More Information
Submitted: 29 June 2020 | Approved: 14 July 2020 | Published: 15 July 2020
How to cite this article: Patil PM, Sharma K, Kaur N. Acute necrotising pancreatitis masquerading as psoas abscess: A report of two cases. Arch Surg Clin Res. 2020; 4: 018-021.
DOI: 10.29328/journal.ascr.1001046
ORCiD: orcid.org/0000-0002-5648-7992
Copyright License: © Patil PM, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Acute necrotizing pancreatitis; Psoas abscess; Pancreatic fistula; Step up approach
Acute necrotising pancreatitis masquerading as psoas abscess: A report of two cases
Praveenkumar M Patil1*, Kartik Sharma2 and Navneet Kaur3
1Senior Resident, Department of Surgery, University College of Medical Sciences and GTB Hospital, New Delhi, India
2Post Graduate Resident, Department of Surgery, University College of Medical Sciences and GTB Hospital, New Delhi, India
3Director Professor & Unit Head, Department of Surgery, University College of Medical Sciences and GTB Hospital, New Delhi, India
*Address for Correspondence: Dr. Praveenkumar M Patil, Senior Resident, Department of Surgery, University College of Medical Sciences and GTB Hospital, New Delhi, India, Tel: 9844004831; Email: patilbmc@gmail.com; drpraveenpatil@hotmail.com
Acute pancreatitis is commonly diagnosed clinically, with its classical presentation of upper abdominal pain, backed by raised serum levels of enzymes amylase and lipase. However, unusual presentation of this common surgical emergency as a psoas abscess is a rare finding which can lead to missed diagnosis with a fatal outcome.
We present here two such cases of acute necrotising pancreatitis masquerading as psoas abscess, with no classical clinical symptoms and only mildly raised levels of serum amylase and lipase. The region of pancreas involved by necrosis influenced the site of presentation of the psoas abscess. In the first case, acute necrotising pancreatitis involving head and neck of pancreas presented as psoas abscess presenting in the right lumbar region, while the left side collection due to pancreatitis involving body and tail of pancreas manifested as an abscess in left flank.
While evaluating the aetiology of a psoas abscess, a differential diagnosis of necrotizing pancreatitis should be kept as a possibility.
Acute pancreatitis (AP) is an inflammatory condition of the pancreas. The diagnosis of AP requires 2 of the following 3 features: (1) abdominal pain characteristic of AP, (2) serum amylase and/or lipase ≥3 times the upper limit of normal, and (3) characteristic findings of AP on CT scan [1]. However, atypical presentation occur with symptoms secondary to pancreatic collections with no recent history of acute episode of pancreatitis. Though, most frequent location of the collections is the lesser peritoneal sac, 20% are located at extra pancreatic sites like pleura, mediastinum, pelvis, spleen, liver and perinephric space. Rarely, it can be present as a psoas abscess [2]. This is due to the destructive nature of the pancreatic enzymes, which are in high concentrations in these collections, resulting in collections sweeping into surrounding areas [3,4].
Iliopsoas abscess is a potentially life-threatening form of retroperitoneal infection that involves the iliopsoas compartment, which contains the psoas and iliacus muscle. Before the discovery of modern antitubercular treatment, iliopsoas abscess was a well-recognized complication of tuberculosis of the spine. Iliopsoas abscess can be classified as either primary or secondary. Primary abscess results from hematogenous spread of an infectious process from an occult source in the body. Local trauma with resultant intra muscular hematoma formation seems to predispose to primary iliopsoas abscess formation. The secondary abscess develops by spreading of infection from contiguous anatomical structures, such as gastrointestinal and genitourinary tract, musculoskeletal system, or vascular tissue [2]. We present here two cases of acute necrotising pancreatitis presenting as psoas abscesses.
Case 1
A 40-year- old chronic alcoholic (14 years) male presented to surgery emergency with history of fullness in right flank associated with throbbing pain radiating till right hip and fever for 10 days. Fever was low grade, intermittent and partially relieved on medication. He developed progressive abdominal distension for last 3 days and non passage of flatus and faeces for 1 day. There was no past or family history of TB. On examination, he was conscious, febrile (100.7 F) and had stable vitals (pulse rate 90/minute, blood pressure 108/68 mm Hg). Bilateral Pedal oedema and icterus was also present. Abdominal examination revealed abdominal distension with sluggish bowel sounds. There was a distinct fullness, tenderness and other signs of acute inflammation in the right lumbar region and iliac fossa. There was no spine/renal angle tenderness. Right hip was flexed with mild pain on extension. A clinical diagnosis of right sided psoas abscess with alcoholic liver disease was made. Investigations revealed leucocytosis(18000/mm3), mildly elevated serum amylase and lipase(amylase-248, lipase-189), and deranged Kidney and liver functions tests (blood urea 132 mg%, serum creatinine 2.5 mg%, total bilirubin 4.4g m%, direct bilirubin 2.4 gm%). Liver enzymes were within normal limits. Ultrasound abdomen revealed fatty liver, mild fluid collection in right sided retroperitoneum extending along psoas muscle till its insertion with inflammatory changes in right iliac fossa. There was Moderate ascites. Pancreas was obscured due to bowel gas.
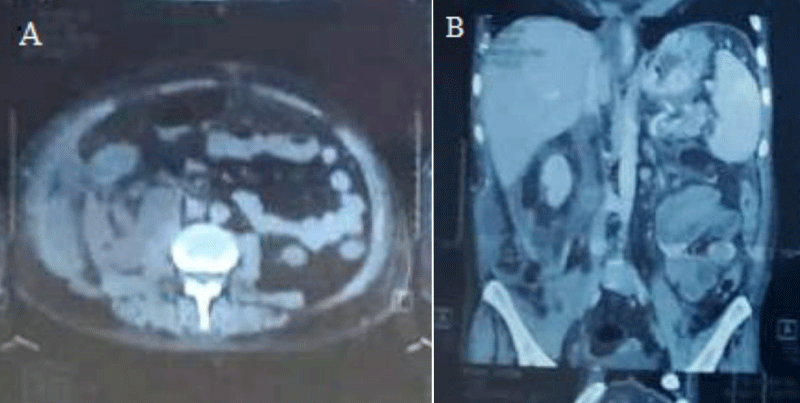
Non contrast Computerized Tomography (NCCT) abdomen (Creatinine raised) was done with the intent to place percutaneous drain. However, it revealed bulky head and neck of pancreas with collection in prehepatic, subhepatic spaces, and in the retroperitoneum along the right perirenal area and psoas muscle. Moderate ascites was also seen. Hence a diagnosis of Acute pancreatitis with peripancreatic infected collection was made (Figure 1A,B). No window could be found for percutaneous drainage (PCN). Patient was optimised with higher antibiotics (Inj Meropenam 500 mg
Figure 1: A) NCCT abdomen axial view showing pancreatic collection. B) NCCT abdomen sagittal view showing pancreatic collection in psoas region.
TDS IV, Inj metronidazole 500 mg IV TDS), Fresh Frozen Plasma (FFP) transfusion to correct INR and taken up for exploratory laparotomy. Midline incision was made. Around 300 ml of Ascitic fluid was present and drain from Intra peritoneal space. Bowel was found healthy. Right colon was mobilised by the Cattel-Braasch Manoeuvre . Frank pus was noted and nearly 600 ml of it was drained from right peri renal and psoas muscle area. Lesser sac was entered via gastrocolic ligament to find pancreatic head and uncinate process parts edematous. A thorough wash and drainage was done in the retro peritoneum. Pus was sent for culture sensitive. Amylase and lipase values of the collection were found to be markedly raised (3860 IU/ml and 2705 IU/ml respectively). Patient was put on broad spectrum antibiotics (Inj Meropenam 1 gm IV TDS, Inj Metronidazole 500 mg IV TDS). The culture showed E. coli and Bacteroides fragilis as pathogens sensitive to meropenam and metronidazole. The same antibiotics were continued for two weeks.
Postoperatively, patient showed good recovery, but continued to have persistent drain output of around 75- 100 ml/day, clear color, watery consistency raising suspicion of low output pancreatic fistula. Drain fluid amylase and lipase were sent and were found to be elevated (1877 IU/ml and 980 IU/ml respectively). Drain was removed and stoma bag was placed. A Contrast Enhanced Computed Tomography (CECT) abdomen was done to look for pancreatic duct status which revealed no ductal dilatation. Patient was discharged on post-operative day 20. The fistula closed in 4 weeks on conservative management. Patient is on regular follow up and has stopped alcohol intake and has had no further episode of pancreatitis till date (one year).
Case 2
A 24-year-old non-alcoholic male presented to the surgical emergency with complaints of fever, associated with chills for 15 days. Fever was associated with a throbbing pain in the left flank with no radiation, and aggravating or reliving factors. He also complained of fullness in left flank for 10 days. He had history of tuberculosis in the family (brother) in recent past. On examination, patient was dehydrated, had fever(101 F) and tachycardia (115/minute). Blood pressure was 100/60 mm Hg. Per abdomen examination revealed fullness in left flank region with tenderness and signs of acute inflammation. Rest of the abdomen was soft with no tenderness, guarding or rigidity. There was flexion deformity of left hip with pain on extension of it. There was no spine/renal angle tenderness. A provisional clinical diagnosis of left psoas abscess was made.
Investigations revealed anaemia (Haemoglobin 9 gm%), leucocytosis (20600/mm3). Liver function test, renal function test and serum amylase and lipase were within normal limits. X-Ray spine was normal. Ultrasound abdomen (USG) revealed a collection with internal echoes along left psoas muscle of 160 ml. Pancreas was obscured because of bowel gas. Empirical broad spectrum antibiotics were started. However, patient did not show clinical improvement over 48hours.
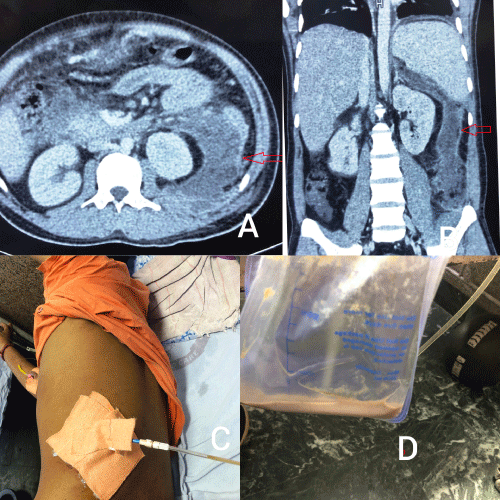
A CECT abdomen was done. It revealed a large collection (13.5 x 6.5 x 10.8 cm) with peripherally enhancing wall seen in pancreatic and peri pancreatic region, replacing body and tail of the pancreas. Laterally, it was extending to the splenic hilum, inferiorly extending to left pararenal space, left paracolic gutter involving left psoas muscle and superiorly till the diaphragm. The collection was displacing the left kidney and descending colon anteriorly. Fat stranding was seen surrounding the collection. Head and uncinate process of pancreas was normal. Pancreatic duct was not dilated. Multiple sub centimetric lymph nodes in mesentery and retro peritoneum were noted. Left sided pleural effusion was seen (pleural separation 1.8 cm). An impression of Acute necrotizing pancreatitis with walled off necrosis (modified CTSI 10) was made (Figure 2A,B).
Figure 2: A) CECT abdomen axial view showing pancreatic collection in perinephric region. B) CECT abdomen in sagittal view showing pancreatic collection in psoas region. C) PCN drain site. D)drain content-infected pancreatic collection.
USG guided per cutaneous drainage (Figure 2C,D) was done to drain the collection which yielded 800 cc of frank pus, followed by daily drainage of around 150 ml for 7 days. Antibiotic was upgraded to Inj. Meropenam 1 gm TDS intravenously and later changed as per culture report. Culture report showed E.coli sensitive to piperacillin- tazobactum. Inj piperacillin –tazobactum 4.5 gm IV TDS was administered for two weeks. Drain was removed on 10th day when the output was minimal and review USG showed minimal collection. The drain amylase and lipase levels were high (amylase 3050 IU/ml, lipase 4100 IU/ml). Patient’s condition improved clinically with subsidence of fever, improved appetite and gradual resolution of pain abdomen. The patient was discharged in stable condition.
Pancreatic necrosis seen about 15% patients of acute pancreatitis and approximately 33% (range 16% - 47%) of these are complicated by infection of necrotic tissue [5]. Necrotizing pancreatitis presents in three configurations: combined pancreatic and peripancreatic necrosis (75%), peripancreatic necrosis alone (20%), and pancreatic necrosis alone (< 5%). The identification of solid necrotic material on imaging is crucial for differentiating acute necrotic collections from acute peri pancreatic fluid collections. Secondary infection of necrotizing pancreatitis is associated with increased mortality and is usually diagnosed at least 2–3 weeks after disease onset. Infected pancreatic necrosis is associated with poor outcomes (mortality rate of 32%) and frequently requires intervention, whereas sterile pancreatic necrosis has a mortality rate of about 12%. The risk of infection is increased in prolonged disease with persistent bacteraemia. Prophylactic antibiotics are usually ineffective, likely because of poor penetration into necrotic tissue [6]. This makes early diagnosis of infective necrotising pancreatitis an imperative for a better outcome as delay will only increase the risk of secondary infection and resultant poorer outcome. Atypical presentations like our cases can cause undue delay in diagnosis and jeopardize outcome.
The Fluid collections subsequent to pancreatitis usually present around pancreas. However, they can also occur in various rare locations in view of retroperitoneal location of pancreas combined with digestive action of pancreatic enzymes. The most commonly involved spaces in these conditions are anterior pararenal space and retromesenteric plane. These fluid may spread posteriorly to involve the retrorenal plane or laterally into the lateroconal plane. At times, the activity can spread inferiorly in the combined interfascial plane to reach up to the pelvic retroperitoneum or superiorly up to the diaphragm or even to enter the mediastinum. These fascial planes provide a weak barrier to the spreading inflammation [7]. Thus any case presenting with collection in these regions should keep necrotising pancreatitis as a differential diagnosis and work up should be done to rule out the same. The collections in some of these regions were revealed by CT scan in our cases along with necrosis of the pancreas. In our cases, we found an association of the location of collections with specific region of pancreas affected by the inflammation. Right sided collection was seen in pancreatitis involving the head and neck region, while left sided collection was noted in pancreatitis involving the body and tail region.
Once a diagnosis of necrotising pancreatitis with collection was made, we followed a step up approach. Per Cutaneous Drainage (PCD) alone was sufficient in one case, while an open drainage was required for the other case due to lack of window for percutaneous drainage. Current guidelines support a step up approach when intervention is necessary, starting with drainage and progressing in invasiveness to surgical necrosectomy. A benefit of the step-up approach is delay of surgery, which has been shown to decrease mortality [6]. The indications for surgery are usually clinical deterioration in a known infected necrotizing pancreatitis and ongoing organ failure for several weeks after the onset of acute pancreatitis in the absence of documented infected necrotizing pancreatitis. In these cases, surgery should be delayed for atleast four weeks for the collections to become walled off. However, intra abdominal catastrophes like haemorrhage, perforation, abdominal compartment syndrome demands immediate surgical intervention if minimal invasive methods like angioembolisation are not available [8].
Traditionally, the success rate of percutaneous drainage alone (defined as survival without the need for additional surgical necrosectomy) ranges from 35% - 84%, with mortality rates ranging from 5.6% - 34%. Morbidity is seen in 11% - 42%, and is most commonly due to pancreatico-cutaneous fistulas and pancreatico-enteric fistulas, which occur in an as many as 20% of cases. Nowadays, percutaneous drainage is more often used as an adjunct therapy, often serving as the first step of a step-up approach to endoscopic or surgical drainage [5]. The Dutch PANTER trial further illustrated this concept by comparing open necrosectomy with a less-invasive step-up approach in 88 patients [9]. The trial results showed that the minimally invasive approach was associated with an overall decreased mortality rate, fewer major and long-term complications, and reduced overall healthcare costs. However, percutaneous drainage alone without subsequent necrosectomy was achieved only in 30% of patients.
However, the PANTER trial did not evaluate the efficacy of Direct Endoscopic Necrosectomy (DEN). The Kumar, et al. [10] study compared the DEN vs step up approach, concluded the DEN may be superior approach as in his study the clinical resolution after DEN was 92% compared to 25% after initial PCD, with 75% of step up patients requiring surgical intervention. Given higher efficacy, lower morbidity, shorter length of stay, and lower health care utilization, DEN could be the first-line therapeutic modality. The step-up approach using initial PCD remains useful in patients with immature necrotic collections, or collections that are inaccessible by DEN. More studies/Randomised controlled trails (RCTs) needs be done to formulate an effective approach to manage pancreatic collections.
A prompt diagnosis and a step-up approach towards managing infected pancreatic collections is crucial to a successful outcome. As illustrated by our cases, a differential diagnosis of acute pancreatitis with infected collections should be kept as a possibility while managing psoas abscesses.
A prompt diagnosis and a step-up approach towards managing infected pancreatic collections is crucial to a successful outcome. As illustrated by our cases, a differential diagnosis of acute pancreatitis with infected collections should be kept as a possibility while managing psoas abscesses.
- Nadhem O, Salh O. Acute pancreatitis: an atypical presentation. Case Rep Gastroenterol. 2017; 11: 359-363. PubMed: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5471751/
- Jain VK, Hadiyal A, Jolly S. Unusual presentation of pancreatic pseudocyst as a psoas abscess. International Surgery Journal. 2019; 6: 1395-1399.
- Moens L, YengueYengue P, Assenmacher C. Intrascrotal collection in an acute pancreatitis: a case report and review of the literature. Case Rep Urol. 2016; 2016. 7534781. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/27882260
- Kamble PM, Patil A, Jadhav S, Rao SA. Anterior abdominal wall abscess with epididymo-orchitis: An unusual presentation of acute pancreatitis. J Postgrad Med. 2011; 57: 335-337. PubMed: https://pubmed.ncbi.nlm.nih.gov/22120865/
- Tyberg A, Karia K, Gabr M, Desai A, Doshi R, Gaidhane M, Sharaiha RZ, Kahaleh M. Management of pancreatic fluid collections: A comprehensive review of the literature. World J Gastroenterol. 2016; 22: 2256-2270. PubMed: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4735000/
- Zhao K, Adam SZ, Keswani RN, Horowitz JM, Miller FH. Acute pancreatitis: revised Atlanta classification and the role of cross-sectional imaging. AJR Am J Roentgenol. 2015; 205: W32-41. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/26102416
- Palanati V, Santhosh Anand KS, Thirunavukkarasu S, Munikrishna S, Reddy S, et al. Psoas Abscess-An Unusual Presentation of WOPN. World J Surgical Res. 2018; 1: 1083.
- Working GI, APA AP. IAP/APA evidence-based guidelines for the management of acute pancreatitis. Pancreatology. 2013; 13(4 Suppl 2): e1-15. PubMed: https://pubmed.ncbi.nlm.nih.gov/24054878/
- Besselink MG, van Santvoort HC, Nieuwenhuijs VB, Boermeester MA, Bollen TL, et al. Minimally invasive ‘step-up approach’versus maximal necrosectomy in patients with acute necrotising pancreatitis (PANTER trial): design and rationale of a randomised controlled multicenter trial [ISRCTN13975868]. BMC Surg. 2006; 6: 6. PubMed: https://pubmed.ncbi.nlm.nih.gov/16606471/
- Kumar N, Conwell DL, Thompson CC. Direct endoscopic necrosectomy versus step-up approach for walled-off pancreatic necrosis: comparison of clinical outcome and health care utilization. Pancreas. 2014; 43: 1334-1339. PubMed: https://pubmed.ncbi.nlm.nih.gov/25083997