More Information
Submitted: 17 April 2020 | Approved: 27 April 2020 | Published: 29 April 2020
How to cite this article: Ogundele MO. Influence of adverse socio-emotional risk factors on the physical and mental health needs of children and young people in public care of a South-West England local authority. Clin J Nurs Care Pract. 2020; 4: 001-009.
DOI: 10.29328/journal.cjncp.1001021
Copyright License: © 2020 Ogundele MO, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Looked-after children; Integrated services; Mental health; Physical health; Adverse child experience; Fostering; Adoption
Abbreviations: Adoption Health Assessment (AHA); Adverse Childhood Experiences (ACE); British Association for Adoption and Fostering (BAAF); Children and Young People (CYP); Review Adoption Health Assessment (RAHA); Looked-After Children and Young People (LACYP); North Somerset Local Authority (NSLA); Initial Health Assessments (IHA)
Influence of adverse socio-emotional risk factors on the physical and mental health needs of children and young people in public care of a South-West England local authority
Michael O Ogundele*
Children’s Services, Weston Area NHS Trust, Drove House, Drove Road, Weston-Super-Mare, BS23 3NT, UK
*Address for Correspondence: Michael O Ogundele, Consultant Pediatrician, Medical Adviser and Designated Doctor for Looked After Children, Weston Area NHS Trust, North Somerset Local Authority, Drove House, Drove Road, Weston-Super-Mare, BS23 3NT, United Kingdom Tel: 01934 88 1340; Email: Michael.Ogundele1@nhs.net
Introduction: There is increasing published evidence confirming the long-term adult mental and physical health impact of childhood exposure to adverse events including different forms of abuse and family dysfunction. Looked-after Children and young people (LACYP) living in public care are known to be a highly vulnerable group, who have often experienced several pre-care poor socio-economic and family circumstances with subsequent placement instability, as well as inadequate compensatory care within the social care system. We aimed to evaluate the relationship between the adverse socio-emotional risk factors experienced by a cohort of LACYP and their emotional, behavioural and physical health needs within a South-West England Local Authority between Jan and Dec 2018.
Methods: We carried out a retrospective review of the medical records of all looked-after children and young people (LACYP) within one year (Jan to Dec 2018) at the North Somerset Local Authority (NSLA). This was an audit project of the LAC Health team completed as part of the Clinical Governance strategies of the NSLA.
Results: 93% (89/96) of the LACYP experienced at least one or more socio-emotional adverse risk factors. The commonest socio-emotional risk factors recorded were parent-related including poor mental health (67%), neglectful parenting (59%), drugs/alcohol abuse (45%) and domestic violence (47%). Forty-six (48%) of the LACYP had at least one or more emotional problems, 48 (50%) had neurodevelopmental conditions, while 63 (66%) had at least one or more physical problems. The most common emotional needs were behavioural problems (35%), anxiety/ depression (17%), nicotine/substance misuse (10%) and self-harm (6%).
Conclusion: High levels of physical, emotional, behavioral, developmental and neurodisability disorders are prevalent among LACYP due to their high vulnerabilities to adverse life experiences and trauma while living within their biological families. Present and future clinical implications of the socio-emotional risk factors and the need for more integrated multi-agency services for addressing the diverse health needs of the LACYP were discussed.
What is known?
• There is increasing awareness of the relationship between childhood exposure to adverse events and long-term adult mental and physical health
• Looked after children and young people (LACYP) are highly vulnerable to early traumatic and poor socio-economic circumstances exposure
What this study adds:
• Over 90% of LACYP experienced at least one ACE which disproportionately affected the youngest age-group
• Parental factors such as childhood abuse, alcohol/substance abuse and mental health problems were the most common adverse factors experienced by the LACYP
There is increasing evidence worldwide about the relationship between childhood exposure to adverse events including physical, emotional or sexual abuse, neglect or family dysfunction and long-term adult mental and physical health [1]. From a large survey of American adults reported recently, people who experienced four or more categories of childhood adversities, compared to those who had experienced none, had 4- to 12- fold increased health risks for alcoholism, drug abuse, depression and suicide attempt, as well as a 2- to 4- fold increase in smoking and poor self-rated health. There was also graded relationship between adverse childhood experiences (ACEs) and several risky behaviors and adult diseases such as sexually transmitted diseases, having ≥ 50 sexual intercourse partners, severe obesity, ischemic heart disease, cancer, chronic lung disease, skeletal fractures and liver diseases [1]. A similar UK study of a longitudinal prospective data from children followed up for 3 years after adoption reported a large proportion of them (42%) having been exposed to four or more ACEs, with significantly higher levels of emotional and behavioural problems compared to the general population [2]. Another recent UK 5-year prospective study compared the mental health outcomes of previously adopted and looked-after adults with their age-related control group. They reported significantly poorer outcomes, with 2 to 5-fold higher smoking rates, increased risk of high depression scores, high rates of criminal convictions and substance addiction for both the looked-after and adopted groups relative to the reference group [3].
Latest studies suggest that rates of adult mental ill health and alcohol misuse in the general population are strongly correlated with rates of Looked-after children [4]. There is now a growing body of research showing evidence for structural and functional brain differences associated with childhood maltreatment and identification of genetic variants responsible for either vulnerability to, or protection from later psychiatric disorders in adulthood. New studies have shown that children exposed to ACEs have increased right amygdala and bilateral anterior insula reactivity to threat on functional Magnetic Resonance Imaging (fMRI) scans. This may explain why abused children show greater hypervigilance and sensitivity to angry faces, which may have a negative effect on behavior and performance outside the home [5,6].
Looked after children and young people (LACYP) living in public care (usually represented by the Local Authority in the UK) are particularly known to be a highly vulnerable group, who have often experienced several pre-care poor socio-economic circumstances, health neglect including missed routine health surveillance, maltreatment or family dysfunction, genetic predisposition and the subsequent placement instability, as well as inadequate compensatory care within the social care system [7]. Entry into care is usually an additional traumatic experience associated with a significant sense of loss and attachment difficulties that are most often insufficiently recognized in care planning [34,35]. The latest UK’s Dept for Education’s reported statistics confirmed that abuse or neglect was the most common primary reason (in 53.2%) for children being referred for assessment by children’s social care in the year ending on 31st March 2018, followed by family dysfunction with 15.4%, and child’s disability or illness at 8.7% [8]. It has also been emphasized that neglect is not only harmful but can also be fatal [9].
CYP who have ever been referred to social care for assessment (including LACYP) are at significantly increased risk for mental health problems and poor educational outcomes due to the impact of diverse adversity trauma they have experienced [4]. There is evidence for higher rates of learning, emotional and behavioural problems and childhood disorders among the looked after children (LAC) population [10,11]. Warmth of parenting has been recognized as one of the protective mechanisms for mitigating the negative impacts of early ACEs [2].
We aimed to evaluate the relationship between the adverse socio-emotional risk factors experienced by a cohort of LACYP assessed in a South-West England Local Authority and their emotional, behavioural or physical health needs, between Jan and Dec 2018.
A retrospective review of the medical records of all looked-after children and young people (LACYP) assessed within one year (Jan to Dec 2018) within the North Somerset Local Authority (NSLA) was carried out. This was an audit project of the LAC Health team completed as part of the Clinical Governance strategies of the NSLA. No identifiable patient record was used and no research ethical approval was required. Statutory Initial health assessments (IHA) were usually undertaken by a Consultant Community Pediatrician using the latest edition of Coram/BAAF Forms. Information collected included the background personal and family social history, past medical and care history and details of examination findings. The data was collected and analyzed using MS Excel spreadsheet along with free online statistical software. Further details about how the statutory health assessments were conducted locally, including sources of information, formulation of health care plans and subsequent reviews have been previously reported [12].
Emotional and behavioural difficulties, sleep and developmental or learning problems were identified from the medical history obtained from multiple sources and through face-to-face interviews with the LACYP. The term “Behavioral difficulty” was used to cover a range of conduct, defiant, oppositional or challenging behaviors. Visual problems included common childhood refractive errors short- and long-sightedness, squint and astigmatism. Hearing problems included glue ear and sensorineural hearing impairment from any cause.
Statistical analysis
Spearman’s rank correlation coefficient [13], was used to determine the relationship between different proportions in discrete nominal groups within the sample. Chi square (with Yates correction when relevant) was used for comparing proportions among discreet non-nominal groups of patients (http://www.socscistatistics.com/tests/chisquare2/Default2.aspx) while T-test was used for comparison of two means (https://www.medcalc.org/calc/comparison_of_means.php). Analysis of variance (ANOVA) was used when testing for differences between three or more means (http://statpages.info/anova1sm.html). Statistical significance was accepted at the p value of < .05.
Clinical and Epidemiological characteristics of LACYP
A total of 96 LACYP aged between 5 months and 18 years (averaged 6 yrs 10 months) were assessed during the one-year period, with equal male and female distribution. There was no statistical difference between the genders in relation to several clinical characteristics that were assessed. Each of them had an average of four multidisciplinary professionals including Social Workers, Dentists, Opticians and Health Visitors and an average of three physical/mental health diagnoses. Further clinical and epidemiological characteristics of the LACYP including age distribution, seasonal variability of attendance, clinic non-attendance (DNA) rates, legal status and different types of placement have been described [12]. Briefly, the preschool children 1 to 4 years were the largest group of patients (34%), while the school children 5-9 yrs were 24%. The school children (5-9 yrs) had the largest burden of health diagnosis (average of 4 vs. 3 for the whole cohort).
Socio-emotional adverse risk factors
Eighty-nine (93%) of the LACYP experienced at least one or more of the nineteen socio-emotional adverse risk factors classified into four categories (Table 1). 80 (83%) experienced at least two ACEs. The four ACE categories (Table 1) included (i) parental factors (80%) such as abuse in childhood, alcohol and substance abuse, mental health problems, and Learning Difficulties; (ii) prenatal insults (49%) such as intra-uterine exposure to stress, tobacco, drugs and alcohol; (iii) family-related insults (73%) such as parental neglect and exposure to domestic violence; (iv) adverse child factors (38%) such as physical, emotional or sex abuse, incomplete immunization and poor school attendance. Each LACYP had an average of 5 identifiable risk factors, ranging from none to twelve. The most common socio-emotional risk factors recorded were parent-related including poor mental health (65%), neglectful parenting (57%), drugs/alcohol abuse (41%) and exposure to domestic violence (47%) (Table 1).
| Table 1: Showing 4 different categories of socio-emotional adverse risk factors experienced by the LACYP. | ||||
| Risk factors / Categories | No LACYP | Avg Age (Months) | Percent (%) | |
| All Parental factors | 77 | 64 | 80 | |
| Mental Health problems | 62 | 55 | 65 | |
| Nicotine / Smoking | 48 | 59 | 50 | |
| Illicit Drugs abuse | 45 | 46 | 47 | |
| Alcohol abuse | 39 | 68 | 41 | |
| Learning Difficulties | 30 | 40 | 31 | |
| History of CPP / LAC | 17 | 36 | 18 | |
| Criminal behavior | 15 | 52 | 16 | |
| History of ADHD / ASD | 6 | 28 | 6 | |
| All Family-related insults | 70 | 62 | 73 | |
| Neglectful Parenting | 55 | 57 | 57 | |
| Parental DV exposure | 45 | 47 | 47 | |
| All Prenatal insults (Intra-uterine exposure) | 47 | 47 | 49 | |
| Nicotine / Smoking | 32 | 33 | 33 | |
| Stress | 32 | 33 | 33 | |
| Illicit Drugs | 21 | 22 | 22 | |
| Alcohol | 8 | 8 | 8 | |
| All Adverse child factors | 36 | 106 | 38 | |
| Physical Abuse | 17 | 72 | 18 | |
| Immunization Incomplete | 15 | 134 | 16 | |
| Emotional Abuse | 9 | 105 | 9 | |
| School Absences | 7 | 177 | 7 | |
| Sexual Abuse | 3 | 198 | 3 | |
| Legend: CPP: Child Protection; LAC: Looked After; ADHD: Attention Deficit Hyperactivity Disorder; ASD: Autistic Spectrum Disorder; DV: Domestic Violence. | ||||
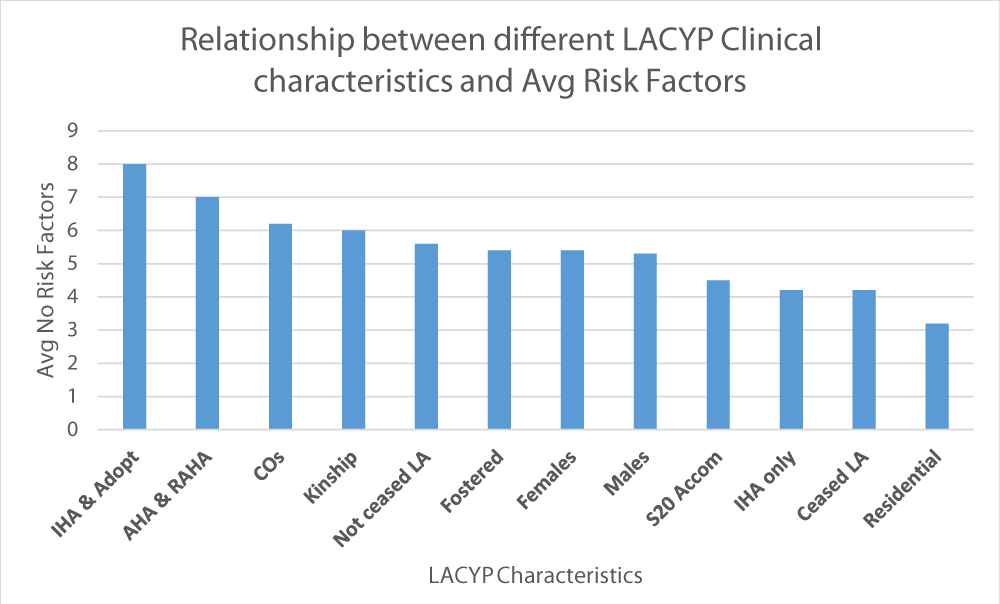
The highest average number of adverse risk factors was experienced by LACYP who had initial health assessments (IHA) followed by adoption health assessment (8) and those who had initial adoption health assessment (AHA) and then review HA later (7). The LACYP in residential placement and those who ceased to be LA had the lowest recorded socio-emotional adverse risk factors (Figure 1).
Figure 1: Showing average number of adverse risk factors experienced by different categories of LACYP$&. Legend: IHA: Initial Health Assessments; AHA: Adoption Health Assessment; RAHA: Review Adoption Health Assessment; LA: Looked-After; CO: Court Orders; s20 Accom: Children’s Act 1989 section 20. $F score 3.8 (p < 0.001); &Statistically significant (F = 3.80, p < .001).
There was statistically significant relationship between the number of adverse life experiences and the age of the LACYP (p < .001). The youngest LACYP disproportionately experienced higher numbers of ACEs compare to the older ones (Table 2). There were statistically significant differences between the number of adverse risk factors experienced by LACYP with different categories of physical, emotional, neurodevelopmental or perinatal problems (Table 3). The youngest children who suffered perinatal problems were exposed to the highest number of ACEs (average of 8). It appeared interesting that the LACYP with emotional and behavioural problems experienced the least average number of ACEs.
| Table 2: Showing the relationship between the number of adverse risk factors and average age of the LACYP. | |||
| No Risks factors | No LACYP& | Avg No Prof (± SD) | Avg Age (Months ± SD) |
| 0 | 7 | 3.9 ± 1.2 | 194 ± 39 |
| 1 | 9 | 3.9 ± 1.2 | 117 ± 79 |
| 2 | 6 | 4.0 ± 1.1 | 148 ± 66 |
| 3 | 8 | 4.5 ± 2.3 | 89 ± 71 |
| 4 | 8 | 4.8 ± 1.8 | 126 ± 75 |
| 5 | 5 | 4.2 ± 1.1 | 31 ± 23 |
| 6 | 14 | 4.1 ± 1.3 | 58 ± 37 |
| 7 | 12 | 3.5 ± 0.9 | 60 ± 47 |
| 8 | 10 | 4.2 ± 1.6 | 38 ± 59 |
| 9 | 9 | 4.1 ± 0.9 | 58 ±38 |
| 10 | 3 | 4.7 ± 1.5 | 49 ± 24 |
| 11 | 3 | 3.3 ± 1.5 | 15 ± 9 |
| 12 | 2 | 3.0 ± 1.4 | 54 ± 66 |
| Rho& | -0.297 | -0.185 | -0.784 |
| p value | .322 | .54 | .002** |
Legend: SD: Standard Deviation; LACYP: Looked After Children and Young People; Prof: Professionals
&Spearman’s rank correlation coefficient; **Statistically Significant |
|||
| Table 3: Showing the relationship between different categories of health problems and adverse risk factors among the LACYP. | ||||||
| Category | No LACYP | Percent (%) | Avg No Diag (± SD) | Avg No Risks (± SD) | Avg No Prof (± SD) | Avg Age (Months ± SD) |
| Physical | 63 | 66 | 3.6 ± 2 | 6 ± 3 | 4.2 ± 1.5 | 69 ± 61 |
| ND | 48 | 50 | 4.1 ± 2.1 | 6 ± 2.8 | 4.5 ± 1.5 | 82 ± 64 |
| Emotional | 46 | 48 | 4.4 ± 2 | 5 ± 3.3 | 4.5 ± 1 | 123 ± 63 |
| Perinatal | 10 | 10 | 4.1 ± 2.2 | 8 ± 2.4 | 4 ± 1.5 | 21 ± 23 |
| F score£ | -- | -- | 1.47 | 3.95 | 0.81 | 10.65 |
| p value | -- | -- | .23 | .009** | .49 | < .001** |
| Legend: ND: Neurodevelopmental/Neurodisabilites; Diag: Diagnosis; Prof: Professionals; £ANOVA test; **Statistically significant | ||||||
Diagnosed health problems
The LACYP experienced an average of three diagnosed physical/emotional problems, ranging from none to ten. The health needs varied significantly according to different age groups (Table 3) and were classified into physical, perinatal, emotional and neurodevelopmental categories.
Physical and perinatal health needs
The youngest LACYP (Average age of 21 months) had perinatal problems such as intra-uterine growth retardation (IUGR) and Neonatal Abstinence syndrome (NAS). 66% (63/96) of the LACYP (average age of 6 years) had at least one or more physical conditions (Table 4). The commonest physical problems among infants less than 1 year old (n = 14) were eczema/dry skin (7), feeding problems/reflux (4), congenital defects (3) and hypotonia (2). Older children ages 1 to 9 years (n = 56) were also frequently diagnosed with eczema/dry skin (23/56), hypermobile joints (11) constipation (8), dental caries (6) and overweight (4). In children 10 years and older (n = 26), the most common physical ailments were overweight (6), dental caries (4) and constipation (3).
| Table 4: Showing the relationship between the physical health diagnosis and risk of ACEs £. | |||||||||
| Diagnosis | No LACYP | Perc (%) | Avg No Risks | Avg Age (mons) | < 1yr | 1 - 4yrs | 5 - 9yrs | 10 - 15yrs | ≥ 16 |
| Eczemaα | 32 | 33 | 6 | 49 | 7 | 13 | 10 | 2 | 0 |
| Constipation | 13 | 14 | 5 | 75 | 2 | 5 | 3 | 1 | 2 |
| Hypermobile | 12 | 13 | 5 | 73 | 0 | 6 | 5 | 1 | 0 |
| Dent_Caries | 10 | 10 | 4 | 127 | 0 | 0 | 6 | 1 | 3 |
| Overweightβ | 10 | 10 | 4 | 126 | 0 | 0 | 4 | 6 | 0 |
| Cong_Defect¥ | 6 | 6 | 8 | 48 | 3 | 1 | 1 | 1 | 0 |
| Feeding_GOR | 6 | 6 | 5 | 10 | 4 | 2 | 0 | 0 | 0 |
| Enuresis | 5 | 5 | 7 | 88 | 0 | 1 | 3 | 1 | 0 |
| Poor growth | 3 | 3 | 8 | 21 | 1 | 2 | 0 | 0 | 0 |
| Iron_Def | 3 | 3 | 4 | 127 | 0 | 0 | 2 | 0 | 1 |
| Microcephaly | 3 | 3 | 6 | 78 | 0 | 1 | 2 | 0 | 0 |
| Genetic_Synd€ | 3 | 3 | 7 | 85 | 0 | 2 | 0 | 1 | 0 |
| SC_Trait | 2 | 2 | 10 | 78 | 0 | 1 | 1 | 0 | 0 |
| Others$ | 2 | 2 | 7 | 20 | 1 | 1 | 0 | 0 | 0 |
| Cong_HD | 1 | 1 | 5 | 11 | 1 | 0 | 0 | 0 | 0 |
| Ortho_Probµ | 1 | 1 | 8 | 11 | 1 | 0 | 0 | 0 | 0 |
| Hypothyroidism | 1 | 1 | 7 | 121 | 0 | 0 | 0 | 1 | 0 |
| Brain_Inj | 1 | 1 | 8 | 17 | 0 | 1 | 0 | 0 | 0 |
| Legend: αEczema including dry skin and chronic urticarial; µOrthopedic problems including congenial talipes and Hip dysplasia; €Genetic Syndromes include Angelman’s syndrome, Brachio-Otic Syndrome, NF1, Chromosomal copy number variants.
¥Congenital defects including Corpus Callosum Dysgenesis, Pachygyria, Scaphocephaly, Hydrocephalus, Arnold Chiari malformation. βOver weight and obesity; $Others: Miscellaneous conditions including Autoimmune Neutropenia (1) and mild Dysmorphism (1). Def: Deficiency; GOR: Gastro-Esophageal Reflux; Cong: Congenital; HD: Heart Disease; Inj: £Sample size: <1y = 14; 1-4yrs = 33; 5-9yrs = 23; 10-15yrs = 14; >15yrs = 12. |
|||||||||
Emotional and neurodevelopmental health needs
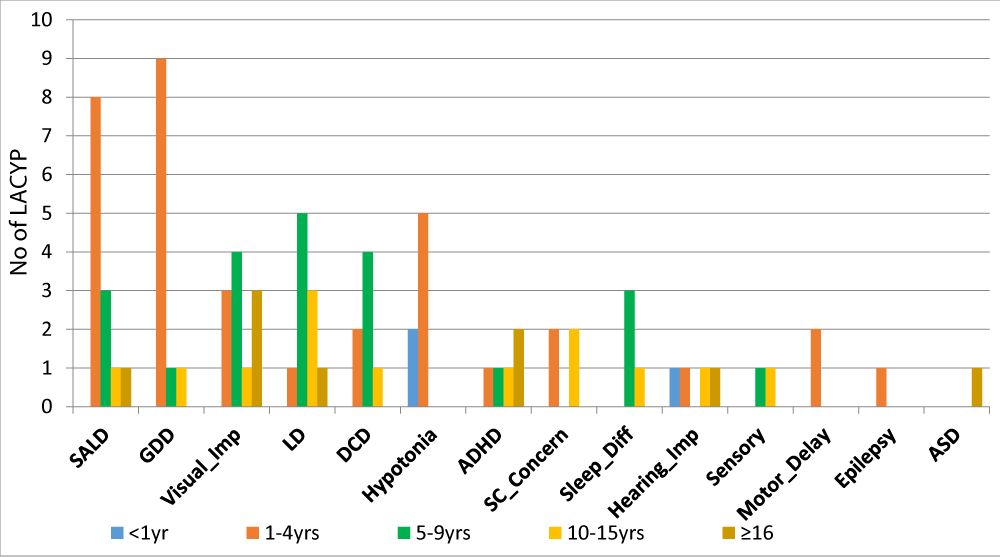
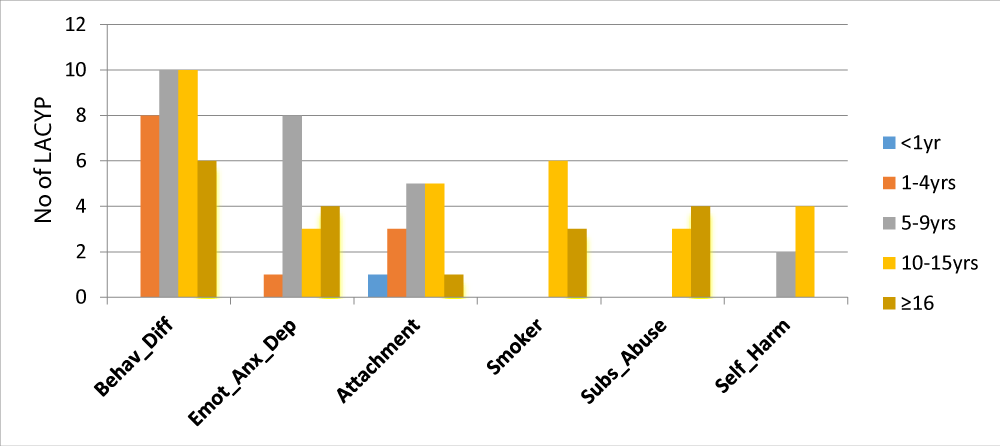
50% of all the LACYP had one or more neurodevelopmental or neurodisability (ND) diagnosis (Figure 2). ND disorders were commonest in the 1 to 4 year aged children (n = 33) including global developmental delay (9), speech/language delay (8), hypotonia (5) and visual problems (3). The school age children (n = 23) were also disproportionately affected by ND problems such as learning difficulties (5), dyspraxia (4), visual problems (4), sleep (3) and speech (3) disorders. Behavioural difficulties were the most common mental health problems among the LACYP (48%) and it affected 40% of preschool, 43% school aged, 77% of adolescents and 46% of YP above 15 years. The other emotional problems including anxiety, depression and were commoner among school age (35%) while attachment difficulties affected 38% of adolescents and 22% of school children respectively (Figure 3). Self-harm was prevalent especially among the 10-15 yrs age group (31%) and 9% among school aged (5-9 yrs). 46% of adolescents smoked tobacco and 31% of YP abused various other substances.
Figure 2: Showing the distribution of various neurodevelopmental and neurodisability problems among the LACYP£. Legend: £See Table 4 for age-group sample size; Diff: Difficulties; SC: Social Communication; DCD: Developmental Coordination Disorder; LD: Learning Difficulties; ADHD: Attention Deficit Hyperactivity Disorder; SALD: Speech & Language Disorder; ASD: Autism Spectrum Disorder; GDD: Global Developmental Delay.
Figure 3: Showing the distribution of various emotional and behavioural problems among the LACYP£. Legend: £See Table 4 for age-group sample size; Subs: Substance; Behav_Diff: Behavior Difficulties; Emo_Anx_Dep: Emotional difficulties including Anxiety and Depression.
Multidisciplinary professionals’ involvement
Each LACYP had an average of 4 multi-disciplinary professionals, ranging from two to nine (Table 5). There was a statistically significant association between number of professionals involved and the number of diagnosed health problems (p = .002) among the LACYP (Table 5). The commonest professionals included (Table 6) Social worker (100%), Dentist (77%), Optician/Orthoptist (52%), Health Visitor (44%), Audiology (16%), Child and adolescent mental health services (CAMHS) (15%), speech and language therapists (SALT) (13%) and Community Pediatricians (11%).
| Table 5: Showing the relationship between involvement of professionals and age and diagnosis. | ||||
| Total No Prof | No LACYP | Percent (%) | Avg No Diagnosis (± SD) | Avg Age (Months ± SD) |
| 2 | 10 | 10 | 1.4 ± 1.3 | 45 ± 65 |
| 3 | 21 | 22 | 2 ± 1.3 | 70 ± 61 |
| 4 | 40 | 42 | 3.4 ± 1.7 | 99 ± 73 |
| 5 | 13 | 14 | 3.4 ± 2 | 72 ± 65 |
| 6 | 7 | 7 | 4.1 ± 2 | 107 ± 87 |
| 7 | 2 | 2 | 8 ± 2.8 | 103 ± 4 |
| 8 | 2 | 2 | 6.5 ± 4.9 | 53 ± 51 |
| 9 | 1 | 1 | 5 ± 0 | 30 ± 0 |
| Rho&/ F score£ | -0.83& | - | 6.67£ | 1. 17£ |
| p value | .011** | - | < .001** | 0.32 |
| Legend: &Spearman’s rank correlation coefficient; £Anova Test; **Statistically significant | ||||
| Table 6: Showing involvement of multidisciplinary professionals. | |||
| Professionals | No LACYP | Percent (%) | Avg Age (Months) |
| Social_W | 96 | 100 | 83 |
| Dentist | 74 | 77 | 96 |
| Orthoptist | 50 | 52 | 118 |
| HV | 42 | 44 | 24 |
| Audiology | 15 | 16 | 66 |
| CAMHS | 14 | 15 | 154 |
| Clin_Psych | 14 | 15 | 149 |
| SALT | 13 | 14 | 67 |
| CCH_Paed | 11 | 11 | 77 |
| Ophthalmologist | 9 | 9 | 24 |
| Gen_Paed | 9 | 9 | 41 |
| Physiotherapy | 7 | 7 | 48 |
| Dietitian | 6 | 6 | 65 |
| FSW | 5 | 5 | 101 |
| Neurologist | 4 | 4 | 20 |
| ENT | 3 | 3 | 76 |
| Edu_Psych | 3 | 3 | 204 |
| Sp_Nurse | 2 | 2 | 8 |
| Continence | 2 | 2 | 116 |
| Cardiologist | 1 | 1 | 76 |
| Neurosurgeon | 1 | 1 | 17 |
| Ortho_Surg | 1 | 1 | 11 |
| Sch_Mentor | 1 | 1 | 186 |
| Sch_Nurse | 1 | 1 | 169 |
| OT | 1 | 1 | 17 |
| Legend: Ed_Psych: Educational Psychologist; Clin_Psych: Clinical Psychologist; FSW: Family Support Worker; Social_W: Social Worker; SALT: Speech and Language Therapist; OT: Occupational Therapist; CCH_Paed: Community Child Health Pediatrician; ENT: Ear, Nose, Throat Surgeon; Sp_Nurse: Special Nurse; Ortho_Surg: Orthopedic Surgeon; CAMHS: Child and Adolescent Mental Health Services. | |||
Six different categories of multi-agency professionals were involved with the care of the LACYP including (i) Social Care and Mental Health Specialists such as FSW, SW and CAMHS (100%), (ii) Primary care Specialists such as HV, Dentist, Optician and Audiologist (99%), (iii) Secondary care specialists such as Pediatricians, Surgeons and specialist nurses (28%), (iv) Allied Therapists such as OT, Physiotherapist, SALT (18%), (v) Tertiary care Specialists including Neurologists and Cardiologists (5%) and (vi) Education Specialists (4%) such as school nurses and educational psychologists.
Life adversities, risk factors or disadvantages that many LACYP face have been classified in a number of ways including: Biological (in-utero exposure to drugs, alcohol); Parent-child relationships (Neglect); Family factors (such as domestic violence, parental mental health, alcohol or drug abuse); Economic factors (including poverty, overcrowding, homelessness); or Neighborhood (bullying, crime/antisocial behaviors) [14,15]. The risk factors are often related and can create synergistic effects in leading to later mental health problems [15].
In England, at least 1.6 million children were reported to have needed a social worker for assessment and provision of additional support at some point over the previous 6 years before 2018, equivalent to 1 in 10 children. About 10% of these CYP were being looked-after by the public during the period [4]. Many of them were known to have experienced multiple adverse and traumatic life situations in their lives. These vulnerable CYP are known to carry a heavy burden of emotional, developmental, behavioural and physical problems. They also perform significantly worse than other CYP at all stages of education. Assessment data shows at least 12% of these children have their mental health recorded as a factor of concern by children’s social care. Almost half of LACYP meet the criteria for a psychiatric disorder compared to 10% children who are not Looked After [4]. This agrees with this study showing that 48% of the LACP had at least one or more behavioural or emotional problems.
Data from LACYP in England from 2017 showed that 61% (44,600 children) came into public care due to an initial abuse or neglect, 15% (11,150) family dysfunction, 8% (6,030) family in acute stress and 7% (5,100) absent parenting [16]. NICE/SCIE PH28 (2015) highlighted the evidence that most LACYP have come from families where parents are struggling with issues such as domestic violence, substance abuse, alcohol abuse and mental health problems, often in combinations [35]. Similar studies of Scottish adopted children under the age of five also showed that the most common risk factors experienced by the children were multiple family difficulties including Parenting capacity impaired by alcohol and substance misuse, mental health difficulties, and domestic violence, within the context of poor housing conditions and limited financial circumstances. 384 (89%) of the adopted children had directly experienced abuse (two thirds exposed to emotional abuse) or neglect (four fifths). Significant numbers of their mothers had also experienced ACEs including abuse (40%) or neglect (45%), and being looked after away from home (25%). Almost one fifth (17%) of fathers had experienced abuse, almost one quarter (24%) neglect, and 14% had been looked-after away from home [18].
Our study found that parent-related adverse factors were the most common traumatic experiences faced by 80% of the LACYP, including poor mental health (65%), neglectful parenting (57%), drugs/alcohol abuse (41%) and exposure to domestic violence (47%). Direct child-related abuses or neglect such as physical, emotional or sexual abuse, school absences and missed immunizations, were recorded in 18%. Previous study from another LA has shown that obtaining immunization details was a problematic area (affecting 75% of cases), which was resolved in only 42% [19]. LACYP are less likely to be ‘up-to-date’ with their immunizations than other children in the general population due to a wide variety of socioeconomic disruptions [20]. Almost half (49%) of the LACYP in this study experienced significant prenatal insults during the pregnancy from maternal stress or abusive use of nicotine, alcohol and other illicit drugs.
Studies have shown links between mental ill-health and ACEs, and have provided evidence that mental health needs are much more prevalent among looked-after children compared to the general population [17,21,22]. The rate of life disadvantages experienced by LACYP population in this study shows that they are at least twice to 12 times more than those reported for the general population of 10-17 year old children in England. For example, the reported prevalence of domestic violence (47 vs. 13.3%), parental mental health (65 vs.28.4%), alcohol abuse (41 vs. 12.4%) and supervisory neglect (57 vs. 4.5%) show evidence of significant differences, when compared to the findings in this study [14].
LACYP experience high incidence of behavioural difficulties including self-harm, often resulting from a combination of underlying emotional distress, depression, self-hatred and access to potentially fatal means [23]. Self-harm was reported in 6% of this cohort of LACYP, especially among the school age and adolescent groups.
66% of LACYP in our study experienced at least one or more physical problems, while 50% and 48% respectively had neurodevelopmental and emotional morbidities. Previous studies have reported that two thirds of children in care have at least one physical complaint, including poor dental health and incomplete routine childhood immunizations [24,36].
Need for dedicated and integrated child-centered and need-based mental and physical health services
Published evidence confirm that LACYP have high levels mental and physical health needs due to their vulnerability to high levels of adverse life and family traumatic experiences. The LACYP in this study required high levels of multi-agency professionals’ involvement (average of 4) from several service areas. This emphasizes the need for early provision of intensive support from several agencies working together in coordinated and integrated models to support their mental health wellbeing [4]. The mental health state of each individual LAC follows several distinct trajectories across their life time. Their health needs are therefore variable and often complex. This suggests the need for regular monitoring and assessment of their emotional wellbeing [25]. High prevalence of co-morbid physical ailments among LACYP with mental health problems emphasizes the importance of close working across mental and physical health services [26]. Their varied and complex needs are best met by a range of specialist multi-agency services operating collaboratively across different settings. As LACYP are often moved around the country due to placement instability, it is recommended that these specialized mental health services are integrated closely with children’s social services and designed as regional or national networks to maximize their effectiveness and provide the necessary seamless access to the LACYP [27].
The UK’s National Institute for Clinical and Health Excellence (NICE) has highlighted the importance of providing dedicated mental health services offering skilled interventions to the LACYP. The services should be flexible and easily accessible to both the LACYP and their carers. These services are recommended to be structured as integrated teams (virtually or, ideally, co-located), and have a mix of professionals who will vary according to local circumstances [35]. They have also recommended the need for the professionals to collaborate closely and share relevant and sensitive information, to ensure provision of effective holistic care to the LACYP [33,35]. However, there is considerable variation nationwide in the scope and threshold of specialist child and adolescent mental health services (CAMHS) for LACYP due to lack of clear models, care pathways and consensus on which CYP would benefit from CAMHS input [37]. LACYP with attachment and behavioural problems are particularly at risk of being neglected due to inconsistent threshold applied by various CAMH services. It is advocated that joint pathway planning by different mental health and social agencies is imperative [28].
Though mean maximum waiting times for access to child and adolescent mental health services (CAMHS) are reported to have fallen since 2012, too many children and young people are still waiting far too long for assessment and then again for treatment [29]. It is heartening to know that progress in several policy decisions and clinical pathways are being steadily achieved in the UK, aiming to ensure provision of sustainable effective mental health services to LACYP.
Recent UK Government initiatives have led to the implementation of the principle of service integration across health, education, justice and social care, leading to formation of sustainability and transformation partnerships (STPs) and Local Transformation Plans (LTPS) across the country [29]. It is reassuring that establishment of a small but increasing number of specialized CAMHS services are being reported across the UK to support carers as well as the LACYP with complex attachment-and trauma-related psychopathology, aiming for long-term developmental recovery, rather than using the ineffective traditional acute care models [27]. It is also reassuring to know that the UK Government has committed over £1 million to pilot high quality mental health assessments for LACYP, focusing on establishing individual needs as children enter care [4].
Need for preventative integrated mental health services
Many CYP would have been under the surveillance of children’s social care and other multi-agencies before they become looked-after. LACYP are very vulnerable to experiencing multiple early life adversities and trauma while they are still living with their biological families. The intervention for the CYP-in-Need (CIN) would therefore need to include effective, early support for whole families, which prevent further escalation of their adverse life experiences. As parental problems often co-occur with CYP living with poverty and deprivation, the parents often need support from multi-agency professionals for themselves to be able to offer the CYP a reasonable level of positive parenting and effective supervision [4]. It has been argued that early supportive interventions for CYP at high risk of being exposed to ACEs would be the most effective way to prevent future psychiatric disorders in adulthood [29-31]. The latest UK’s Dept for Education’s (DfE) report showing evidence of poor educational outcomes of CYP under the care of Children’s social care for additional support, emphasizes the need for the social care and educational agencies to work closely together, helping the CYP realize their maximum potentials and life chances, while breaking the cycle of disadvantages and trauma [8].
Although the completion of the Strengths and Difficulties Questionnaire (SDQ) for all looked-after children has been a statutory requirement since 2009, there is a huge variation in completion rates across local authorities. It has been reported that only a 75 per cent completion rate was achieved in England as a whole between 2014 and 2016 [32]. SDQ was not routinely used during the statutory IHAs within the NSLA but was more commonly completed for the regular review assessments conducted by the specialist LAC nurse practitioners. A recently constituted Expert Working Group by the UK’s Social Care Institute for Excellence (SCIE) has suggested that the SDQ alone is not an effective way to measure the mental health and emotional wellbeing of LACYP, as it is unable to detect post-traumatic stress disorder (PTSD), attachment disorganisation and developmental issues such as autistic spectrum condition. They have therefore advocated greater research into other validated comprehensive screening tools that are better suited to the peculiar needs of the LACYP [29].
This study was a retrospective analysis of clinical records from LACYP in a single center of England, UK. There are some potential limitations to be considered in interpreting the results. They may not be representative of other regions and locations within England and other countries of the United Kingdom. Efforts were made to minimize the possibility of biased estimates from incomplete data by the clinical information being obtained and recorded by the same team of few specific professionals throughout the study period. Regular multi-agency discussions between the social and health teams were held throughout the study period, ensuring that the high-standard of routinely collected data was maintained across all the services. The strength of the study includes the length of follow-up spanning a whole year and analysis of a comprehensive single-site data set with detailed description of the clinical and epidemiological characteristics of LACYP under the care of a relatively small LA in the South West of England.
High levels of physical, emotional, behavioural, developmental and neurodisability disorders are prevalent among LACYP due to their high vulnerabilities to adverse life experiences and trauma while living within their biological families. Several ongoing Government initiatives have started addressing the indispensable need for well-funded, highly integrated multi-agency mental health services to this vulnerable group of CYP. Several opportunities for prevention of enduring or escalating life adversities among high-risk CYP need to be more extensively explored and implemented. Many future adult mental and physical morbidities can be effectively avoided if better attention is paid to ensuring CYP are kept safe and stable across several settings.
The author hereby gratefully acknowledges the invaluable support of the LAC secretary (Amanda Burrows) and other Community Child Health secretaries, for their excellent administrative support.
- Felitti VJ, Anda RF, Nordenberg D, Williamson DF, Spitz AM, et al. Relationship of Childhood Abuse and Household Dysfunction to Many of the Leading Causes of Death in Adults: The Adverse Childhood Experiences (ACE) Study. Am J Prev Med. 2019; 56: 774-786. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/9635069
- Anthony RE, Paine AL, Shelton KH. Adverse Childhood Experiences of Children Adopted from Care: The Importance of Adoptive Parental Warmth for Future Child Adjustment. Int J Environ Res Public Health. 2019; 16: 2212. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/31234480
- Teyhan A, Wijedasa D, Macleod J. Adult psychosocial outcomes of men and women who were looked-after or adopted as children: prospective observational study. BMJ Open. 2018; 8: e019095. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/29439075
- DfE. Children in Need of help and protection: data and analysis: 2019.
- McCrory E, De Brito SA, Viding E. The impact of childhood maltreatment: a review of neurobiological and genetic factors. Frontiers in Psychiatry. 2011; 2: 48. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/21847382
- Woolgar M. The practical implications of the emerging findings in the neurobiology of maltreatment for looked after and adopted children: Recognising the diversity of outcomes. 2013; 37: 237-252.
- Burton K. Chapter 2: The child's health. In: Merredew F and Sampeys C (eds) Promoting the Health of Children in Public Care. London: BAAF. 2015; 13-49.
- Department for Education (DfE) UK. Characteristics of Children in Need: 2017-2018. Headlines. London: Department for Education. 2019.
- Brandon M, Bailey S, Belderson P, Larsson B. The Role of Neglect in Child Fatality and Serious Injury. Child Abuse Review. 2014; 23: 235-245.
- Sempik J, Ward H, Darker I. Emotional and behavioural difficulties of children and young people at entry into care. Clin Child Psychol Psychiatry. 2008; 13: 221-233. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/18540226
- Tarren-Sweeney M. The mental health of children in out-of-home care. Child and Adolescent Psychiatry. 2008; 21: 345-349. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/28734200
- Ogundele MO. Clinical characteristics of children and young people looked after by a South-West England Local Authority in 2018. Advances in Pediatrics and Neonatal Care. 2019.
- Wessa P. Free Statistics Software, Office for Research Development and Education. 2019.
- The Children's Society. Good Childhood Report. 2017.
- Arango C, Díaz-Caneja CM, McGorry PD, Rapoport J, Sommer IE, et al. Preventive strategies for mental health. The Lancet Psychiatry. 2018; 5: 591-604.
- DfE. Children looked after in England (including adoption). 2017.
- Department of Health (DoH)/ DfE. Transforming Children and Young People's Mental Health Provision: A Green Paper. 2017
- Cusworth L, Biehal N, Whincup H, Grant M, Hennessy A. Children looked after away from home aged five and under in Scotland: experiences, pathways and outcomes. 2019.
- Croft G. Implementation of Health Recommendations after Initial Statutory Health Assessment. Adoption & Fostering. 2009; 33: 76-81.
- Walton S, Bedford H. Immunization of looked-after children and young people: A review of the literature. Child Care Health Dev. 2017; 43: 463-480. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/28317146
- Anda RF, Felitti VJ, Bremmer JD, Walker JD, Whitfield CH, et al. The enduring effects of abuse and related adverse experiences of childhood. Eur Arch psy & clin neurosc. 2006; 256: 174-186. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/16311898
- Hughes K, Bellis M, Hardcastle K, Sethi D, Butchart A, et al. The effect of multiple adverse childhood experiences on health: a systematic review and meta-analysis. Lancet Public Health. 2017; 2: e356-e366. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/29253477
- Wadman R, Clarke D, Sayal K, Armstrong M, Harroe C, et al. A sequence analysis of patterns in self-harm in young people with and without experience of being looked after in care. Br J Clin Psychol. 2017; 56: 388-407. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/28593633
- Williams J, Jackson S, Maddocks A, Cheung WY, Loveb A, et al. Case-control study of the health of those looked after by local authorities. Arch Dis Child. 2001; 85: 280-285. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/11567933
- Tarren-Sweeney M. Rates of meaningful change in the mental health of children in long-term out-of-home care: A seven- to nine-year prospective study. Child Abuse Negl. 2017; 72: 1-9. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/28734200
- Hill C, Thompson M. Mental and Physical Health Co-Morbidity in Looked after Children. J Interpers Violence. 2003; 8: 315-321. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/19768893
- Tarren-Sweeney M. Mental health services for our most vulnerable children. Clinical Child Psychology and Psychiatry. 2017b; 22: 521-523. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/28994327
- Rao P, Ali A, Vostanis P. Looked after and Adopted Children: How Should Specialist CAMHS Be Involved? Adoption & Fostering, 2010; 34: 58-72.
- Social Care Institute for Excellence (SCIE). Expert Working Group Final Report. Improving mental health support for our children and young people. London. 2017.
- Fryers T, Brugha T. Childhood determinants of adult psychiatric disorder. Clin Pract Epidemiol Ment Health. 2013; 9: 1-50. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/23539489
- Woolgar M, Baldock E. Attachment disorders versus more common problems in looked after and adopted children: comparing community and expert assessments. Child and Adolescent Mental Health. 2015; 20: 34-40.
- Channa K. A healthy state of mind: Improving Young People's Mental Fitness. London: LOCALIS. 2017.
- NICE/SCIE. Looked After Children and Young People. 2013.
- National Institute for Care and Health Excellence (NICE) UK. Children's attachment: attachment in children and young people who are adopted from care, in care or at high risk of going into care. NG26. 2015.
- NICE/ Social Care Institute for Excellence (SCIE). Looked After Children and Young People. PH28. 2015.
- Meltzer H, Gatward R, Corbin T, Goodman R, Ford T. The Mental Health of Young People Looked after by Local Authorities in England. London: Of?ce for National Statistics. 2003.
- Children's Commissioner, UK. Lightning review: Access to child and mental health services. London: Children's Commissioner for England. 2016.