INTRODUCTION
Shoulder instability is a common injury with a range of presentations. Attempts to classify shoulder instability commonly include three primary descriptors that depict the severity and mechanism of injury.1 Traumatic shoulder dislocation generally describes structural injury linked to a specific destabilizing event. Microtraumatic subluxations often include structural damage but are not tied to any specific event. Atraumatic instability is not tied to a specific incident and is often linked with altered neuromuscular control, systemic laxity, or anomalies of body structure.
Glenohumeral dislocations are straightforward to diagnose with radiographs in acute assessment and advanced imaging to determine additional tissue injury as needed. The incidence of glenohumeral dislocations has been reported as high as 23.9 (95% CI: 20.8 to 27.0) per 100,000 person-years and a lifetime prevalence between 2-8% in the general population in the United States.2–4 Risk factors for acute (mostly anterior) dislocation have been identified and include age, sex, sport participation, immobilization protocol, and glenoid shape.5–12
Instability associated with microtrauma or atraumatic instability is more difficult to diagnose and may present with a range of symptoms from the feeling of looseness or instability to humeral subluxation with immediate reduction.13 The incidence of glenohumeral instability is therefore more difficult to measure.14 Risk factors for instability not associated with dislocation have been infrequently investigated.
Once the diagnosis of glenohumeral instability has been confirmed, management may include surgical stabilization, bracing, and physical therapy.15 Injuries involving glenohumeral instability are associated with high medical costs (with ranges between $973 to $7,800) depending on the complexity and potential surgical interventions.15
Despite the frequency of GH shoulder instability, many unknowns remain regarding risk factors. No consensus exists regarding identifiable risk factors that may be beneficial for physicians and rehabilitation professionals to discern either prevention or appropriate management strategies. Furthermore, the authors are unaware of any systematic review that has investigated risk factors associated with all types of instability, not just shoulder dislocation. Thus, the purpose of this systematic review was to identify modifiable risk factors to guide patient management decisions with regards to implementation of interventions to prevent or reduce the risk of shoulder instability.
MATERIALS AND METHODS
Search Strategy
This systematic review was performed following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines.16 The protocol for this systematic review was sent for registration a priori to the International Prospective Register of Systematic Reviews (PROSPERO). However, it was “rejected” because “PROSPERO was focusing on COVID-19 registrations during the pandemic.” This registration was automatically rejected because it did not meet all acceptance requirements (i.e. not Covid related). Therefore, the authors registered the protocol in the Open Science Framework. This registration describes all the methods used in this systematic review.
An research librarian with greater than 30 years of experience performed a systematic search in compliance with PRISMA protocol in October of 2022 and again in March of 2023 in the following databases from the time of their inception: PubMed, EMBASE, Cochrane, CINAHL, Web of Science Core Collection, and SportDiscus databases. Search terms (Appendix 1) were developed along with guidance from the librarian and included a combination of the following: shoulder, shoulder joint, glenohumeral joint, instability, dislocation, subluxation, hyperlaxity, prevalence, incidence, risk ratios, and odds ratios. The librarian was not an author or investigator of the review. Filters included human subjects and published in the English language. Date restrictions were not applied.
Once the search was complete the librarian imported citations into Covidence software which eliminated any duplicates from multiple databases. Studies were included if they were prospective and retrospective cohort studies which investigated risk factors associated with first time or recurrent shoulder instability defined as dislocation, subluxation, or other symptoms of instability either alone or together. Anterior, posterior, and multidirectional instability were all included as were all mechanisms of injury including both traumatic and atraumatic. A diagnosis of instability had to be confirmed with a reference standard of surgery, diagnostic imaging, or required reduction, and a history of prior dislocation for the recurrent instability group. Studies had to include an analytical component (ie, the study examined the relationship between risk factor and shoulder instability), or sufficient data for these to be calculated. All studies needed to be published in the English language. Studies were excluded if they did not meet the above criteria, when subjects had co-existing conditions (e.g., Ehlers-Danlos syndrome), neurological conditions (e.g., Stroke), syndromes, or congenital conditions (e.g. skeletal dysplasia) as well as studies investigating risk factors of instability following surgical intervention. Search strategies along with the number of citations captured in each search are displayed in Appendix 1. Bibliographic reference lists from identified articles were hand searched for any other potential study not identified during the database searches.
Study Selection
After the duplicate articles from the different databases were removed, two independent reviewers screened titles and abstracts to determine which studies might possibly meet the eligibility criteria. Studies that appeared to satisfy the inclusion/exclusion criteria or whose eligibility could not be determined from the title/abstract screening were retrieved for full-text review. All retrieved studies were independently reviewed by at least two named authors. Disagreements between reviewers were resolved by consulting a third author who was blind to other reviewers’ decisions on whether the study should be included.
Data Extraction and Quality Assessment
All six authors used a standardized data extraction form to collate the following information: Author and the year of the study, study design (cohort or case-control) sample size, age, sex, description of shoulder instability reported in the study, refence standard used to determine instability, risk factors and odd ratios or relative risk. If odds ratios or risk ratios were not provided, but summary injury data were provided, ratios were calculated by the authors of this manuscript.
All reviewers examined the quality studies using the Newcastle-Ottawa Scale (NOS) which has been shown to be both reliable and valid for examining longitudinal and case-control studies.17,18 The NOS evaluates three quality parameters (selection, comparability, and outcome) divided across eight specific items, which slightly differ when scoring case control and longitudinal studies.19 A study can be awarded a maximum of one star for each numbered item within the selection and exposure categories. A maximum of two stars can be given for comparability. Thus, the maximum for each study is 9, with studies having less than 5 points being identified as representing a high risk of bias.19
Using previously reported recommendations regarding strength of association with likelihood ratios,20 the reported risk factor strength of associated odds ratios was classified as shown in Table 1.
RESULTS
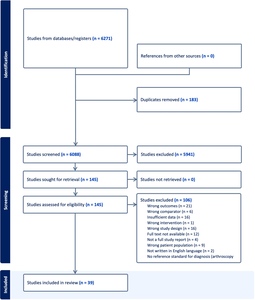
The initial search strategy (Appendix 1) identified 6271 citations potentially eligible for this systematic review. After 183 duplicates were eliminated a total of 6088 citations remained. Of these 6088 underwent title and abstract screening. A total of 147 articles were selected for full text review with 395–12,21–51 included in the final review. (Figure 1) Of those 39 studies, 18 focused on first time shoulder instability (Appendix 2), 18 focused on recurrent instability (Appendix 3), and three studies reported on both.5,11,51 Of the 21 studies reporting on first time shoulder instability, 19 were classified as dislocation and/or subluxation and two were classified as shoulder instability. Of those 19 studies reporting on first time dislocation and/or subluxation, five studies reported on anterior dislocation and/or subluxation, three studies reported on posterior dislocation and/or subluxation; seven studies reported on mixed populations or multidirectional dislocation and/or subluxation; and four studies did not report on the direction of shoulder dislocation and/or subluxation. Of the two studies reporting on shoulder instability, both were in the anterior direction. Of the 21 studies reporting on recurrent shoulder instability, all 21 studies were classified as dislocation and/or subluxation. Of those 21 studies, 12 reported in the anterior direction; two in the posterior direction; six on mixed populations or multidirectional dislocation and/or subluxation; and one study did not report on the direction of recurrent shoulder dislocation and/or subluxation. Figure 1 represents the flow diagram of study inclusion. The results of the quality assessment are shown in Table 2. Of the 39 included studies, five7,24,44,45,48 scored less than 5/9 rating them at high risk of bias. Most methodological shortcomings concerned comparability of cases and controls, specifically controlling for a second variable that could have a mediating effect; clear definition of controls; and report of non-response rate and adequacy of follow up of cohorts.
Risk Factors Associated with First Time Shoulder Instability (Appendix 2)
Sports Participation
Of the total number of studies included reporting on risk factors associated with first time shoulder instability, 24% (5/21) were related to sports participation.5,9,11,36,48 Of these studies one48 scored 2/9; three5,11,36 scored 6/9; and one9 scored 8/9; on the Newcastle Ottawa Risk of Bias Report (NRoB).17,18 (Table 2) Based on the current findings it is possible that the type of sport an individual participates in may increase the risk for first time shoulder dislocation. Participation in sports including skiing and snowboarding,36 and both intercollegiate and intramural male wrestling9 demonstrated a moderate to large risk for experiencing a shoulder dislocation. Additionally, studies examining the risk of individuals playing football5,9 found moderate associations with participation in the sport.
Participation in other sports demonstrated a smaller risk of shoulder dislocation include rugby, boxing, American football, lacrosse, and Judo.5,11,48 Interestingly, one study11 found sports such as wrestling, indoor obstacles, fitness testing, and swimming to have a protective effect against shoulder dislocation. These findings should be interpreted with caution they are from only one dataset in a population of students attending a United States Military academy.
Four5,11,36,48 out of five9 of the included studies were from mixed populations suggesting that participation in sport is not unique to a particular direction of shoulder instability.
Anatomical Variations
The risk factor of anatomical variation contributing to first time shoulder instability was studied in 5/21 (24%) of included manuscripts. Of the studied anatomical variations, risk related to increased glenoid index (GI), or the glenoid height to width ratio, was included in three manuscripts and was reported as a moderate (((OR = 7.88 (CI: 2.14, 29.13))8 and ((OR = 8.12 (CI: 1.07-61.72)))10 to large ((OR = 16.71 (CI: 4.26,65.62))51 risk factor. Notably, the large risk was identified by a study that used a lower (>1.45) GI compared to the others which used >1.6. Of the studies that investigated GI, two8,10 scored 6/9 on the NRoB while the study that reported large related risk scored a 7/9.51 Of these studies, all risk factors were reported in anterior shoulder dislocation and/or subluxation populations.
Four other anatomical variations were found in studies that met the search criteria. Two variations, humeral containing angle >64 degrees8 and coracohumeral interval,10 had minimal association with risk yielding OR’s of <1.20 in those with anterior dislocation and/or subluxation while there was a small association between glenoid dysplasia and injury ((OR = 2.84, CI: (1.14, 7.09) in those with posterior dislocation and/or subluxation.7 Regarding glenoid retroversion, three studies7,10,37 included this variation. Two studies resulted nearly identical OR’s of 1.157 and 1.1737 (CI: 1.14, 1.16 and CI: 1.03, 1.34) in those with posterior dislocation and/or subluxation while one determined there to be a small risk ((OR = 4.83, (CI: 1.75, 13.33)) in those with anterior dislocation and/or subluxation.10 With the exception of the single study that investigated glenoid dysplasia7 which scored 4/9 on the NRoB, other studies scored either 6/9 or 7/9.
Sex
Of the six out of the 21 papers that examined the risk of first time shoulder instability on the basis of sex,6,9,35,36,44,46 males exhibited a greater risk for first time shoulder dislocation compared to females in all studies. Of these studies, the NRoB Report scores ranged from 3-9 (out of 9) with a median score of 5.5. The strength of association between male gender and risk for first time shoulder dislocation ranged from minimal/small6,9,35,36,46 to large.44 Included studies were representative of all shoulder instability types, severity, and direction making it impossible to link sex to any specific shoulder instability type.
Age
Relative to those ≥35 years of age, a moderate association was observed between younger age (15-19) and risk for first time shoulder dislocation, OR 7.4 (95% CI: 2.7, 20.7), while the ORs were relatively less (ORs: 1.0-3.7) for patient groups between 20-34 in the same study.46 Older age (≥65) had a small association with increased risk for first time shoulder dislocation compared to those aged < 65 in one study.35
In the study by Syzluk,12 the ORs were calculated for males relative to females across nine different age groups separated into ten-year increments, where the ORs ranged from 0.62 (80-89 years old) to 7.49 in the 20-29 age group. When examining this study based on risk by age group, 0-9 years old and 10-19 years old demonstrated a small to large protective effect for first time shoulder dislocation.12 All included studies were representative of those with shoulder dislocation and/or subluxation but populations were mixed regarding direction.
Laxity, Motion, and Strength Measures
Hypermobility and shoulder range of motion were investigated in one, small (n = 57 cases) retrospective case control study for their association with acute, first-time traumatic shoulder dislocations.23 Hypermobility was assessed by the Hospital del Mar criteria,52 which measures the degree of passive hypermobility across ten joints. Regardless of sex, a score of >4/10 for males and >5/10 for females on the Hospital del Mar scale was found to be statistically significant in predisposing an individual to shoulder dislocation risk OR = 2.79 (95%: CI 1.27, 6.09) in this lower quality study (NRoB = 5/9).23 The association of hypermobility and dislocation was statistically significant when combined with greater than 85 degrees of external rotation at the shoulder ((OR = 3.6 (95% CI: 1.49, 8.68)).23 When sex was analyzed separately, hypermobility had a moderate association with first-time shoulder dislocation for both males (OR= 7.43, 95% CI: 2.13, 25.57) and females ((OR = 8.36 (CI:1.08, 61.10)). Combining shoulder external range of motion greater than 85 degrees to the hypermobility score resulted in similar, moderate associations with shoulder dislocation risk, but only in males ((OR 6.75 (CI 1.92, 23.36)).23 This study is specific to those with first time anterior shoulder dislocation and/or subluxation.
Strength as a risk factor for first time shoulder dislocation was investigated in two studies. Internal and external rotation shoulder strength at various degrees of shoulder abduction had minimal association with shoulder dislocation that did not reach statistical significance, as assessed by hazard ratios.37,39 One study investigating the association between strength and instability boasted a “good quality” rating (Table 2) and a large cohort size (n = 1,428),39 whereas the other failed to report critical data and was received a “fair” quality rating.37 These studies included both anterior and posterior first time shoulder dislocation and/or subluxation making it difficult to link strength to any particular direction of shoulder instability.
Urban or Rural living
One population-based study12 from Poland examined glenohumeral dislocation rates between urban and rural areas. Overall incidence and risk of first time dislocations did not differ based on area of residence (25.97 vs 25.62 per 100,000 person-years in rural vs urban communities respectively, OR = 1.01 (0.97-1.05)). Risk of shoulder dislocation when incorporating age and gender is highest in rural areas for females aged 70-79 years (OR = 4.17, (4.17–5.33)) whereas the highest risk in urban areas is in females aged 80+ years (OR = 5.07 (4.58–5.61)). The greatest disparity between rural and urban areas is among females aged 0-9 years where the odds ratio = 20.39 (CI 8.25-50.4) for females living in rural areas compared to females living in urban areas. The study population was not reported in this study in terms of direction of shoulder dislocation and/or subluxation.
Risk Factors Associated with Recurrent Shoulder Instability (Appendix 3)
Sport Participation
Of the total number of studies included reporting on risk factors associated with recurrent shoulder instability, 9.5% (2/21) were related to sports participation. The Amako et al. and Owens et al. studies both scored 6/9 NRoB Report.5,11 These two studies suggest that participation in sport may pose a minimal risk for recurrent shoulder dislocation. Specifically, participation in rugby, American football, and Judo sports demonstrated a small to minimal risk of recurrent shoulder dislocation. Owens11 reports a large association between skiing/snowboarding and ice hockey with shoulder dislocation. Included studies were from mixed populations suggesting that participation in sport is not unique to a particular direction of recurrent shoulder instability.
Sex
Gender as a risk factor was described in 32% (6/19) of studies that reported on risk of recurrent instability,25,26,29,30,34,41 with NRoB Report scores ranging from 6-9 out of 9. As compared to females, males were identified to be at greater risk for recurrent instability in five of the six studies (83%).25,29,30,34,41 A moderate association with recurrent instability according to male gender was reported by one study25 which identified an OR of 7.21 (95% CI: 2.84, 18.27). A majority of included studies referred to patients suffering from recurrent anterior shoulder dislocation and/or subluxation with two reporting on mixed populations.
Age
Of the total number of studies reporting on risk of recurrent glenohumeral dislocations, 58% (11/19) reported on patient age as a risk factor.21,25,26,29,30,32,34,40,41,43,47 The NRoB Report scores for each study are reported in Table 2. The strongest associations with risk of recurrent shoulder instability were identified in four studies, which demonstrated a moderate-large association with age as a risk factor.25,32,34,40 ORs for individuals less than 30 years old were reported by Hoelen25 and Lill32 at 20.22 (95% CI: 8.34, 48.51) and 22.67 (95% CI: 7.76, 70.81), respectively, and for those under 20 years old was 6.75 (95% CI: 1.19, 38.41) as described by Murray.34 One study47 examining younger age found an inverse association with risk of recurrent dislocation primarily for individuals in the 0-9 age group, where ORs ranged from 0.07 - 0.24. Included studies were representative of all directions of recurrent instability making it impossible to link age to any particular direction of recurrent shoulder instability.
Sociodemographics
Only two studies considered elements of sociodemographics as a risk factor for recurrent shoulder instability.26,30 The three elements investigated were marital status, socioeconomic status, and educational level. None of these elements were found to have more than minimal association with OR’s between .80 and 1.23.
Prior history with concomitant injury
Prior history of glenohumeral dislocation with or without concomitant injury was reported as a risk factor for recurrent shoulder dislocation in five (26%) of the nineteen studies.22,26,30,33,50 The strength of these associations ranged from minimal to large. Each of the five studies looked at a different type of prior shoulder injury history from prior history of glenohumeral instability and rotator cuff tears33 to instability and axillary nerve injury.26 The largest association with recurrent shoulder dislocation included a history of instability alongside of rotator cuff injury in those with recurrent anterior shoulder instability33 with OR of 10.8 (CI: 3.1, 37.9), and a history of instability and posteroinferior defect with crandiocaudal length of >12mm in those with recurrent posterior instability50 with OR of 32.5 (CI 5.53, 191.09). Both of these studies were high quality with NRoB scores of six and eight, respectively (Table 2); the strong association with shoulder instability as reported by Weishaupt et al. 2000 should be interpreted with caution given the small sample size (n = 45, with 15 exposed cases). Of the remaining risk factors related to prior shoulder injury, a self-reported prior history of posterior glenohumeral instability was the only risk factor with a moderate association (OR 8.67 CI 1.81, 41.59) from a high-quality study (NRoB = 9/9).22 This study included a mixed population of anterior, posterior, and multidirectional instability.
Anatomical Variations
The risk factor of anatomical variation contributing to recurrent shoulder instability was studied in 1/21 (4.8%) of included manuscripts and did not differentiate between first time or recurrent shoulder instability. As reported above, Yellin51 reports a large association (OR = 16.71 (4.26, 65.62) between the glenoid index > 1.45 and risk of recurrent anterior shoulder instability.
Other (manual work, immobilization, CADG, physician specialty)
“High-risk” manual laborers are at increased risk of recurrent dislocation compared to more sedentary professions (e.g. office work).33 This study with a NRoB score of 6/9 attributed the increased risk (OR 4.3 (1.2,15.5)) due to the loads applied during work (bricklayer, paratrooper, firefighters, etc.) Manual laborers’ risk was also measured in one other study (NRoB = 7/9) that reported a similar risk of recurrent dislocation (OR: 1.39 (0.55,3.51)) to a group of non-manually intensive professions.49 Both of these studies were specific to those suffering from recurrent anterior shoulder dislocation and/or subluxation.
The position of immobilization (internal vs external rotation) following first-time dislocation was reported in three studies.24,31,34 Risk of recurrent shoulder dislocation based on immobilized position was similar [OR: 2.23 (0.67,7.4), 1.75 (0.61,5.04)} in two high quality (NRoB scores: 8/9) studies of anterior and mixed direction recurrent shoulder dislocation and/or subluxation.31,34 The third lower quality study (NRoB score: 2/9) showed a risk reduction (OR 0.08 (0.02,0.38) when immobilized in abduction with external rotation in those with recurrent anterior shoulder dislocation and/or subluxation.24
The odds of recurrence were compared by the providers performing the closed reduction in two high-quality studies from one large epidemiological investigation.29,30 Orthopedic surgeons were compared to other specialties. In pediatric patients, aged 10-16 years, there was no difference in recurrence rate (OR: 0.69 (0.43-1.07)) whereas in adult patients, aged 16-70 years, the risk of recurrence was lower in patients with recurrent anterior shoulder dislocation and/or subluxation (HR: 0.76 (0.64-0.90) when orthopedic surgeons performed the reduction compared to other providers.
Patient’s overall health, utilizing combined aggregate diagnostic groups (CADG),53 was compared between patients with fewer (0-4) comorbid health conditions and patients with ≥ 5 comorbid health conditions.30 Patients with higher comorbidity were found to have a lower risk (HR: 0.92 (0.87, 0.98) of recurrent anterior shoulder dislocation and/or subluxation compared to patients with fewer comorbidities in one high-quality study.30 Comorbidity was defined as any number of 12 disease categories based on ICD-9 and ICD-10 codes.
DISCUSSION
The results of this study shed light on several key risk factors associated with both first-time and recurrent shoulder instability.
Sports Participation: A moderate to large risk of first-time shoulder dislocation was observed in individuals participating in sports such as skiing, snowboarding, intercollegiate and intramural male wrestling, and football. Conversely, sports like rugby, boxing, American football, lacrosse, and Judo showed a smaller risk. Notably, certain sports like wrestling, indoor obstacles, fitness tests, and swimming demonstrated a protective effect against shoulder dislocation. However, caution is warranted due to the limited dataset and specific population demographics. Patient education is important in helping athletes understand the potential risk of participating in some sports over others.
Anatomical Variations: An increased glenoid index (GI) was associated with a moderate to large risk of first-time shoulder instability, particularly in anterior dislocation populations. When this ratio is increased the morphology of the glenoid is that it is taller and narrower, decreasing the contact area of the joint which results in greater instability compared to joints with lower glenoid height to width ratios. One hypothesis is that infants who fail to crawl properly lack the necessary weightbearing to further develop the glenoid height to width ratio placing them at increased risk for shoulder dislocation later in life. Further research is needed to explore this hypothesis and potentially support the need for early intervention to reduce the incidence of shoulder instability later in life. Other anatomical variations such as humeral containing angle, coracohumeral interval, glenoid dysplasia, and glenoid retroversion showed minimal to small associations with dislocation risk.
Sex and Age: Males exhibited a greater risk of both first-time and recurrent shoulder instability compared to females. Younger age groups, especially those between 15-19 years old, demonstrated a moderate association with first-time shoulder dislocation. Conversely, older age groups (≥65 years) showed a small association with increased risk.
Laxity, Motion, and Strength Measures: Hypermobility, particularly in combination with excessive shoulder external rotation, showed a significant association with first-time shoulder dislocation, especially in males. However, the quality of evidence for this association was limited. Measures of strength, including internal and external rotation shoulder strength, demonstrated minimal associations with shoulder dislocation.
Urban or Rural Living: Interestingly, urban versus rural living did not significantly affect the overall incidence or risk of shoulder dislocation, although certain age and gender demographics showed variations in risk across different residential settings.
Other Factors: Factors such as manual labor, immobilization position, and the specialty of medical providers performing reduction procedures also influenced the risk of recurrent shoulder instability. Additionally, patients with a higher number of comorbid health conditions showed a decreased risk of recurrence compared to those with fewer comorbidities. This finding could potentially be contributed to the idea that those with additional comorbidities may be less active thus reducing the number of exposures to activities attributed to shoulder instability.
Overall, understanding these risk factors can inform targeted strategies for prevention and management of shoulder instability, potentially improving patient outcomes and guiding clinical decision-making. However, further research is needed to validate these findings and elucidate the underlying mechanisms driving these associations.
Study Limitations
There are a number of limitations with this systematic review. Despite the authors’ best intentions, studies meeting inclusion criteria were dominated by a diagnosis of shoulder dislocation and/or subluxation. Only two included studies reported on less severe symptoms of shoulder instability making it impossible to report on risk factors associated with less severe yet inhibiting shoulder instability. The lack of studies assessing instability may be related to the challenges or controversies in diagnosing instability (vs. dislocation).13 Intersectionality, specifically age and gender was not clearly delineated in many of the studies which could potentially limit the generalizability of the results. Three of the included studies did not differentiate between first time and recurrent shoulder instability. Additionally, cohort sizes varied amongst the studies which would be expected considering the number of variables examined would have a direct impact on the necessary sample sizes to achieve adequate power and narrow confidence intervals. Another limitation was that fewer studies examined predictors for first time shoulder dislocation or recurrent instability for females versus males. Furthermore, ORs were not provided in every study. Although the authors attempted to calculate those for each study it was evident that insufficient data was provided in many of them to do so.
Additional limitations include the quality of studies identified. For first time shoulder instability, two studies scored 2/9; one scored 3/9; two scored 4/9; four scored 5/9; six scored 6/9; two scored 7/9; one scored 8/9; and three scored 9/9 on the NRoB. For recurrent shoulder instability, one study scored 2/9; two scored 5/9; six scored 6/9; four scored 7/9; three scored 8/9 and three scored 9/9. Results of this systematic review suggested higher quality studies were reported as part of recurrent shoulder instability as compared to first time shoulder instability. The reference standard utilized in the studies was not consistent nor were the age norms. As a result of the heterogeneity, a meta-analysis was unable to be performed.
CONCLUSIONS
The results of this systematic review suggest there may be a number of predictive variables for first time dislocation or recurrent dislocations. Male sex, participation in sport, hypermobility in males, and glenoid index demonstrated moderate to large risk associated with first time shoulder instability. Male sex, age < 30 years, and prior history of glenohumeral instability with concomitant injury demonstrated moderate to large risk associated with recurrent shoulder instability. However, the quality of included studies was mixed with higher quality studies reported in populations with recurrent shoulder instability. Therefore, it is necessary to perform additional studies to determine if the findings are consistent with well-designed prospective studies. An opportunity may exist for patient education in particular populations as to their increased risk for suffering shoulder instability, particularly in young males who appear to be at increased risk for recurrent shoulder instability.
Conflict of Interest
The authors declare no conflicts of interest in the creation of this manuscript.