More Information
Submitted: February 09, 2022 | Approved: April 04, 2022 | Published: April 05, 2022
How to cite this article: Gupta PD. Menstrual cycle effects on sleep. Clin J Obstet Gynecol. 2022; 5: 042-043.
DOI: 10.29328/journal.cjog.1001105
Copyright License: © 2022 Gupta PD. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Sleep status; Menstrual phases; Steroid hormones; Neurosteroids
Menstrual cycle effects on sleep
Gupta PD*
Former Director Grade Scientist, Centre for Cellular and Molecular Biology, Hyderabad, India
*Address for Correspondence: Gupta PD, Former Director Grade Scientist, Centre for Cellular and Molecular Biology, Hyderabad, India, Email: pdg2000@hotmail.com
Sleep and menstrual cycle both are normal physiological processes in women’s life but they are regulated by different centers. Sleep is a daily rhythm whereas the menstrual cycle lasts for 28 days. During this period the estrogen peaks twice. We have shown earlier that there is an inverse relationship between estrogen and the hormone melatonin which aids sleep. Because of this menstruating women will have sleep disorders.
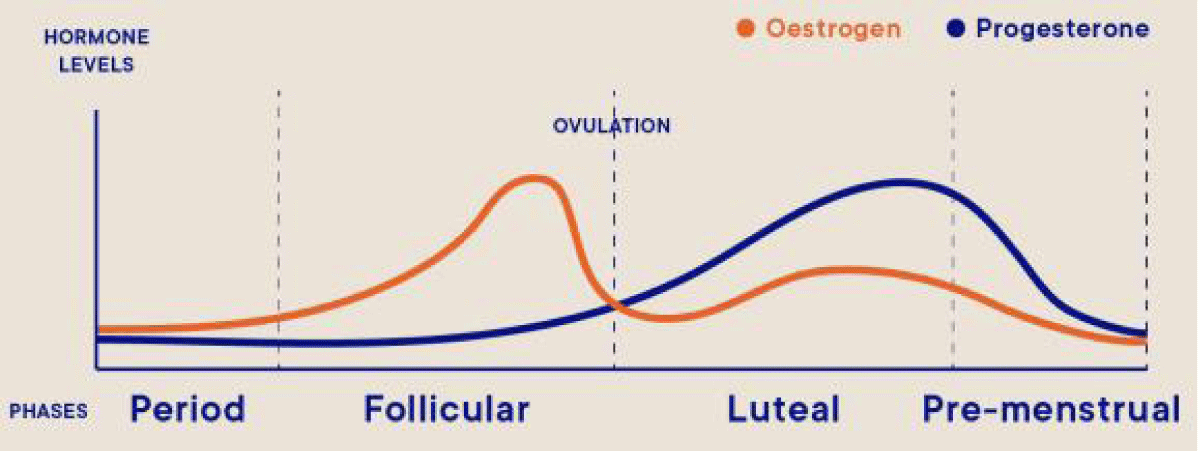
All human beings spend about one-third of their lifetime in sleep only. And it is essential too, without which it is difficult to manage our daily life. Due to sleep the brain and the body regain energy. Sleep is heavily influenced by circadian rhythms and by hormonal and environmental factors. Sleep performs a restorative function for the brain and body as evidenced by the myriad symptoms of metabolic dysfunction that result when animals or human beings are deprived of sleep [1]. Sleep provides essential support to the immune system [2]. Sleep is more commonly disrupted in women compared with men and is disrupted by the female hormonal milieu [3]. Estrogen levels rise and fall twice during the menstrual cycle (Figure 1).
Figure 1:
Estrogen levels rise during the mid-follicular phase and then drop precipitously after ovulation. This is followed by a secondary rise in estrogen levels during the mid-luteal phase with a decrease at the end of the menstrual cycle. By causing anxiety and depressed mood during the decline of estrogen that contributes to disrupted sleep
Further, the awake and sleep cycle is influenced by various internal (physiological) and external factors. Perhaps the greatest influence is the exposure to light which influences the hormonal milieu. Specialized cells in the retinas of the eyes process light and tell the brain whether it is day or night and can advance or delay our sleep-wake cycle. Exposure to light can make it difficult to fall asleep and return to sleep when awakened. It is due to the fact that melatonin, the hormone that aids sleep is synthesized only in the dark [4]. We have shown earlier that there is an inverse relationship between estrogen and the hormone melatonin which aids sleep [5]. It is now well established that sleep and the endocrine system have a bidirectional relationship that depends on each other to regulate different physiological processes including sleep.
Menstrual events
The anovulatory cycle has a circadian rhythm superimposed on the menstrual-associated rhythm (28 days cycle). The ovarian cycle consists of three phases: follicular (preovulatory) phase, ovulation, and luteal (postovulatory) phase, whereas the uterine cycle is divided into menstruation, proliferative (postmenstrual) phase, and secretary (premenstrual) phase [6].
Women’s menstrual cycle affects their circadian rhythm. The hormonal environment is a critical regulator of many physiologic processes, which significantly changes twice during the menstrual cycle. The menstrual cycle is regulated by the complex interaction of hormones: luteinizing hormone, follicle-stimulating hormone, and estrogen and progesterone. Estrogen levels rise during the mid-follicular phase and then drop precipitously after ovulation. This is followed by a secondary rise in estrogen levels during the mid-luteal phase with a decrease at the end of the menstrual cycle [7,8].
Sleep status during menstrual cycle
Studies of sleep across the life cycle in women were carried out by various investigators to investigate how prominent gynecological factors (regular/irregular menstrual cycle, premenstrual complaints, or menopause) can influence both subjective and objective sleep data by both survey and polysomnographic techniques. Subjective and objective sleep changes occur during the menstrual cycle. Poor sleep quality in the premenstrual phase and menstruation is common in women with premenstrual symptoms or painful menstrual cramps( dysmenorrheal) is significantly associated with and self-awareness of menstrual irregularity among healthy, young, ovulating, Chinese females [9,10].
Sleep is more disrupted in the luteal phase compared with the follicular phase in midlife women, whether or not they have an insomnia disorder. There is a prominent increase in sleep spindles and spindle frequency activity in the luteal phase, likely an effect of progesterone and/or its neuroactive metabolites acting on sleep regulatory systems. Luteal phase changes also include blunted temperature rhythm amplitude and reduced rapid eye movement sleep. Short sleep duration is associated with irregular menstrual cycles, which may impact reproductive health. The menstrual cycle phase and menstrual-related disorders should be considered when assessing women's sleep complaints [11,12]. Sleep disruption during pregnancy and postpartum is nearly universal, but effective and practical countermeasures are still needed.
Menopause is associated with insomnia due to several factors including hot flashes, mood disorders, and increased sleep-disordered breathing. In summary, much research is required to fully elucidate the impact of the life cycle on sleep parameters in women [13]. Compared to the follicular phase, in the post-ovulation luteal phase, body temperature is elevated, but the amplitude of the temperature rhythm is reduced. Evidence indicates that the amplitude of other rhythms, such as melatonin and cortisol, may also be reduced in the luteal phase. Subjective sleep quality is lowest around menses, but the timing and composition of sleep remain relatively stable across the menstrual cycle in healthy women, apart from an increase in spindle frequency activity and a minor decrease in rapid eye movement (REM) sleep during the luteal phase.
Disruption of circadian rhythms is associated with distur-bances in menstrual function. Female shift workers compared to non-shift workers are more likely to report menstrual irregularity and longer menstrual cycles [14].
Sleep disturbances are common during perimenopause, menopause, and postmenopause [15]. The menopausal decline of estrogen contributes to disrupted sleep by causing menopausal symptoms from hot flushes and sweats (vasomotor symptoms) to anxiety and depressed mood; anxiety leading to difficulty getting to sleep, and depression leading to non-restorative sleep and early morning wakening.
Furthermore, neurosteroids such as allopregnanolone and pregnenolone are involved in the generation of slow-wave sleep, the effect has been demonstrated in experimental animal studies. Thus we see that sleep and the endocrine system saved a bidirectional relationship that depends on each other to regulate different physiological processes including sleep. Further investigations into the biological consequences of circadian disruption in women will offer insight into some menstrual-associated disorders, including mood changes, as well as reproductive function, and possible links with breast cancer.
- Shepard JW Jr, Buysse DJ, Chesson AL Jr, Dement WC, Goldberg R, et al. History of the development of sleep medicine in the United States. J Clin Sleep Med. 2005; 1: 61-82. PubMed: https://pubmed.ncbi.nlm.nih.gov/17561617/
- Besedovsky L, Lange T, Born J. Sleep and immune function. Pflugers Arch. 2012; 463: 121-137. PubMed: https://pubmed.ncbi.nlm.nih.gov/22071480/
- Mallampalli MP, Carter CL. Exploring sex and gender differences in sleep health: a Society for Women's Health Research Report. J Womens Health (Larchmt). 2014; 23: 553-562. PubMed: https://pubmed.ncbi.nlm.nih.gov/24956068/
- Wright Jr KP, McHill AW, Birks BR, Griffin BR, Rusterholz T, et al. Entrainment of the human circadian clock to the natural light-dark cycle. Curr Biol. 2013; 23: 1554–1558. PubMed: https://pubmed.ncbi.nlm.nih.gov/23910656/
- Jagota A, Olcese J, Rao SH, Gupta PD. Pineal rhythms are synchronized to light–dark cycles in congenitally anophthalmic mutant rats. Brain Res. 1999; 825: 95–103. PubMed: https://pubmed.ncbi.nlm.nih.gov/10216177/
- Gupta PD, Iino A. Mothering A Cause. Capricorn Publishing House, Jaipur. India. 2010.
- Gupta PD. Menstrual Cycle and its Importance. Arch Reprod Med Sex Health. 2020; 3: 51-54.
- He H, Yu X, Chen T, Yang F, Zhang M, et al. Sleep Status and Menstrual Problems among Chinese Young Females. Biomed Res Int. 2021; 1549712. PubMed: https://pubmed.ncbi.nlm.nih.gov/34734080/
- Hachul H, Andersen ML, Bittencourt LRA, Santos-Silva R, Conway SG, et al. Does the reproductive cycle influence sleep patterns in women with sleep complaints? Climacteric. 2010; 13: 594-603. PubMed: https://pubmed.ncbi.nlm.nih.gov/20001564/
- de Zambotti M, Willoughby AR, Sassoon SA, Colrain IM, Baker FC. Menstrual Cycle-Related Variation in Physiological Sleep in Women in the Early Menopausal Transition. J Clin Endocrinol Metab. 2015; 100: 2918-2926. PubMed: https://pubmed.ncbi.nlm.nih.gov/26079775/
- Baker FC, Lee KA. Menstrual Cycle Effects on Sleep Sleep Med Clin. 2018; 13: 283-294. PubMed: https://pubmed.ncbi.nlm.nih.gov/30098748/
- Moline ML, Broch L, Zak R, Gross V. Sleep in women across the life cycle from adulthood through menopause Sleep Med Rev. 2003; 7: 155-77. PubMed: https://pubmed.ncbi.nlm.nih.gov/12628216/
- Lawson CC, Whelan EA, Lividoti Hibert EN, Spiegelman D, Schernhammer ES, et al. Rotating shift work and menstrual cycle characteristics. Epidemiology. 2011; 22: 305-312. PubMed: https://pubmed.ncbi.nlm.nih.gov/21364464/
- Jehan S, Masters-Isarilov A, Salifu I, Zizi F, Jean-Louis G, et al. Sleep Disorders in Postmenopausal Women. J Sleep Disord Ther. 2015; 4: 212.
- George O. Neurosteroids and cholinergic systems: implications for sleep and cognitive processes and potential role of age-related changes Psychopharmacology (Berl). 2006; 186: 402-413.