’ patients. Various small studies have correlated the lung findings like fibrosis with the persistent lung symptoms. A retrospective multicenter study involving 55 recovered noncritical patients documented that over 60% patients had persistent symptoms three months following discharge, whereas over 70% had abnormal findings on lung CT scans and about 25% had demonstrable significant abnormalities in pulmonary function tests [25].
It has been found that the lower lobes of the lungs are the most frequently affected. The CT scans during the acute infection commonly show opaque patches indicating inflammation, which usually reduce in most cases after two weeks. An Austrian study also confirmed that lung damage seen on scans lessened with time: 88% of participants had visible damage 6 weeks after being discharged from hospital and after 12 weeks only 56% showed lung damage [26]. It has been noted in a prospective follow-up of patients infected with the coronavirus that COVID-19 patients may suffer long-term lung and heart damage but, for a significant proportion, this tends to improve over time [27]. On the other hand, though the lung scans can improve with time, many patients continue to suffer with lasting symptoms which may take a long time to resolve, as highlighted in post-discharge patients 70% of whom continued to suffer with shortness of breath and 13.5% were still using oxygen at home [28]. The past evidence from people infected with SARS and MERS also suggests that the lung injury and symptoms may linger for some. This is also suggested by a study published in February 2020 highlighting the long-term lung harm in SARS patients due to SARS-CoV-1, in which even after 15 years (between 2003 and 2018) 4.6% of SARS patients had visible lesions on their lung scans, and 38% had reduced diffusion capacity [29].
• Heart – Various clinical studies have shown that COVID-19 patients may suffer with complications like myocarditis and cardiomyopathy, abnormal heart rhythms and other cardiac sequelae weeks and months after contracting the infection [30]. The myocardial damage increases the risk of heart failure and other related complications [31]. The exact prevalence of cardiovascular disease (CVD) in COVID-19 patients is not known, but pre-existing CVD may be associated with a more severe COVID-19 infection [32].
It appears that about 20% of patients admitted with COVID-19 have clinically significant cardiac involvement. Cardiopulmonary complications include myocarditis, pericarditis, myocardial infarction, dysrhythmias, and pulmonary embolus; they may present several weeks after acute COVID-19. They are commoner in patients with pre-existing cardiovascular disease, but they have also been described in young, previously active patients. The occult involvement is common and add to post-COVID complications [33].
Various related studies appear to help explain the cause of shortness of breath, palpitations, and other cardiac symptoms in ‘long COVID’ patients. The imaging studies may indicate damage to myocardium weeks and months following recovery, even in those who had only mild COVID-19 symptoms. In a non–peer reviewed study involving 139 health care workers following recovery from COVID-19, 37% of them were found to have developed myocarditis and myopericarditis on their scans about 10 weeks after initial infection, but only half of them had showed related symptoms [34].
• Brain – The ‘long COVID’ is commonly associated with mild neurologic symptoms such as ‘brain fog’, dizziness, headache, insomnia, loss of smell or taste, etc. [35]. On the serious side, in any age group, COVID-19 can cause ischemic strokes, cranial neuropathies and Guillain-Barre syndrome during the acute phase as well as during the chronic phase. Carlos del Rio, et al. have described encephalitis due to the virus and occurrence of ‘brain fog’ and seizures several months following the initial infection [11]. Further, COVID-19 increases the risk of neurodegenerative disorders such as Parkinson’s disease and Alzheimer’s disease in long term.
It has been found that the serious neurologic manifestations are more likely to occur in patients who have suffered with severe COVID-19 disease, are older and have co-morbidities [36]. In addition, these patients are more likely to present with myalgic encephalomyelitis /chronic fatigue syndrome (ME/CFS) like other viral infections such as SARS, MERS, and HIV.
In addition, they are also more likely to suffer with neurological complications like cognitive difficulties, including confusion and memory loss, persisting for a longer duration.
It appears that the virus may not infect the brain and the symptoms are a secondary consequence of cerebral inflammation [37]. The various mental health related outcomes such as anxiety, hopelessness, ‘brain fog’, depression and post-traumatic stress disorder are more common in patients with serious disease and may have a link with cerebral inflammation. Further research and long-term studies in due course may provide better understanding of the neurological and psychological manifestations of COVID-19.
• Blood vessels - COVID-19 affects small blood vessels as well as large vessels leading to vasculopathy and coagulopathy. The involvement of major vessels can result in acute coronary and cerebrovascular events, whereas the involvement of small blood vessels, arterioles, and capillaries in the heart lead to myocarditis and cardiomyopathy, and acute renal injury, acute injuries in other organs.In addition, the immune system becomes overactive and triggers harmful widespread inflammation and organ damage. The over-reactive immune system through inflammation and tissue damage leads to cardiovascular manifestations such as cardiomyopathy and pulmonary thrombosis in almost one-third of patients during the acute phase of COVID-19, affecting the ejection fraction of heart. In addition, the virus can infect the endothelial cells in blood vessels of various organs [38]. The cardiovascular system affliction may linger on for a prolonged time. The patients with COVID-19 pneumonia are at increased risk of long-term cardiovascular manifestations [39].
• Further, various long-term COVID-19 related effects are still unknown and may become apparent only later. There are concerns that the pandemic will lead to a significant surge of people battling with lasting symptoms and disabilities resulting due to the infecting virus and subsequent inflammatory process. In addition, some of the organ injury is likely to be a side effect of intensive treatments such as intubation, ventilatory therapy related and therapeutic agents used during hospitalization.
Management of ‘long COVID’ syndrome
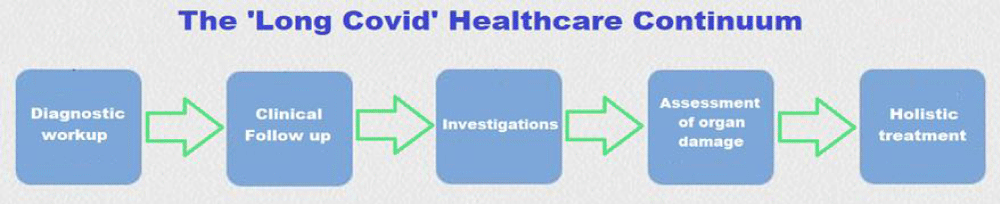
There is a healthcare continuum for management of ‘long COVID’ encompassing diagnostic workup, clinical follow up, investigational workup, followed by assessment of organ damage and treatment which involves pharmacological as well as non-pharmacological treatment, and holistic care (Figure 4).
Figure 4: The ‘long COVID’ care and management continuum – Diagnosis, Clinical follow up, Investigations, Assessment of organ damage, and Supportive treatment.
The findings from various clinical and follow up studies of those infected with SARS-CoV-2 are crucial in preventing further organ damage in ‘long COVID’. They are equally important for developing clinical guidelines for the care of survivors of COVID-19 afflicted with persistent and incapacitating symptoms. Presently, the physicians and medical communities are getting aware of long-hauler syndrome and the need of establishing post-COVID clinics with multidisciplinary and integrated approach is being realised. Further, the Neuro COVID-19 and Pulmo COVID-19 Clinics could be novel concepts for dealing with the ‘long COVID’ patients and offering them specialised care and follow up.
Approximately 10% of people experience prolonged illness after acute mild or severe COVID-19. Many such patients recover spontaneously with holistic support, rest, symptomatic treatment, and gradual increase in activity. Further specialised treatment is required for new, persistent, progressive, and newly emergent respiratory, cardiac, or neurological symptoms. As such the post-acute COVID-19 or ‘long COVID’ seems to be a multisystem disease and its management is largely based on limited clinical studies and requires a whole-patient perspective [40].
General treatment guidelines
➢ Respiratory symptoms: A degree of breathlessness is common during acute COVID-19 and convalescence. There could be worsening breathlessness and severe breathlessness may require hospitalization. In general, the breathlessness tends to improve with breathing exercises and guided pulmonary rehabilitation.
➢ Chest pain: Non-specific chest pain is common in post-acute COVID-19. It could be musculoskeletal, unexplained non-specific chest pain, or due to a cardiovascular condition.
➢ Thromboembolism: COVID-19 is an inflammatory and hypercoagulable state, with an increased risk of thromboembolic events. The hospitalised patients, in general, receive prophylactic anticoagulation but the recommendations for anticoagulant therapy after discharge vary. The high-risk patients are typically discharged with 10 days of extended thromboprophylaxis. Investigations and monitoring should follow during follow up.
➢ Ventricular dysfunction and cardiopulmonary complications: Left ventricular systolic dysfunction and heart failure can occur during post-COVID period. Intense cardiovascular exercise must be avoided for three months in all patients with myocarditis or pericarditis. During the follow up they are to be assessed for functional status, absence of dysrhythmias, and left ventricular systolic function.
➢ Mental health and wellbeing: Anxiety, stress, and symptoms related to social isolation are common. The post-COVID period is often associated with low mood, hopelessness, and insomnia. Post-traumatic stress disorder may occur and common in healthcare workers.
➢ The older patient: In general, COVID-19 tends to affect older patients more severely. Post-COVID-19 chronic pain and other general symptoms are frequent. The elderly patients, in addition, are more prone to risk of sarcopenia and malnutrition. Depression and delirium in elderly may mask neurodegenerative disorders like Alzheimer’s disease.
Investigations during ‘long COVID’ follow up
➢ Blood tests - Anaemia should be excluded. Lymphopenia is a feature of severe, acute COVID-19 illness, whereas leucocytosis may denote infection or inflammatory response.
➢ The elevated biomarkers may include C reactive protein, natriuretic peptides in heart failure, ferritin indicative of inflammation and continuing prothrombotic state, troponin suggestive of acute coronary syndrome or myocarditis and D-dimer indicating thromboembolic disease.
➢ A chest X-ray at 12 weeks and referral for new, persistent, or progressive symptoms. Cardiac echo, CT scan chest or MR scan may be required.
➢ Further studies and research are likely to refine the indications and interpretation of diagnostic and monitoring tests in follow-up of ‘long COVID’.
Supportive treatment and rehabilitation of ‘Long COVID’
The ‘long COVID’ syndrome has multi-system involvement and unpredictable course with variable presentation depending on known unmodifiable factors such as race, age and sex, and modifiable factors like comorbidities and lifestyle, and certain unknown factors. Following clinical and investigational assessment, the patients should be managed according to their clinical manifestations, extent of organ damage and associated complications.
Planning Careful resumption of physical activity: As highlighted earlier, apart from the severe cases, even those who suffer with mild disease, a proportion of people from all age groups face a prolonged recovery, particularly in relation to the physical activity [41]. Moreover, there is increasing recognition of potential long-term symptoms and complications of ‘long COVID’, including the enduring malaise and asthenia, cardiopulmonary disease, and psychological sequelae in some people. In this respect, though the current state of understanding of recovery from COVID-19 is limited, the ongoing research has highlighted several key concerns such as the potential for cardiac injury, including post-COVID myocarditis and cardiomyopathy.
Without evidence from robust studies, the current guidelines are based on clinical experience and consensus. A pragmatic approach is recommended for a gradual return to physical activity to mitigate associated risks. In general, all the COVID-19 patients should be risk stratified following recovery before recommending a return to physical activity, which should be gradual, individualized, and based on subjective tolerance of the activity. In general, a return to physical activity should be after at least seven days period free of symptoms, followed by two weeks of minimal exertion. As a rule, those with ongoing symptoms or history of severe COVID-19 need cardio-pulmonary assessment before advising return to physical activity [42].
Post-COVID Myocarditis and Cardiomyopathy: Most of our data on post-COVID cardiac injury is from patients with severe disease who were hospitalized. This cannot be extrapolated to those who have suffered with mild illness. As such, the incidence of cardiac injury in those with asymptomatic or mild to moderate disease is not known. Cardiac symptoms during illness such as chest pain, palpitations, syncope, severe breathlessness, need assessment for myocarditis and cardiomyopathy, followed by restriction of physical activity and periodic assessment. People who did not require hospital treatment but who had symptoms during their illness suggestive of myocardial injury, such as chest pain, severe breathlessness, palpitations, symptoms or signs of heart failure, or syncope and pre-syncope, should be assessed with a physical examination and considered for further investigations. Both European and US guidelines advocate restrictions on exercise for three to six months in cases of myocarditis confirmed by cardiac magnetic resonance imaging or endomyocardial biopsy.
In a study of in unselected patients who were followed with serum troponin measurements and cardiovascular magnetic resonance imaging after a diagnosis of COVID-19, it was documented that a significant number of patients suffered with ongoing myocardial inflammation several weeks after the diagnosis [30]. The cardiac MR in these patients recently recovered from COVID-19 infection, indicated cardiac involvement in 78% patients and ongoing myocardial inflammation in 60% patients, independent of pre-existing conditions, severity and overall course of the acute illness, and time from the original diagnosis. The study, thus, outlines the need for investigations for cardiovascular involvement and prudence during the convalescent period in advising exercise and return to physical activity.
Post-COVID Thromboembolic Complications: Pulmonary embolism is associated with COVID-19. Its long-term effects on pulmonary function are not currently known, but the previous relating to the SARS epidemic suggest persistent impairments in pulmonary function and exercise capacity in survivors. An early resumption of physical activity and exercise in the presence of pulmonary dysfunction may be associated with increased morbidity and mortality. Those with respiratory symptoms such as persistent cough and breathlessness are expected to resolve after several weeks, but the progressive, non-resolving or worsening symptoms may indicate pulmonary-vascular complications such as pulmonary embolism, concomitant pneumonia, or post-inflammatory bronchoconstriction and need full cardiopulmonary assessment.
The ‘brain fog’ and psychiatric symptoms: The ‘brain fog’ and various psychological sequelae include post-traumatic stress disorder, anxiety, and depression, and psychiatric disorders phenomena, such as psychosis in the post-COVID period. The exercise and physical activity can have beneficial as well as harmful effects. Hence the resumption of exercise and physical activity should be closely monitored.
Activity level and occupational rehabilitation: In the natural course of COVID-19, deterioration signifying severe infection usually occurs following a week from symptoms onset. This being the basis of consensus, a return to regular occupational activity, exercise or sporting activity should only occur after a symptom-free period of at least seven days. Further, risk-stratification approach is recommended to maximise safety and mitigate risks.
Thus, in practice, for those with mild symptoms during the COVID illness and asymptomatic during convalescence period, there should be a phased return to physical activity with at least a week in between every phase (Figure 5).
Figure 5: The phases of physical activity and exercise.
The phases have been outlined as - Phase 1: Breathing exercises, mild stretching, and gentle walking. Phase 2: Low intensity walking, mild household and gardening tasks, light yoga. Phase 3: Moderate intensity aerobic and strength challenge. Phase 4: Moderate intensity aerobic and strength challenge with coordination and functioning skills. Phase 5: Return to regular exercise and physical activity pattern. Usually, a light intensity activity is advised for initial two weeks. The Borg Rating of Perceived Exertion (RPE) scale is a subjective assessment of activity and physical work and is helpful in guiding the progress through the phases of increasing physical activity. The patients must rate their subjective feeling of exertion, including shortness of breath and fatigue, on a scale from 6 (no exertion at all) to 20 - maximal exertion [43].
Long COVID’s prognostic challenges
In general, levels of physical activity and exercise vary substantially across society. There are various contributing factors in the background and include cultural mores, prevailing concepts of gender, occupational demands, availability of time and cost, access and awareness for physical activity or exercise. As relates to the ‘long COVID’ syndrome, the inequalities in physical activity have impact on manifestation of various symptoms. In turn, the overall effect of ongoing ‘long COVID’ symptoms on the patient’s life need to be evaluated.
As apparent, the ‘long COVID’ afflictions are more common than realised earlier. It has been documented in a large survey involving 8200 participants that around one in five COVID-19 patients, continue to have symptoms 5 weeks later, and around one in ten after 12 weeks after infection [44]. According to the National Institute for Health and Care Excellence (NICE) guideline the patients are likely to have ongoing, symptomatic COVID-19 if they present with symptoms 4 to 12 weeks after the start of acute symptoms and have ‘long COVID’ if they still present with symptoms after 12 weeks [45].
Many of those who have suffered with severe COVID-19 may continue to have distressing symptoms, including breathlessness, anxiety, and chronic fatigue. Symptoms can
escalate among patients with co-morbid conditions. Symptomatic or palliative therapy may be an important aspect of overall care [46]. The relief of incapacitating symptoms through provision of holistic care, is another essential component of healthcare for ‘long COVID’ patients. Further, there is a scope for anticipatory approach to symptomatic management of these patients [47]. The distressing ‘long COVID’ symptoms are further accentuated by isolation and separation from loved ones, and the anxiety concerning the illness and fear of grave prognosis. The persistent symptoms among COVID-19 survivors pose new challenges to the healthcare providers and may be suitably managed with a combination of pharmacological and non-pharmacological treatments [48].
With the realization of ‘long COVID’ as a disease entity, the post-COVID-19 care centers are opening at various academic medical centers in the UK, the United States, and elsewhere. They aim to bring together the multidisciplinary teams to provide a comprehensive treatment and coordinated care. The US National Institutes of Health have provided interim guidelines for the medical management of persistent symptoms or illness after recovery from acute COVID-19 [49]. The guidelines and perspective about the overall management of ‘long COVID’ patients will witness ongoing revisions as new information emerges from research and clinical studies.
- Max Planck Institute for the Science of Human History. COVID-19 is here to stay for the foreseeable future: Future of field-based sciences in the time of coronavirus. ScienceDaily. ScienceDaily, 14 September 2020. www.sciencedaily.com/releases/2020/09/200914112206.htm.
- Nikhra V. Exploring COVID-19: Relating the Spike Protein to Infectivity, Pathogenicity, and Immunogenicity. Research Gate. 2021.
- Oran DP, Topol EJ. The Proportion of SARS-CoV-2 Infections That Are Asymptomatic. Ann Internal Med. 2021.
- Pollitt KJG, Peccia J, Ko AI, Kaminski N, Cruz CSD, et al. COVID-19 vulnerability: the potential impact of genetic susceptibility and airborne transmission. Human Genomics. Hum Genomics. 2020; 14: 17. PubMed: https://pubmed.ncbi.nlm.nih.gov/32398162/
- Murray MF, Kenny EE, Ritchie MD, Rader DJ, Bale AE, et al. COVID-19 outcomes and the human genome. Gen Med. 2020; 22: 1175–1177. PubMed: https://pubmed.ncbi.nlm.nih.gov/32393819/
- Wu BB, Gu DZ, Yu JN, Yang J, Shen WQ. Association between ABO blood groups and COVID-19 infection, severity and demise: A systematic review and meta-analysis. Infect Genet Evol. 2020; 84: 104485. PubMed: https://pubmed.ncbi.nlm.nih.gov/32739464/
- Nguyen A, David JK, Maden SK. Human Leukocyte Antigen Susceptibility Map for Severe Acute Respiratory Syndrome Coronavirus 2. J Virol. 2020; 94: e00510-20.
- Project Leader Dr Helen Su, National Institute of Allergy and Infectious Diseases (NIAID)/National Institutes of Health (NIH), Bethesda, USA and Co-leader Dr Jean-Laurent Casanova, The Rockefeller University, Howard Hughes Medical Institute (HHMI), New York, USA and Necker Hospital for Sick Children & INSERM, Paris, France. https://www.COVIDhge.com
- Carfì A, Bernabei R, Landi F. Gemelli against COVID-19 Post-Acute Care Study Group. Persistent Symptoms in Patients After Acute COVID-19. JAMA. 2020; 324: 603-605. PubMed: https://pubmed.ncbi.nlm.nih.gov/32644129/
- Godlee F. Editors’s Choice - Living with COVID-19. BMJ. 2020; 370: m3392.
- del Rio C, Collins LF, Malani P. Long-term health consequences of COVID-19. JAMA. 2020. PubMed: https://pubmed.ncbi.nlm.nih.gov/33031513/
- Sudre CH, Murray B, Varsavsky T, et al. Attributes and predictors of Long-COVID: analysis of COVID cases and their symptoms collected by the COVID Symptoms Study App. medRxiv and bioRxiv. 2020.
- Cellai M, O’Keefe JB. Characterization of prolonged COVID-19 symptoms and patient comorbidities in an outpatient telemedicine cohort. medRxiv and bioRxiv. 2020.
- Huang C, Huang L, Wang Y, Li X, Ren L, et al. 6-month consequences of COVID-19 in patients discharged from hospital: a cohort study. Lancet. 2021; 397: 220-232. PubMed: https://pubmed.ncbi.nlm.nih.gov/33428867/
- Weerahandi H, Hochman KA, Simon E, Blaum C, Chodosh J, et al. Post-discharge health status and symptoms in patients with severe COVID-19. Preprint. medRxiv. 2020; 2020; 08.11.20172742. PubMed: https://pubmed.ncbi.nlm.nih.gov/32817973/
- Davis HE, Assaf GS, McCorkell Ll. Characterizing Long COVID in an International Cohort: 7 Months of Symptoms and Their Impact. medRxiv preprint. 2020.
- Otte MS, Klussmann JP, Luers JC. Persisting olfactory dysfunction in patients after recovering from COVID-19. J Infect. 2020. 81: e58. PubMed: https://pubmed.ncbi.nlm.nih.gov/32592702/
- Paderno A, Mattavelli D, Rampinelli V, Grammatica A, Raffetti E, et al. Olfactory and Gustatory Outcomes in COVID-19: A Prospective Evaluation in Non-hospitalized Subjects. Otolaryngol Head Neck Surg. 2020; 163: 1144-1149. PubMed: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7331108/
- Carvalho-Schneider C, Laurent E, Lemaignenet A, Beaufils E, Bourbao-Tournois C, et al., Follow-up of adults with noncritical COVID-19 two months after symptom onset. Clin Microbiol Infect. 2020; S1198-743X(20)30606-6. PubMed: https://pubmed.ncbi.nlm.nih.gov/33031948/
- Wise J. COVID-19: Symptoms are common after acute phase of disease, Italian study shows. BMJ. 2020; 370: m2804. PubMed: https://pubmed.ncbi.nlm.nih.gov/32651164/
- Ngai JC, Ko FW, Ng SS, Kin-Wang T, Tong M, et al. The long-term impact of severe acute respiratory syndrome on pulmonary function, exercise capacity and health status. Respirology. 2010; 15: 543-550. PubMed: https://pubmed.ncbi.nlm.nih.gov/20337995/
- Fraser E. Long term respiratory complications of COVID-19. BMJ. 2020; 370: m3001. PubMed: https://pubmed.ncbi.nlm.nih.gov/32747332/
- Huang Y, Tan C, Wu J, Chen M, Wang Z, et al. Impact of coronavirus disease 2019 on pulmonary function in early convalescence phase. Respir Res. 2020; 21: 163. PubMed: https://pubmed.ncbi.nlm.nih.gov/32600344/
- Salehi S, Abedi A, Balakrishnan S, Gholamrezanezhad A. Coronavirus disease 2019 (COVID-19) imaging reporting and data system (COVID-RADS) and common lexicon: a proposal based on the imaging data of 37 studies. Eur Radiol. 2020; 30: 4930-4942. PubMed: https://pubmed.ncbi.nlm.nih.gov/32346790/
- Zhao YM, Shang YM, Song WB, Qing-Quan L, Xie H, et al. Follow-up study of the pulmonary function and related physiological characteristics of COVID-19 survivors three months after recovery. eClinicalMedicine. 2020; 100463.
- Marshall M. The lasting misery of coronavirus long-haulers. Nature. 2020; 585: 339-341. PubMed: https://pubmed.ncbi.nlm.nih.gov/32929257/
- The prospective follow-up study of patients infected with the coronavirus, presented at the European Respiratory Society International Congress. 2020. https://www.ersnet.org/the-society/news/COVID-19-patients-suffer-long-term-lung-and-heart-damage-but-it-can-improve-with-time
- Leulseged TW, Hassen IS, Edo MG, et al. Duration of Supplemental Oxygen Requirement and Predictors in Severe COVID-19 Patients in Ethiopia: A Survival Analysis. medRxiv preprint. 2020.
- Zhang P, Li J, Liu H, Han N, Ju J, et al. Long-term bone and lung consequences associated with hospital-acquired severe acute respiratory syndrome: a 15-year follow-up from a prospective cohort study. Bone Res. 2020; 8: 34.
- Puntmann VO, Carerj ML, Wieters I, Fahim M, Arendt C, et al. Outcomes of cardiovascular magnetic resonance imaging in patients recently recovered from coronavirus disease 2019 (COVID-19). JAMA Cardiol. 2020; 5: 1265-1273. PubMed: https://pubmed.ncbi.nlm.nih.gov/32730619/
- Sardari A, Tabarsi P, Borhany H, Mohiaddin R, Houshmand G. Myocarditis detected after COVID-19 recovery. Eur Heart J Cardiovasc Imaging. 2021; 22: 131-132. PubMed: https://pubmed.ncbi.nlm.nih.gov/32462177/
- Li B, Yang J, Zhao F, Zhi L, Wang X, et al. Prevalence and impact of cardiovascular metabolic diseases on COVID-19 in China. Clin Res Cardiol. 2020; 109: 531-538. PubMed: https://pubmed.ncbi.nlm.nih.gov/32161990/
- Long B, Brady WJ, Koyfman A, Gottlieb M. Cardiovascular complications in COVID-19. Am J Emerg Med. 2020; 38: 1504-1507. PubMed: https://pubmed.ncbi.nlm.nih.gov/32317203/
- Eiros R, Barreiro-Perez M, Martin-Garcia A. Pericarditis and myocarditis long after SARS-CoV-2 infection: a cross-sectional descriptive study in health-care workers. medRxiv and bioRxiv preprint. 2020.
- Varatharaj A, Thomas N, Ellul MA, Davies NWS, Pollak TA, et al. CoroNerve Study Group. Neurological and neuropsychiatric complications of COVID-19 in 153 patients: a UK-wide surveillance study. Lancet Psychiatry. 2020; 7: 875-882. PubMed: https://pubmed.ncbi.nlm.nih.gov/32593341/
- Meppiel E, Peiffer-Smadja N, Maury A, Bekri I, Delorme C, et al. Neurologic manifestations associated with COVID-19: a multicentre registry. Clin Microbiol Infect. 2020. PubMed: https://pubmed.ncbi.nlm.nih.gov/33189873/
- Lyons D, Frampton M, Naqvi S, Donohoe D, Adams G, Glynn K. Fallout from the COVID-19 pandemic - should we prepare for a tsunami of post viral depression? Ir J Psychol Med. 2020; 37: 295-300. PubMed: https://pubmed.ncbi.nlm.nih.gov/32408926/
- Varga Z, Flammer AJ, Steiger P, Haberecker M, Andermatt R, et al. Endothelial cell infection and endothelitis in COVID-19. Lancet. 2020; 95: 1417-1418. PubMed: https://pubmed.ncbi.nlm.nih.gov/32325026/
- Xiong TY, Redwood S, Prendergast B, Chen M. Coronaviruses and the cardiovascular system: acute and long-term implications. Eur Heart J. 2020; 41: 1798-1800. PubMed: https://pubmed.ncbi.nlm.nih.gov/32186331/
- Greenhalgh T, Knight M, A’Court C, Buxton M, Husain L, et al. Management of post-acute COVID-19 in primary care. BMJ. 2020; 370: m3026. PubMed: https://pubmed.ncbi.nlm.nih.gov/32784198/
- Salman D, Vishnubala D, Le Feuvre P, Beaney T, Korgaonkar J, et al. Returning to physical activity after COVID-19. BMJ. 2021; 372: m4721. PubMed: https://pubmed.ncbi.nlm.nih.gov/33419740/
- Tenforde MW, Kim SS, Lindsell CJ, et al. Symptom duration and risk factors for delayed return to usual health among outpatients with COVID-19 in a multistate health care systems network-United States, March-June 2020. MMWR Morb Mortal Wkly Rep. 2020; 69: 993-998.
- Williams N. The Borg Rating of Perceived Exertion (RPE) scale. Occup Med. 2017; 67: 404-405.
- Nabavi N. COVID-19: Consider overall impact of long COVID symptoms when deciding whether to refer, says NICE. BMJ. 2020; 371: m4915.
- National Institute for Health and Care Excellence. COVID-19 rapid guideline: managing the long-term effects of COVID-19. 2020. www.nice.org.uk/guidance/ng188.
- Ting R, Edmonds P, Higginson IJ, Sleeman KE. Palliative care for patients with severe COVID-19. BMJ. 2020; 370: m2710. PubMed: https://pubmed.ncbi.nlm.nih.gov/32665316/
- Greenhalgh T, Knight M, A’Court C, Buxton M, Husain L, et al. Management of post-acute COVID-19 in primary care. BMJ. 2020; 370: m3026. PubMed: https://pubmed.ncbi.nlm.nih.gov/32784198/
- Halpin, SJ, McIvor, C, Whyatt, G, Adams A, Harvey O, et al. Postdischarge symptoms and rehabilitation needs in survivors of COVID-19 infection: A cross-sectional evaluation. J Med Virol. 2021; 93: 1013-1022. PubMed: https://pubmed.ncbi.nlm.nih.gov/32729939/
- Late Sequelae of COVID-19. 2020. https://www.cdc.gov/coronavirus/2019-ncov/hcp/clinical-care/late-sequelae.html