More Information
Submitted: 06 May 2020| Approved: 22 May 2020 | Published: 25 May 2020
How to cite this article: Najar KA, Amin A, Ommid M. Anaesthetic management of an elderly patient with ischaemic heart disease and previous MI undergoing elective inguinal hernia repair: Case report. Int J Clin Anesth Res. 2020; 4: 001-003.
DOI: 10.29328/journal.ijcar.1001013
Copyright License: © 2020 Najar KA, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Ischemic heart disease; Perioperative medicine; Spinal anaesthesia; Non-cardiac surgery
Anaesthetic management of an elderly patient with ischaemic heart disease and previous MI undergoing elective inguinal hernia repair: Case report
Khaleel Ahmad Najar1*, Anka Amin2, Mohammad Ommid3
(¹Senior Resident, ²Assistant Professor, ³Associate Professor)
1Department of Anaesthesiology, Government Medical College, Srinagar, UT of J&K, India
2Department of Anaesthesiology, Government Medical College, Srinagar, UT of J&K, India
3Department of Anaesthesiology, Government Medical College, Srinagar, UT of J&K, India
*Address for Correspondence: Najar KA, Senior Resident, Department of Anaesthesiology, Government Medical College, Srinagar, UT of J&K, India, Email: ka6915369@gmail.com
Ischemic heart disease may occur in isolation, or in combination with the pathological process of vascular ageing, arteriosclerosis. These two conditions have differing impacts on the haemodynamic changes in response to anaesthesia and surgery. Hypertension is not a feature of ischemic heart disease, and vice versa, but where the two conditions co-exist, hypertension aggravates and accelerates the pathological processes of ischemic heart disease. Patients older than 40 yrs. presenting for anaesthesia and surgery must therefore be considered at risk of any combination of these three conditions. Anaesthetic techniques must also be chosen to minimize haemodynamic changes which in the normal healthy patient cause no serious morbidity, but which, in the patient with ischemic heart disease, can lead to serious morbidity or death. Here we report a 70 years old (BMI of 23.3) elderly, hypertensive Male patient with ischemic heart disease with previous MI (EF of 40% - 5%) undergoing elective Inguinal hernia repair. We Opted Spinal anesthesia over General anaesthesia as it should be an asset in cardiac patients undergoing non-cardiac lower abdominal surgeries to reduce preload and after load, stress response, coagulation responses, improves coronary perfusion, provides better postoperative analgesia, reduces incidence of perioperative MI, maintains myocardial oxygen supply demand ratio and avoids harmful effects of GA such as hypotention due to intravenous induction drugs, tachycardia and hypertension due to pressor response during direct laryngoscopy and tracheal intubation.
Patients with Ischemic heart disease undergoing non-cardiac surgery are at an increased risk for peri-operative complications such as myocardial ischaemia, MI, cardiac failure, arrhythmias, cardiac arrest and increased morbidity and mortality. These complications are much higher in patients with recent MI or unstable angina who require urgent or emergency cardiac surgery [1,2]. Ischemic heart disease may occur in isolation, or in combination with the pathological process of vascular ageing, arteriosclerosis. These two conditions have differing impacts on the haemodynamic changes in response to anaesthesia and surgery. Hypertension is not a feature of ischemic heart disease, and vice-versa, but where the two conditions co-exist, hypertension aggravates and accelerates the pathological processes of ischemic heart disease. Patients older than 40 yrs. presenting for anaesthesia and surgery must therefore be considered at risk of any combination of these three conditions. Aside from risk stratification and functional capacity evaluation, cardiac assessment includes measuring biomarkers, performing noninvasive and invasive test of cardiac status. Anaesthetic techniques must also be chosen to minimize haemodynamic changes which in the normal healthy patient cause no serious morbidity, but which, in the patient with ischemic heart disease, can lead to serious morbidity or death.
A seventy year old, elderly male patient posted for an elective right sided inguinal hernia repair. His Pre-anaesthetic evaluation reveals that he was a known case of Hypertension on Tab. Enalapril (10 mg od) since eight years and Type 2 DM on Tab. Glimepiride (with Insulin) since nine years. Both hypertension and DM were well controlled. Patient complains of breathlessness on exertion (NYHA class II) and has a predicted METs score of ≥ 4. There is a past history of hospital admission four years back for documented Inferior wall MI (managed conservatively) after which patient had undergone Coronary Angiography (findings: mid RCA -50% lesion, LAD/LCX Plaquing) and was on Tab Metoprolol (25 mg) once daily and Tab clopidogrel (75 mg) once daily as secondary prophylaxis treatment.
On physical examination, Patient was well built, well-nourished with a body weight of 47 kgs., a pulse rate of 86 bpm, BP of 128/80 mmhg. Airway examination reveals adequate mouth opening (Mallampatti grade-I) with normal neck mobility and normal dentition. Spine examination was also normal. Clinical examination of Cardiovascular and Respiratory systems was unremarkable.
Laboratory investigations included complete blood count with hemoglobin levels of 14.6g% and platelet count of 1.78 lacs/mm³. Liver function, kidney function, serum electrolytes, coagulation profile and blood sugar levels were also normal. Chest radiograph was normal and 12-lead ECG showed normal sinus rhythm and no significant ST/T wave changes. Echocardiography revealed RCA territory akinesia, mild left ventricular systolic dysfunction with an ejection fraction of 40% - 45% and mild MR.
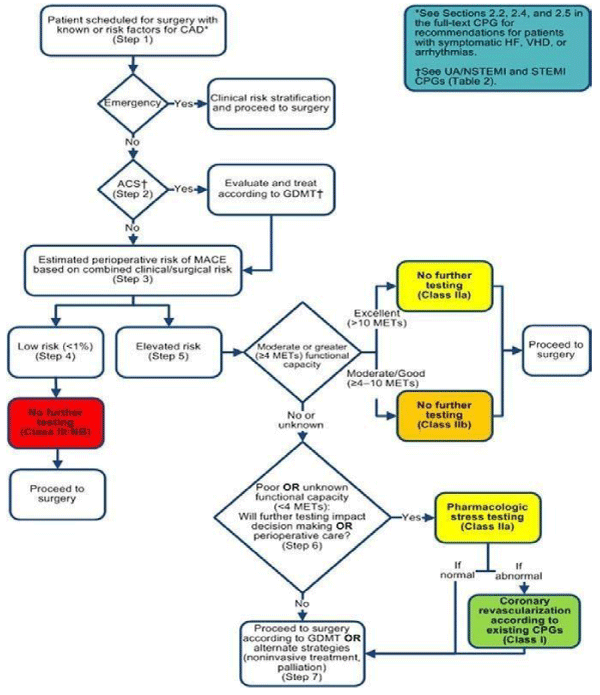
Patient was labelled as high risk procedure (calculated RCRI of ≥ 2) with an elevated risk of adverse perioperative cardiac outcome (predicted MACE of 6.6%) (Figure 1).
Figure 1: Fleisher LA. Circulation. 2014 ACC/AHA Guideline on Perioperative Cardiovascular Evaluation and Management of Patients Undergoing Noncardiac Surgery: Executive Summary. Volume: 130, Issue: 24, Pages: 2215-2245.
Anaesthetic management
Patient was classified as ASA III and high risk consent was taken. Patient preferred regional anaesthesia after the risk benefit ratio of General and regional anaesthesia was explained to him. Clopidogrel was stopped 5 days before surgery and Glimepiride 24 hours before surgery. Two thirds of usual Insulin (NPH) dose was given the night before surgery and morning dose withheld on the day of surgery. ACEi (Enalapril) and Beta-blockers (Metoprolol) were continued in the perioperative period.
On the day of surgery, fasting status was confirmed and necessary investigations blood sugar (F) of 99 mg/dl, Platelet count of 1.78 lacs/mm³, Na+ (134 mg/dl), K+ (3.4 mg/dl) and coagulation (PT/INR of 12.2/1.06) were checked. Standard monitoring included 5 lead ECG (including II, V5 ischemia sensitive), Pulse oximetry and non-invasive Blood Pressure (NIBP). Pre-operative baseline vitals (HR-85 bpm, BP-134/82 mmHg and SpO2-97% on room air) were recorded and an I/V line was established. Inj. Pantoprazole 40 mg was given I/V and patient was preloaded with 500ml of 0.9% NS (8 ml/kg).
Spinal anaesthesia was performed under all asceptic precautions, in sitting position; Skin was infiltrated with 2% plain xylocaine at L3-L4 intervertebral disc space and with a 25G Quincke spinal needle, subarachnoid space was entered. Inj. Bupivacaine 10 mg with fentanyl 25 ug was injected into the subarachnoid space after free flow of CSF. Patient was laid supine and spread of the block was monitored by pinprick testing. A slight head-up position, guided by the curvature of the patient´s spine, helped to achieve the desired sensory and motor block level (below T6). Inj. Midazolam (1 mg) was given intravenously and Oxygen administered intraoperatively via Venti Mask. Vitals were recorded every three minutes for first 15 minutes and every 5 minutes thereafter. Systolic blood pressure remained between 110 and 130 mmhg, diastolic blood pressure between 70 and 80 mmHg and Heart rate between 60 and 90 bpm throughout the procedure. Inj. Ondansetron (4 mg) was given at the end of surgery. The patient remained hemodynamically stable throughout the procedure and Surgery was completed uneventfully. Duration of surgery was 80 minutes and total intravenous fluid given intraoperatively was one litre.
Postoperatively, SpO2, non-invasive blood pressure and ECG monitoring with oxygen supplementation by ventimask were performed in the recovery room. Inj paracetamol was given as rescue analgesic in the postoperative period. A cardiology review was sought for reinstitution of antiplatelet therapy. Beta-blockers and antihypertensives were continued in the postoperative period and Patient was discharged home on first postoperative day.
The primary goal of the anaesthetic management of a patient with ischaemic heart disease undergoing non-cardiac surgery is the avoidance of myocardial ischaemia. Anything which increases cardiac stress such as physical work, emotional stress, anaesthesia and surgical procedures simultaneously increase myocardial oxygen demand which is compensated in normal individuals by increasing coronary blood flow. This is not so in patients with IHD where coronary flow is already compromised. Therefore, all anaesthetic techniques must aim to keep myocardial oxygen supply greater than demand and thus avoid ischaemia. The essential requirements are avoiding tachycardia and extremes of blood pressure, both of which adversely affect myocardial oxygen supply and demand ratio [3].
General or regional anaesthesia can be chosen alone or in combination as part of a balanced technique depending on the surgery and patient requirements. The combination of general and regional anaesthesia may cause greater cardiovascular instability than either technique alone. The benefits of neuraxial anaesthetic techniques (spinal or epidural) over General include reduction of preload and after load, stress response, coagulation responses, coronary vasodilation, improved postoperative analgesia, reduced incidence of perioperative MI and avoidance of harmful effects of GA such as hypotention due to intravenous induction drugs, tachycardia and hypertension due to pressor response during direct laryngoscopy and tracheal intubation. However, Sympathetic blockade due to neuraxial anaesthesia can lead to severe hemodynamic perturbations. Therefore, correction and management of arterial hypotension has been recently recommended [4]. Neuraxial anaesthesia alone (but not when associated with general anaesthesia) can therefore be considered as the anaesthetic technique of choice following careful assessment of the risk/benefit ratio for each patient [4].
Furthermore, there is a frequent association in cardiac patients of drugs that impede coagulation; complications can be tragic, so risk-benefit ratio should be calculated while choosing neuraxial anaesthesia. A 2014 review of nine systematic reviews of randomized controlled clinical trials summarises the outcome of neuraxial analgesia with or without general anaesthesia versus general anaesthesia alone in patients undergoing any type of surgery. In comparison with General anaesthesia use of neuraxial blockade alone reduces 0-30 day mortality and decreases the risk of pneumonia [5].
We conclude that Regional anaesthesia can be an alternative over General for anaesthetic management of patients with ischemic heart disease undergoing lower abdominal non-cardiac surgical procedures as it reduces stress response to surgery, avoids the cardiodepressant effects of induction drugs, coagulation responses, tachycardia and hypertension due to pressor response due to laryngoscopy and tracheal intubation, improved postoperative analgesia and reduced incidence of perioperative MI.
The authors are very thankful to Prof. (Dr.) Rukhsana Najeeb, Professor and Head, Department of Anaesthesiology, Govt. Medical College, Srinagar (Jammu and Kashmir, India).
- Fleisher LA, Fleischmann KE, Auerbach AD, Barnason SA, Beckman JA, et al. 2014 ACC/AHA guideline on perioperative cardiovascular evaluation and management of patients undergoing noncardiac surgery: Executive summary: A report of the American College of Cardiology/American Heart Association task force for on practice guidelines. Circulation. 2014; 130: 2215–2245. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/25085962
- Kristensen SD, Knuuti J. New ESC/ESA Guidelines on non-cardiac surgery: Cardiovascular assessment and management. Eur Heart J. 2014; 35: 2344. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/25086026
- Hedge J, Balajibabu PR, Sivaraman T. The patient with ischaemic heart disease undergoing non cardiac surgery. Indian J Anaesth. 2017; 61: 705–711. PubMed: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5613595/
- Kristensen SD, Knuuti J, Saraste A, Anker S, Bøtker HE, et al. 2014 ESC/ESA Guidelines on non-cardiac surgery: cardiovascular assessment and management. The Joint Task Force on noncardiac surgery: cardiovascular assessment and management of the European Society of Cardiology (ESC) and the European Society of Anaesthesiology (ESA). Eur J Anaesthesiol. 2014; 31: 517-573. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/25086026
- Guay J, Choi P, Suresh S. Neuraxial blockade for the prevention of postoperative mortality and major morbidity: an overview of Cochrane Systemic Reviews. Cochrane Database Syst Rev. 2014: cd010108. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/24464831