- Department of Neurosurgery, Zagazig University, Zagazig,
- Department of Neurosurgery, Al Mokatam Insurance Hospital, Cairo, Egypt.
Correspondence Address:
Mahmoud M. Taha
Department of Neurosurgery, Zagazig University, Zagazig,
DOI:10.25259/SNI_543_2019
Copyright: © 2019 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Mahmoud M. Taha, Ahmad M. Elsharkawy, Hassan A. Al Menshawy, Amr AlBakry. Spontaneous cervical epidural hematoma: A case report and review of literature. 13-Dec-2019;10:247
How to cite this URL: Mahmoud M. Taha, Ahmad M. Elsharkawy, Hassan A. Al Menshawy, Amr AlBakry. Spontaneous cervical epidural hematoma: A case report and review of literature. 13-Dec-2019;10:247. Available from: https://surgicalneurologyint.com/surgicalint-articles/9800/
Abstract
Background: Spontaneous cervical epidural hematoma (SCEH) is an uncommon cause of acute spinal cord compression. This is a rare idiopathic condition that leads to acute onset of neurologic deficits, which if not diagnosed early can lead to catastrophic consequences.
Case Description: Here, we report a 41-year-old male, diagnosed with SCEH, with a presenting chief complaint of cervical pain followed by progressive quadriparesis and urgency of micturition who was managed surgically, along with the review of literature.
Conclusion: SCEH is a rare pathologic entity. Due to the high risk of poor neurological outcome without treatment, SCEH should be a diagnostic possibility when the presentation is even slightly suggestive. Prompt surgical evacuation of the hematoma and hemostasis leads to a favorable neurological outcome, whereas delay in treatment can be disastrous.
Keywords: Hemilaminectomy, Neurologic manifestations, Progressive, Spinal cord, Spontaneous cervical epidural hematoma
INTRODUCTION
Spinal epidural hematoma (SEH) is a very rare cause of acute spinal cord compression and is estimated to occur in approximately 0.1% of 100,000 individuals.[
CASE REPORT
This 41-year-old male presented with a 6-day history of acute neck pain radiating into both upper extremities, accompanied by unsteady gait, progressive quadriparesis, and urinary urgency. Notably, the patient had a cardiac valve replaced 2 years ago and was on routine anticoagulation. On admission, he was quadriparetic with Grade 2/5 motor function in the right upper and both lower extremities and 3/5 left upper extremity strength. He also had a relative pin level from C5 downward. Laboratory studies showed an initial INR of 3.5, with a platelet count of 90.000/mm3 and hemoglobin of 12 mg/dl. The urgent cervical MRI, done within 2 h of admission, showed a right dorsolateral intraspinal mass lesion extending from C5 to T1; the lesion was hyperintense on T1WI (weighted image) and showed heterogeneous isointensity-hypointensity on the T2WI. These findings were consistent with a spontaneous, early, and subacute cervical epidural hematoma [
Surgery
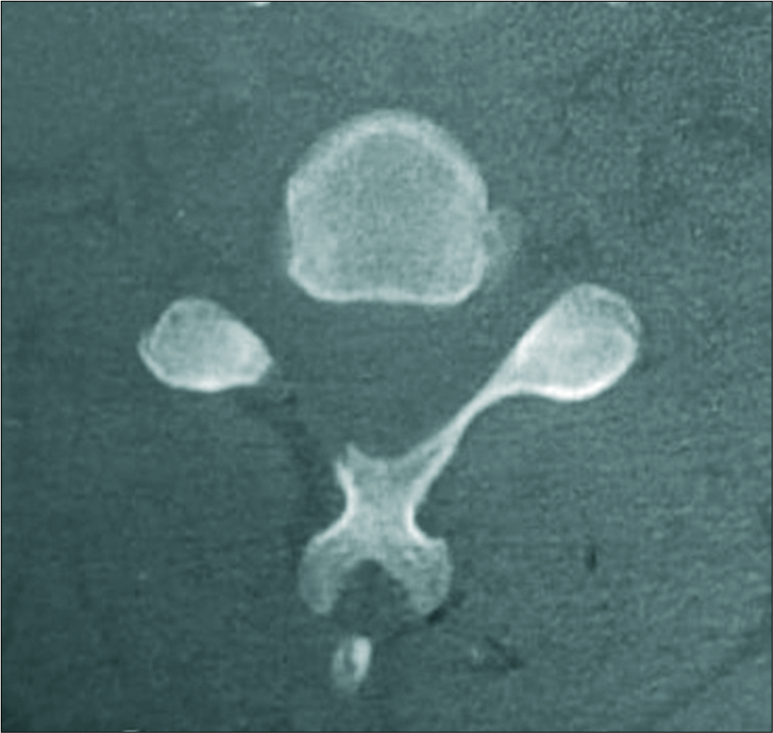
Evacuation of the hematoma was planned, and the patient preparation was started, 6 units of fresh frozen plasma, 36 units of platelets, 12 preoperative, 12 intraoperative, 12 postoperative, and 2 units of fresh blood were administered to the patient. Within 8 h after the initial MRI, utilizing C-arm guidance, a C5-T1 right hemilaminectomy was preformed allowing for complete hematoma evacuation [
DISCUSSION
SCEH is typically attributed to coagulopathies, anticoagulation, disc herniation, vascular malformations, neoplasms, and idiopathic causes.[
MRI of SEH
MRI is the diagnostic study of choice for SCEH.[
Neurological presentation
Although few cases of SCEH present with mild neurological symptoms, many exhibit frank quadriparesis/quadriplegia that should be rapidly diagnosed and treated to avoid permanent residual neurological deficits.[
CONCLUSION
SCEH is a rare disorder. Early diagnosis with MRI and hematoma evacuation within 24 h of symptom onset is critical to maximize recovery.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Anderson TJ, Donaldson IM. Spontaneous resolution of cervical spinal epidural haematoma. Postgrad Med J. 1989. 65: 488-90
2. Baek BS, Hur JW, Kwon KY, Lee HK. Spontaneous spinal epidural hematoma. J Korean Neurosurg Soc. 2008. 44: 40-2
3. Beatty RM, Winston KR. Spontaneous cervical epidural hematoma. A consideration of etiology. J Neurosurg. 1984. 61: 143-8
4. Bruyn GW, Bosma NJ, Vinken PJ, Bruyn GW. Spinal extradural haematoma. Handbook of Clinical Neurology. Amsterdam: Holland Publishing Company; 1976. 26: 1-30
5. Cai HX, Liu C, Zhang JF, Wan SL, Uchida K, Fan SW. Spontaneous epidural hematoma of thoracic spine presenting as Brown-Séquard syndrome: Report of a case with review of the literature. J Spinal Cord Med. 2011. 34: 432-6
6. Choi JH, Kim JS, Lee SH. Cervical spinal epidural hematoma following cervical posterior laminoforaminotomy. J Korean Neurosurg Soc. 2013. 53: 125-8
7. Fujiwara H, Oki K, Momoshima S, Kuribayashi S. PROPELLER diffusion-weighted magnetic resonance imaging of acute spinal epidural hematoma. Acta Radiol. 2005. 46: 539-42
8. Groen R. Non-operative treatment of spontaneous spinal epidural haematomas: A review of the literature and a comparison with operative cases. Acta Neurochir (Wien). 2004. 146: 103-10
9. Groen RJ, Ponssen H. The spontaneous spinal epidural haematoma: A study of the etiology. J Neurol Sci. 1990. 98: 121-38
10. Halim TA, Nigam V, Tandon V, Chhabra HS. Spontaneous cervical epidural hematoma: Report of a case managed conservatively. Indian J Orthop. 2008. 42: 357-9
11. Matsumura A, Namikawa T, Hashimoto R, Okamoto T, Yanagida I, Hoshi M. Clinical management for spontaneous epidural hematoma: Diagnosis and treatment. Spine J. 2007. 8: 534-7
12. Pope JV, Edlow JA. Avoiding misdiagnosis in patients with neurological emergencies. Emerg Med Int. 2012. 2012: 949275-
13. Song KJ, Lee KB. The poor outcome of the delayed diagnosis of acute spontaneous spinal epidural hematoma: Two cases report. J Korean Med Sci. 2005. 20: 331-4
14. Vayá A, Resurección M, Ricart JM, Ortuño C, Ripoll F, Mira Y. Spontaneous cervical epidural hematoma associated with oral anticoagulant therapy. Clin Appl Thromb Hemost. 2001. 7: 166-8
15. Vázquez-Barquero A, Abascal F, García-Valtuille R, Pinto JI, Figols FJ, Cerezal L. Chronic nontraumatic spinal epidural hematoma of the lumbar spine: MRI diagnosis. Eur Radiol. 2000. 10: 1602-5