- Department of Neurology, Papageorgiou Hospital of Thessaloniki, Periferiaki Odos N. Efkarpia, Thessaloniki, Central Macedonia, Greece.
- Department of Neurosurgery, Papageorgiou Hospital of Thessaloniki, Periferiaki Odos N. Efkarpia, Thessaloniki, Central Macedonia, Greece.
Correspondence Address:
Efthymia Samara
Department of Neurology, Papageorgiou Hospital of Thessaloniki, Periferiaki Odos N. Efkarpia, Thessaloniki, Central Macedonia, Greece.
DOI:10.25259/SNI_886_2020
Copyright: © 2021 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Efthymia Samara1, Ioannis Siasios2, Konstantinos Katsiardanis1, Eirini Liaptsi1, Kalliopi Tsoleka2, Georgia Deretzi1. Brain abscess in a rheumatoid arthritis patient treated with leflunomide – A case presentation and review. 17-Mar-2021;12:97
How to cite this URL: Efthymia Samara1, Ioannis Siasios2, Konstantinos Katsiardanis1, Eirini Liaptsi1, Kalliopi Tsoleka2, Georgia Deretzi1. Brain abscess in a rheumatoid arthritis patient treated with leflunomide – A case presentation and review. 17-Mar-2021;12:97. Available from: https://surgicalneurologyint.com/surgicalint-articles/10654/
Abstract
Background: Immunosuppression is a significant parameter in the pathogenesis of brain abscesses (BA) and it could be the result of severe infections such as acquired immunodeficiency syndrome or drug-induced, by several medications used for systemic autoimmune diseases. Leflunomide is a pyrimidine synthesis inhibitor that affects the proliferation of lymphocytes and is used as a disease-modifying antirheumatic drug. Mild infections, particularly those of the respiratory tract and herpes zoster, are one of its most common adverse effects. However, atypical and severe infections have also been reported under treatment with leflunomide.
Case Description: A 70-year old female was referred to our hospital with headache, aphasia, and right-sided hemiparesis and a lesion of the left parietal lobe initially interpreted as a malignancy. Her medical history revealed a 12-year old history of rheumatoid arthritis under current treatment with leflunomide. A cerebral magnetic resonance imaging (MRI) revealed typical findings for a BA. She subsequently underwent a left craniotomy, which confirmed the MRI-based diagnosis. The abscess was evacuated and cultures were obtained intraoperatively. In the postoperative examination, the patient showed no neurological deficit.
Conclusion: The differential diagnostic considerations in immunocompromised patients with neurologic deficits should include focal central nervous system infections such as a BA, even in the absence of fever or immunosuppressant-induced leukopenia. It also demonstrates the importance of early neurosurgical intervention for the prevention of sequelae. To the best of our knowledge, this is the second-to-date reported case of a BA under immunomodulatory therapy with leflunomide.
Keywords: Brain abscess, Infections, Leflunomide, Rheumatoid arthritis
INTRODUCTION
Brain abscess (BA) is an intracranial, potentially lethal, space occupying inflammatory lesion with an estimated incidence of 0.3–1.3 per 100,000 people yearly in northern societies.[
Trauma or commonly performed neurosurgical procedures have been associated with the emergence of BA by either direct contiguous microbial spread or hematogenous spread, while in almost 40% of the published cases the cause remains unknown.[
In addition, the literature supports that immunosuppression is also a significant parameter in the pathogenesis of BAs. Immunosuppression could be the result of severe infections such as acquired immunodeficiency syndrome or drug-induced, by several medications used for systemic autoimmune diseases, such as corticosteroids, calcineurin inhibitors, mTOR inhibitors, tumor necrosis factor (TNF) inhibitors, monoclonal antibodies, and antiproliferative agents. Leflunomide is a pyrimidine synthesis inhibitor that acts as an immunomodulator by affecting the proliferation of lymphocytes and is used in the treatment of active Rheumatoid and Psoriatic Arthritis. Susceptibility to infections, particularly those of the respiratory tract and herpes zoster, is one of its most common adverse effects and is mostly associated to leucopenia.
Here, we present the case of a 70-year-old woman with a known history of rheumatoid arthritis (RA) under treatment with leflunomide, who was referred to our hospital of tertiary care with headache, aphasia, right-sided hemiparesis, and a left parietal lesion which was initially misdiagnosed as central nervous system (CNS) malignancy.
CASE PRESENTATION
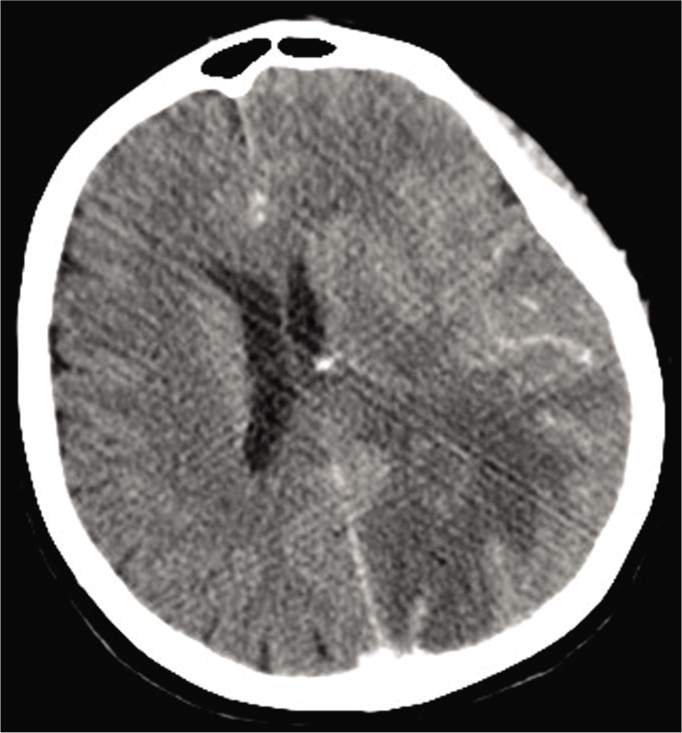
A 70-year old female was admitted to an outside hospital with a 14-days history of headache, dizziness, and a mild aphasia. A CT scan was performed [
On admission at the emergency department and later on at the clinic, the patient had a Glasgow Coma Scale of 14/15 (Eyes:4, Verbal: 4, Movement: 6) with a mild aphasia, a right-sighted hemiparesis, and neglect.
Her previous medical history revealed that she was diagnosed with RA at the age of 58 years old and was receiving orally 20 mg of leflunomide per day. She had been treated with methotrexate and hydroxychloroquine in the past, under which she had experienced many relapses that required oral corticosteroids. It was only when her antirheumatic therapy was switched to leflunomide that she had a long-term remission. The last time she had received oral corticosteroids was 3 years ago for a period of 6 months.
Initial laboratory studies were normal, apart from a slightly elevated C-reactive protein (CRP) (CRP: 4.7 mg/dl, normal range: <0.5 mg/dl) with a normal white blood cell count (WBC: 6,9 × 103/μl) and no history of fever.
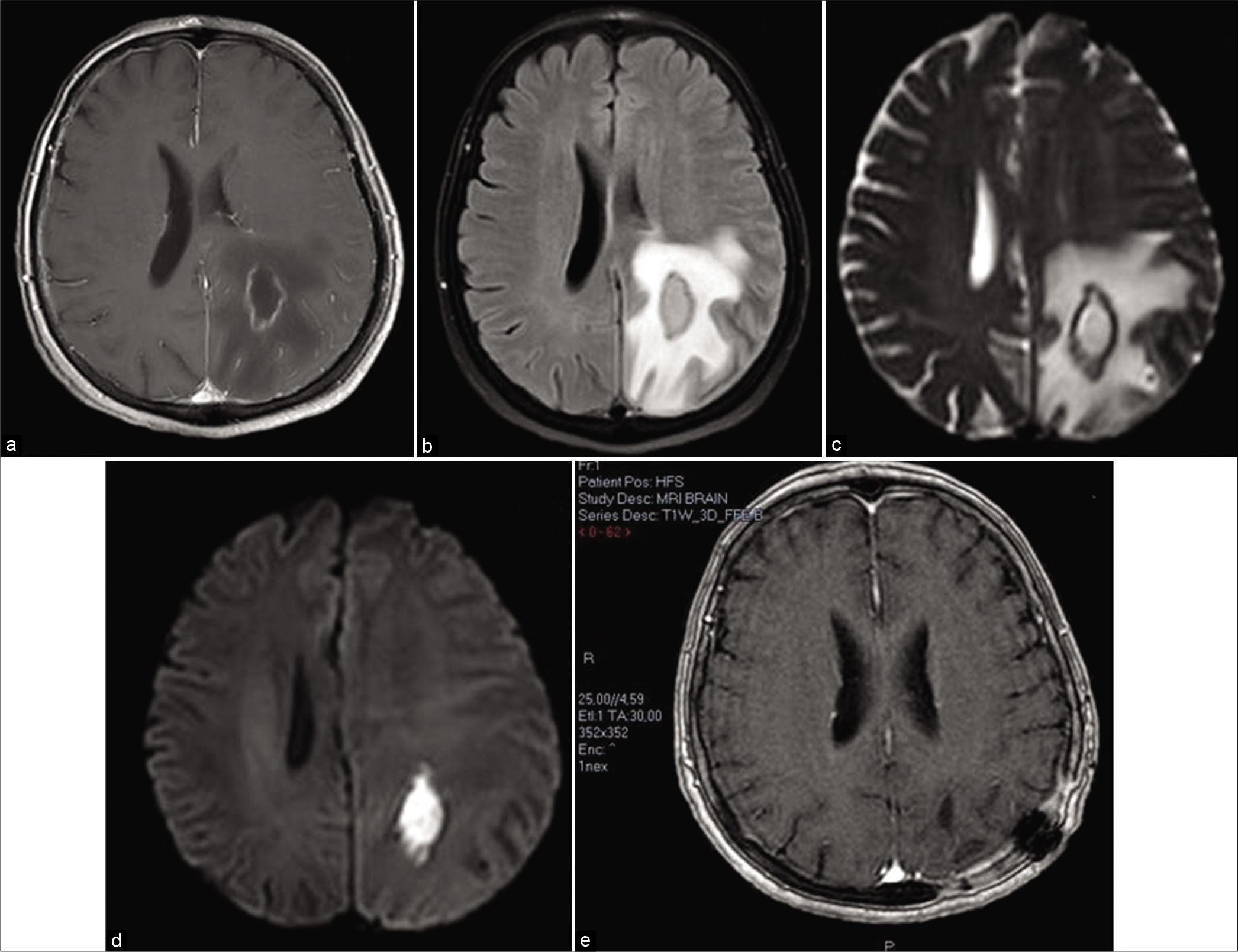
In the next 48 h a single fever wave of 39°C was documented, followed by subfebrile body temperatures, and a slight deterioration of her speech and orientation. A brain MRI demonstrated a left parietal, rim-enhancing collection of fluid with diffusion restriction and dimensions of 48 mm × 25 mm × 19 mm that resembled a BA [
Figure 2:
Axial brain MRI images demonstrate a rim-enhancing (a), collection of fluid which does not attenuate on FLAIR (b), with true diffusion restriction (c and d), indicative of a brain abscess. Postoperative image (e) was acquired 2 months after evacuation and demonstrates no signs of fluid collection or gadolinium enhancement.
Seven days postoperatively only a slight paresis of patient’s right upper extremity remained. The patient was discharged 6 weeks after her surgery and she continued receiving an oral antibiotic therapy (amoxicillin/clavulanic acid in combination with levofloxacin) for another 4 weeks. At her follow-up examination (1 month postoperative) she did not have any focal neurological deficits and she was able to resume her daily activities. The postoperative brain MRI demonstrated only the usual postoperative changes of the brain without any sign of fluid collection or gadolinium enhancement [
Despite this incident, leflunomide was resumed after the termination of the antibiotic therapy, since her RA was refractory to the other antirheumatic therapies.
METHODS
The authors performed a review of the literature considering BA and other severe infections under treatment with leflunomide, published in PubMed, reported up to October 2020. Searching key words included “BA,” “RA,” “infections,” and “leflunomide.” A severe infection was defined as an infection requiring intravenous antibiotic therapy and hospitalization.
RESULTS
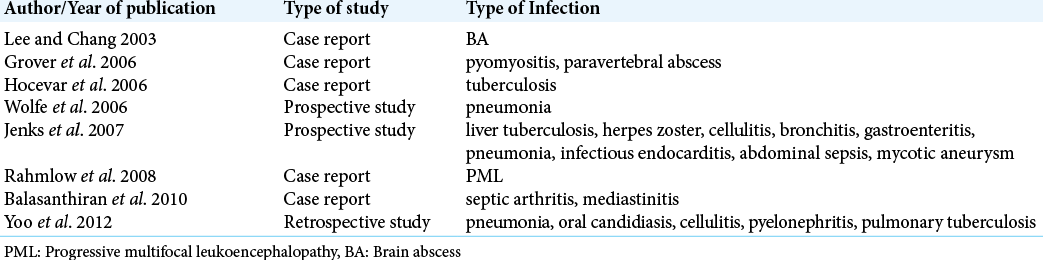
The results of the search showed a total of five case reports/ series, two prospective studies, and one retrospective study in RA patients under treatment with leflunomide. Apart from our case, only one other case of a BA has been reported (Lee and Chang, 2003),[
DISCUSSION
Our case illustrates that the differential diagnostic considerations in immunocompromised patients with neurologic deficits should include a focal CNS infection such as a BA, even in the absence of fever, and signs of a systemic infection or immunosuppressant-induced leucopenia.
MRI is an indispensable tool in the differential diagnosis of a BA. MRI demonstrates a well-defined T1-weighted images (T1WI) hypointense and T2-weighted images (T2W1) hyperintense lesion with a rim, best seen on T2WI, enhancing intensely on postcontrast T1WI (ring enhancement),[
Diagnostic delay may be caused by the non-specificity of the initial symptoms, such as dizziness and headache, and the absence of fever. Absence of fever can be seen in 30-76% of the cases,[
Leflunomide is a pyridine synthesis inhibitor used in the treatment of active RA. Its active metabolite reversely inhibits dihydroorotate dehydrogenase, resulting in the depletion of the pyrimidine supply to support the DNA synthesis and, subsequently, the proliferation of T-lymphocytes. It has also been implicated in the disruption of interleukin-1 and TNF-α pathways as well as in the glycosylation of adhesion molecules, thus reducing cell-cell contact activation during the inflammatory process.[
RA is characterized by dysfunctional innate immunity, which increases the risk for infections and infection-related mortality.[
On review of this literature, a direct cause-and-effect relationship between leflunomide and severe infections cannot be verified. Disease activity and duration, age, other comorbidities, and combination therapy with corticosteroids and/or other immunosuppressants also play a significant role. Jenks et al. imply that infections under leflunomide have the tendency to progress rapidly, therefore a washout with cholestyramine or activated carbon should be considered.[
The successful management of this rare case was not only the result of early identification but also of the cooperation and coordinated exchange of information and expertise of the different medical specialties in a tertiary hospital, including a neurologist, a neuroradiologist, a rheumatologist, an infectiologist, and a neurosurgeon.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Balasanthiran A, Vakilgilani T, Darzy K, Axon J. A case of severe staphylococcal septicaemia: Septic arthritis and a mediastinal abscess following leflunamide therapy for rheumatoid arthritis. BMJ Case Rep. 2010. 2010: bcr0720092082
2. Breedveld FC, Dayer JM. Leflunomide: Mode of action in the treatment of rheumatoid arthritis. Ann Rheum Dis. 2000. 59: 841-9
3. Brouwer MC, Coutinho JM, van de Beek D. Clinical characteristics and outcome of brain abscess: Systematic review and meta-analysis. Neurology. 2014. 82: 806-13
4. Carpenter J, Stapleton S, Holliman R. Retrospective analysis of 49 cases of brain abscess and review of the literature. Eur J Clin Microbiol Infect Dis. 2007. 26: 1-11
5. Chuang JM, Lin WC, Fang FM, Huang YJ, Ho JT, Lu CH. Bacterial brain abscess formation in post-irradiated patients: What is the possible pathogenesis?. Clin Neurol Neurosurg. 2015. 136: 132-8
6. Dorsett M, Liang SY. Diagnosis and treatment of central nervous system infections in the emergency department. Emerg Med Clin North Am. 2016. 34: 917-42
7. Grover R, Dhir V, Aneja R, Arya V, Galle A, Marwaha V. Severe infections following leflunomide therapy for rheumatoid arthritis. Rheumatology (Oxford). 2006. 45: 918-20
8. Hocevar A, Rozman B, Prapotnik S, Lestan D, Eržen V, Petric M. Leflunomide-associated tuberculosis?. Rheumatology (Oxford). 2006. 45: 228-9
9. Jameson JL, Kasper DL, Fauci AS.editors. Harrison’s Principles of Internal Medicine. New York: McGraw-Hill Education; 2018. p.
10. Jenks KA, Stamp LK, O’Donnell JL, Savage RL, Chapman P. Leflunomide-associated infections in rheumatoid arthritis. J Rheumatol. 2007. 34: 2201-3
11. Landriel F, Ajler P, Hem S, Bendersky D, Goldschmidt E, Garategui L. Supratentorial and infratentorial brain abscesses: Surgical treatment, complications and outcomes--a 10-year single-center study. Acta Neurochir (Wien). 2012. 154: 903-11
12. Lee CS, Chang CK. Brain abscess in rheumatoid arthritis. Ann Rheum Dis. 2003. 62: 689-90
13. Lee TH, Chang WN, Su TM, Chang HW, Lui CC, Ho JT. Clinical features and predictive factors of intraventricular rupture in patients who have bacterial brain abscesses. J Neurol Neurosurg Psychiatry. 2007. 78: 303-9
14. Leuthardt EC, Wippold FJ, Oswood MC, Rich KM. Diffusion-Weighted MR imaging in the preoperative assessment of brain abscesses. Surg Neurol. 2002. 58: 395-402
15. Michaud K, Wolfe F. Comorbidities in rheumatoid arthritis. Best Pract Res Clin Rheumatol. 2007. 21: 885-906
16. Miranda HA, Castellar-Leones SM, Elzain MA. Brain abscess: Current management. J Neurosci Rural Pract. 2013. 4: S67-81
17. Naz SM, Symmons DP. Mortality in established rheumatoid arthritis. Best Pract Res Clin Rheumatol. 2007. 21: 871-83
18. Rahmlow M, Shuster E, Dominik J, Deen HG, Dickson DW, Aksamit AJ. Leflunomide-associated progressive multifocal leukoencephalopathy. Arch Neurol. 2008. 65: 1538-9
19. Toh CH, Wei KC, Chang CN, Hsu PW, Wong HF, Ng SH. Differentiation of pyogenic brain abscesses from necrotic glioblastomas with use of susceptibility-weighted imaging. AJNR Am J Neuroradiol. 2012. 33: 1534-8
20. Wolfe F, Caplan L, Michaud K. Treatment for rheumatoid arthritis and the risk of hospitalization for pneumonia: Associations with prednisone, disease-modifying antirheumatic drugs, and anti-tumor necrosis factor therapy. Arthritis Rheum. 2006. 54: 628-34