- Department of Neurosurgery, All India Institute of Medical Sciences, New Delhi, Delhi, India.
DOI:10.25259/SNI_489_2019
Copyright: © 2020 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Amandeep Kumar, Poodipedi Chandra, Shashank Kale. Parietal transventricular approach for medial temporal glioma: A technical report. 14-Feb-2020;11:22
How to cite this URL: Amandeep Kumar, Poodipedi Chandra, Shashank Kale. Parietal transventricular approach for medial temporal glioma: A technical report. 14-Feb-2020;11:22. Available from: https://surgicalneurologyint.com/surgicalint-articles/9871/
Abstract
Background: Medial temporal lobectomy (MTLy) poses a surgical challenge due to convoluted anatomy of medial temporal lobe (MTL). Various approaches have been described to access MTL for removing various pathologies. We, hereby, describe the parietal transventricular approach for removing a concurrent medial temporal glioma in a patient with recurrent parietal glioma.
Case Description: A 40-year-old female operated and diagnosed case of the right parietal anaplastic astrocytoma presented to us with a recurrence in parietal region. In addition, a fresh lesion was observed in the right MTL suggestive of a separate temporal glioma. The patient underwent excision of both parietal and temporal gliomas through the parietal approach only. Complete excision of parietal recurrence and near-total excision of medial temporal glioma was achieved.
Conclusion: The parietal approach can be used for excision of medial temporal lesions, especially those involving or extending into its posterior limits. In the presence of concurrent parietal and MTL lesions, both lesions can be removed through a single parietal approach rather than a separate approach for MTLy. It offers additional advantages of the preservation of optic radiations as well as the temporal neocortex. The visual orientation of MTL structures is different when viewed from the parietal approach as compared to the temporal approaches. The parietal approach provides in line orientation of medial temporal structures contrary to the perpendicular orientation visualized in temporal approaches. An understanding of MTL anatomy as viewed from a parietal vantage point and its three-dimensional conceptualization is very important to successfully remove lesions of MTL through the parietal approach.
Keywords: Glioma, Medial temporal lobectomy, Parietal transventricular approach
INTRODUCTION
Medial temporal lobectomy (MTLy) is performed for various indications, most commonly for temporal lobe epilepsy and tumors of medial temporal lobe (MTL). MTLy has posed challenges to neurosurgeons as MTL is a complex convoluted structure. Several approaches have been described for accessing and removing lesions of MTL.[
CASE REPORT
A 40-year-old female operated and diagnosed case of the right parietal anaplastic astrocytoma presented to us with recurrence of symptoms after being lost to follow-up after the first surgery performed 1 year back. The latest magnetic resonance imaging (MRI) revealed a recurrence in the parietal region that was reaching up to the ventricular surface. Apart from the parietal lesion, a fresh signal change could be observed in the right MTL suggestive of a separate temporal glioma [
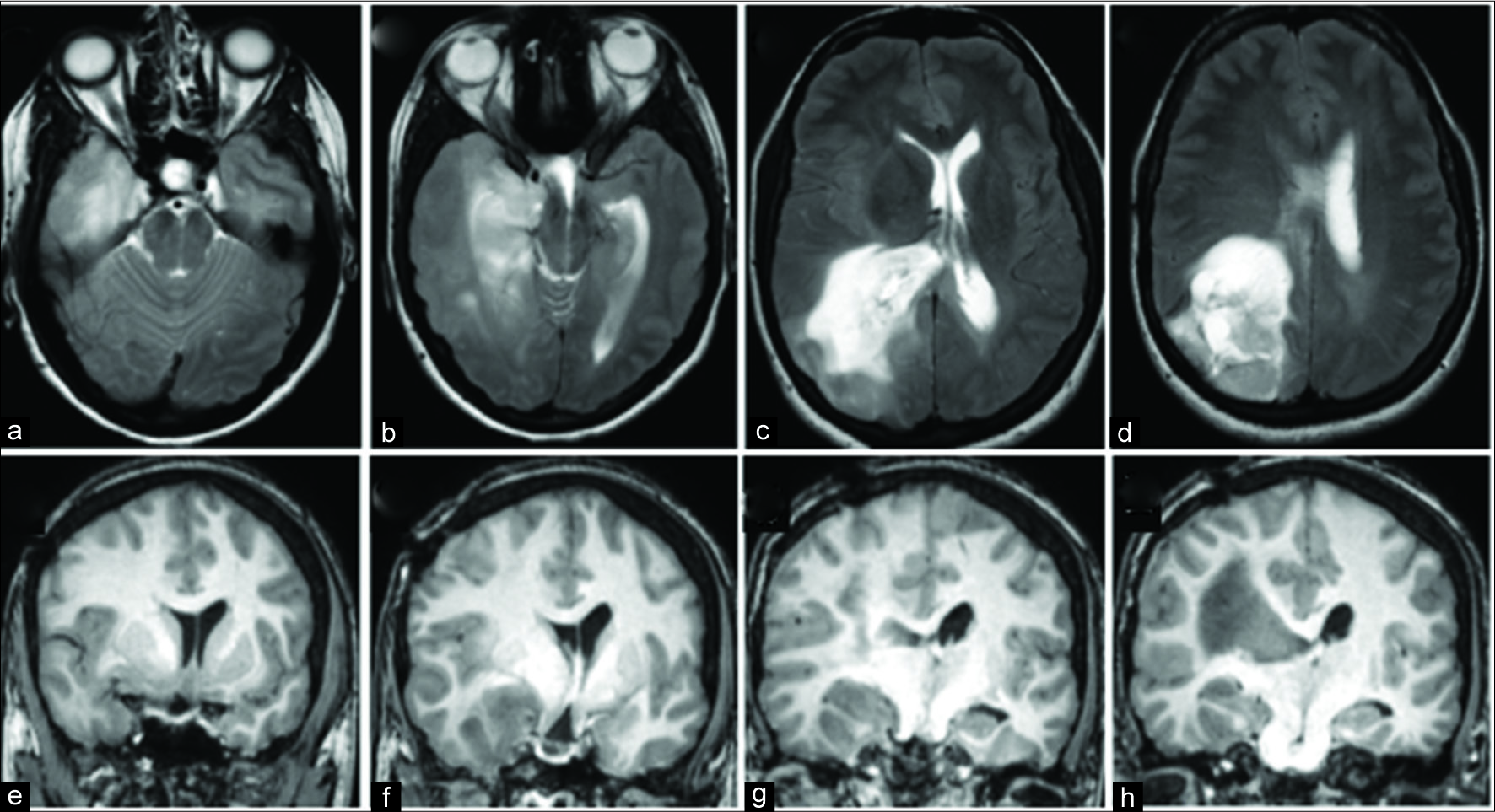
Figure 1:
Preoperative magnetic resonance imaging images. Axial (a-d) and coronal (e-h) images show a lesion hyperintense on T2-weighted (T2W) images and isointense on T1-weighted (T1W) images, involving the right medial temporal lobe (a, b, and e-h) and large recurrent tumor involving the right parietal region (c and d).
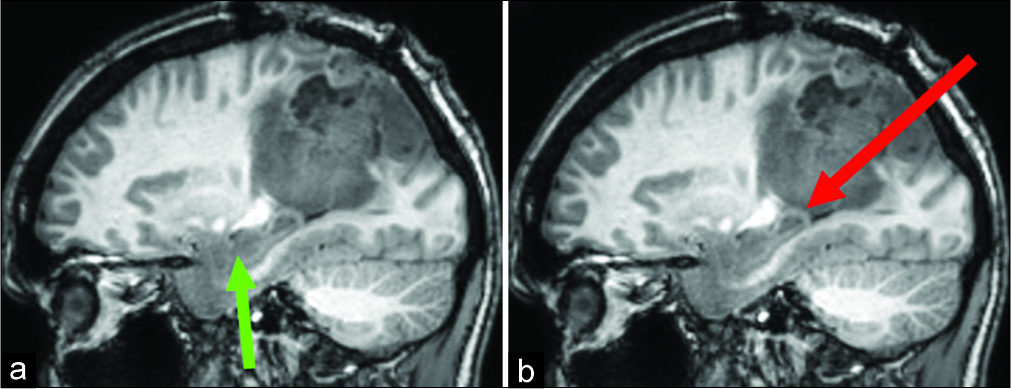
The patient was positioned prone with head turned slightly toward the right side. Through the scalp incision, the previous parietal craniotomy flap was raised. The parietal tumor was completely resected. At the end of the resection of parietal tumor, the ventricular cavity was entered as the tumor was extending till and bulging into ventricles. The retraction was applied using the Leyla retractor system so as to get a view of the atrium and the temporal horn. The normal anatomical landmarks, including thalamus, choroid plexus, fimbriae, and body of fornix, were identified. There was no continuity between the parietal and medial temporal tumors confirming the two being concurrent tumors. The enlarged hippocampus was seen along its entire length, except the region of amygdala, that was not in the line of vision. The orientation of hippocampus/parahippocampus was along its anteroposterior axis [
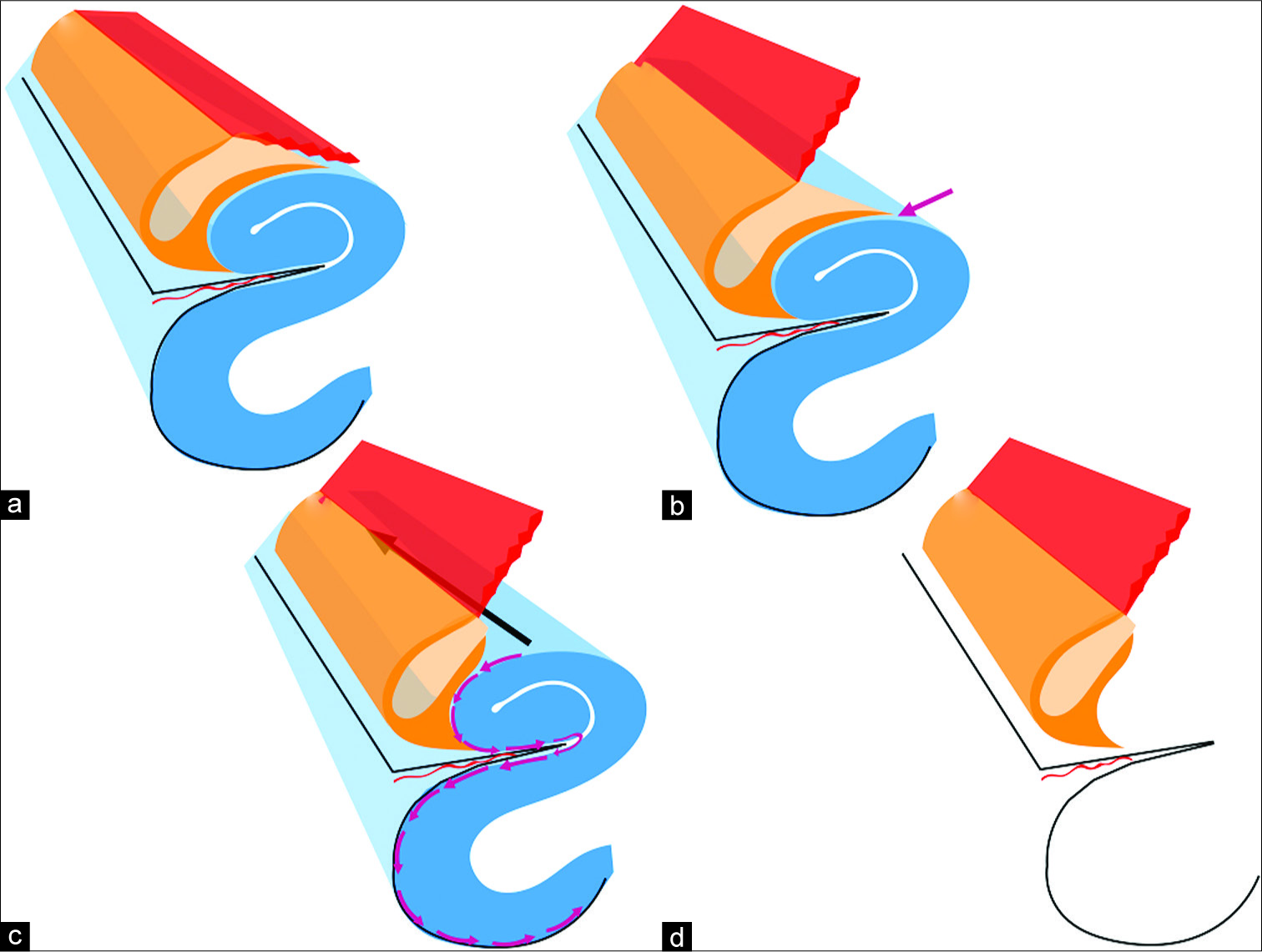
Figure 3:
Diagrammatic illustration of the right medial temporal anatomy and the procedure of medial temporal lobectomy (MTLy) when performed through parietal transventricular approach. The hippocampus/parahippocampus (blue) is visualized in an anteroposterior orientation in this approach (a). The choroid plexus (red) is reflected medially followed by dissection (purple arrow) of fimbriae (yellow) away from hippocampus (b). The dissection then proceeds along with the surface of hippocampus and parahippocampus (serial purple arrows in c) to separate them from the hippocampal fissure pia/arachnoid. These steps are repeated and dissection proceeds in anterior direction (black arrow in c) to complete the MTLy (d).
DISCUSSION
MTLy has been considered a challenging procedure. The convoluted anatomy and long anteroposterior dimensions of medial temporal structures with associated two bends along with the midbrain and petrous pyramid are the factors responsible for the complexity associated with surgery of this region. For this reason, it is also difficult to approach the entire length of medial temporal structures with a single approach.[
Various approaches that are used for accessing the MTL include transsylvian, anterior two-third temporal lobe resection, subtemporal, and transcortical.[
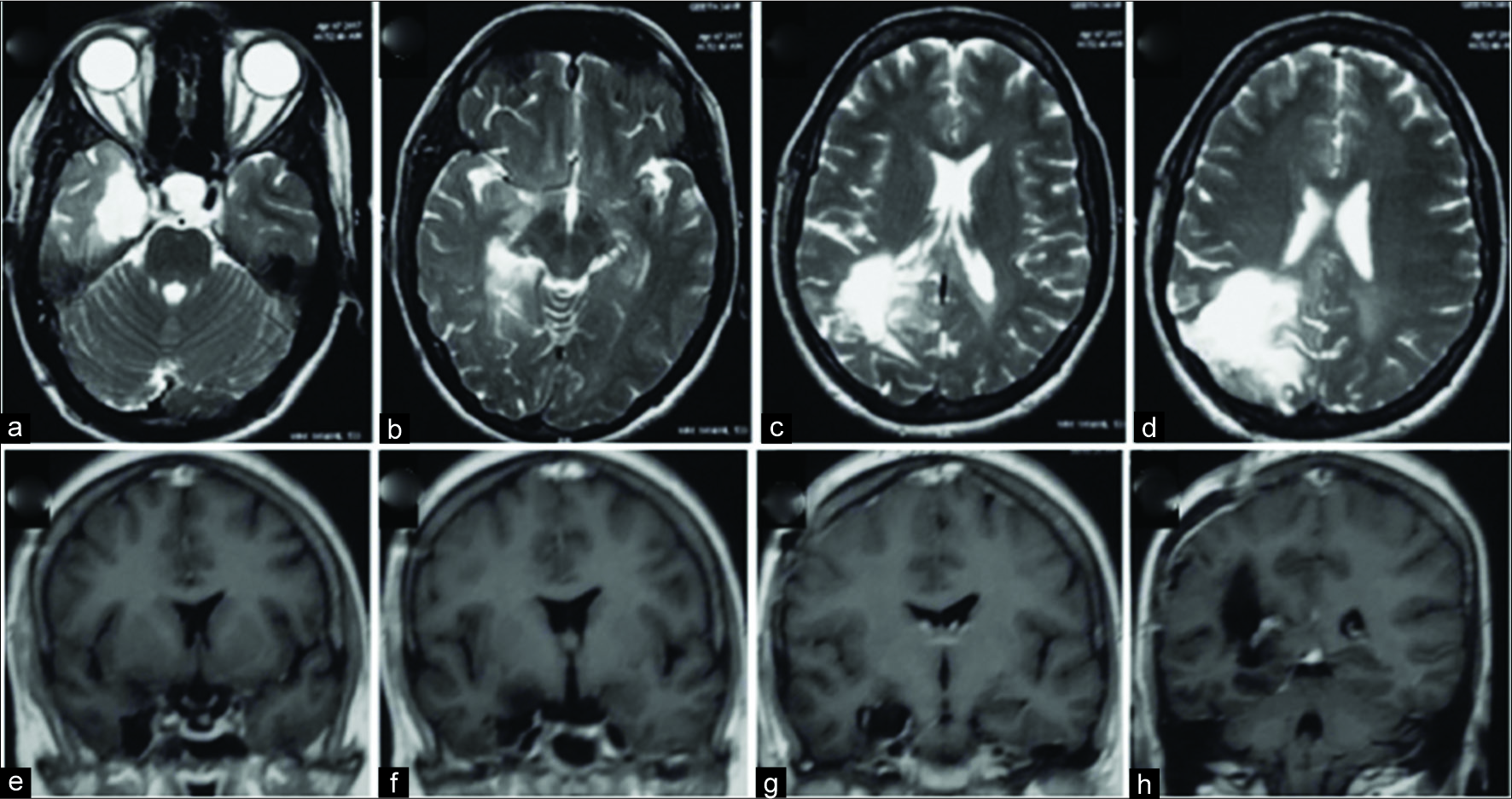
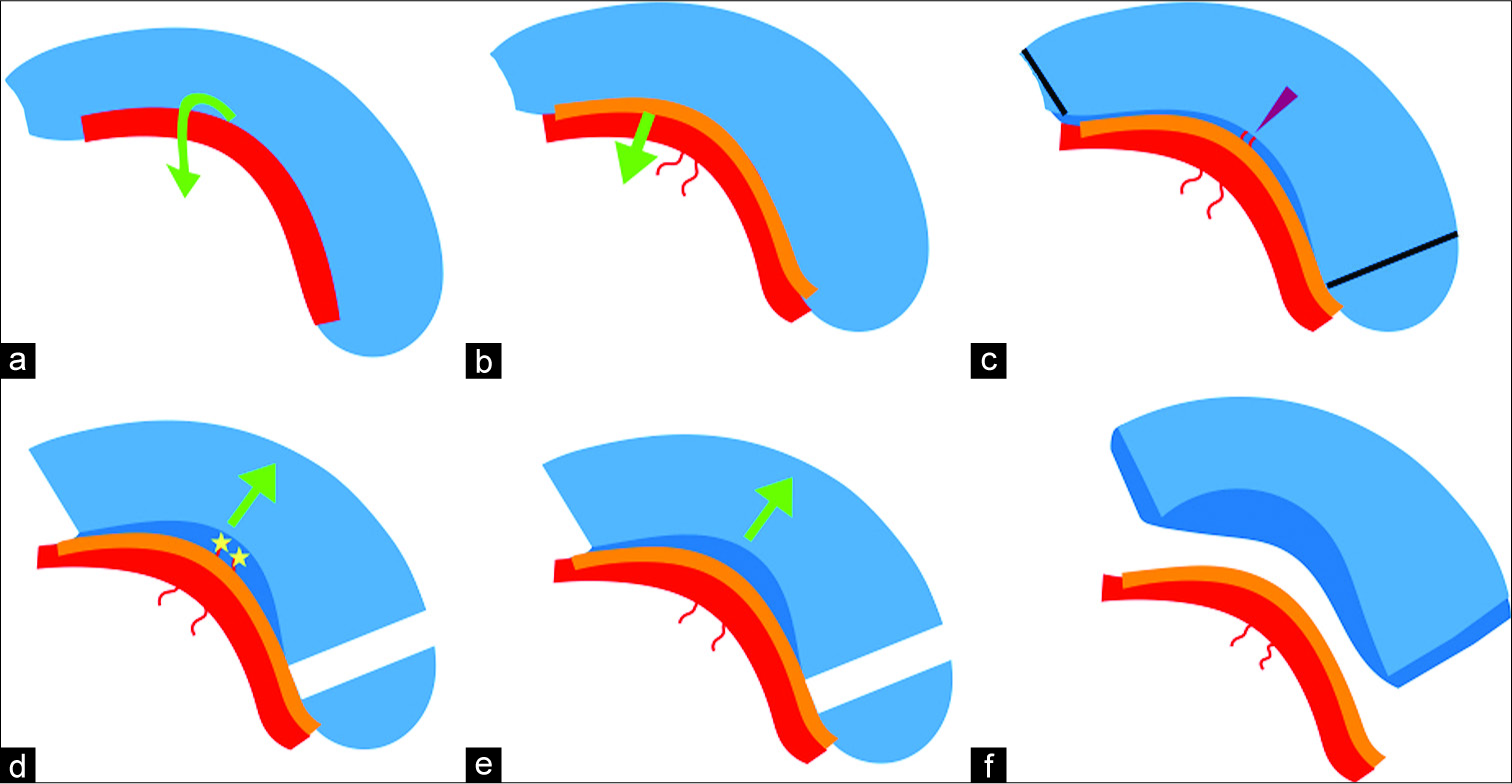
Figure 5:
Diagrammatic illustration of the right medial temporal anatomy and the procedure of medial temporal lobectomy (MTLy) through temporal approach. The hippocampus (blue) is visualized in a perpendicular orientation to visual trajectory (a). The choroid plexus (red) is reflected medially (curved green arrow in a). The dissection of fimbriae (orange in b) reveals the hippocampal fissure with hippocampal vessels (purple arrowhead in c). Anterior and posterior disconnections (black lines in c) are then made. After dissection of hippocampus/parahippocampus from hippocampal fissure and surrounding pia/arachnoid, the MTLy specimen is then removed (d-f). Yellow oval represents amygdala.
In this report, the author describes MTLy performed through a PTV route. This approach was chosen in this particular case because the atrium of the lateral ventricle was made accessible by the parietal tumor extending from the cerebral to the ventricular surface. The patient had no visual field deficits preoperatively, suggesting the displacement of optic radiation fibers. There was thus a possibility of preserving the optic radiations if the tumor was approached through the parietal route as compared to the standard anterior temporal approaches that are associated with a significant risk of injury to optic radiation with consequent field cuts.[
CONCLUSION
PTVa can be used for excision of medial temporal lesions, especially those involving or extending into its posterior limits. In the presence of concurrent parietal and MTL lesions, both lesions can be removed through a single parietal approach rather than a separate approach for MTLy. It offers additional advantages of the preservation of optic radiations as well as temporal neocortex. The visual orientation of MTL structures is different when viewed from PTVa as compared to the temporal approaches. The PTVa provides in line orientation of medial temporal structures contrary to the perpendicular orientation visualized in temporal approaches. An understanding of MTL anatomy as viewed from a parietal vantage point and its three- dimensional conceptualization is very important to successfully remove lesions of MTL through the parietal approach.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms.
Financial support and sponsorship
Publication of this article was made possible by the James I. and Carolyn R. Ausman Educational Foundation.
Conflicts of interest
There are no conflicts of interest.
References
1. Erdem A, Yaşargil G, Roth P. Microsurgical anatomy of the hippocampal arteries. J Neurosurg. 1993. 79: 256-65
2. Fried I, Kim JH, Spencer DD. Limbic and neocortical gliomas associated with intractable seizures: A distinct clinicopathological group. Neurosurgery. 1994. 34: 815-23
3. Horel JA, Misantone LJ. Visual discrimination impaired by cutting temporal lobe connections. Science. 1976. 193: 336-8
4. Hori T, Yamane F, Ochiai T, Kondo S, Shimizu S, Ishii K. Selective subtemporal amygdalohippocampectomy for refractory temporal lobe epilepsy: Operative and neuropsychological outcomes. J Neurosurg. 2007. 106: 134-41
5. Miyamoto S, Kataoka H, Ikeda A, Takahashi J, Usui K, Takayama M. A combined subtemporal and transventricular/transchoroidal fissure approach to medial temporal lesions. Neurosurgery. 2004. 54: 1162-7
6. Olivier A. Transcortical selective amygdalohippocampectomy in temporal lobe epilepsy. Can J Neurol Sci. 2000. 27: S68-76
7. Schramm J, Aliashkevich AF. Temporal mediobasal tumors: A proposal for classification according to surgical anatomy. Acta Neurochir (Wien). 2008. 150: 857-64
8. Smith KA, Spetzler RF. Supratentorial-infraoccipital approach for posteromedial temporal lobe lesions. J Neurosurg. 1995. 82: 940-4
9. Türe U, Harput MV, Kaya AH, Baimedi P, Firat Z, Türe H. The paramedian supracerebellar-transtentorial approach to the entire length of the mediobasal temporal region: An anatomical and clinical study. Laboratory investigation. J Neurosurg. 2012. 116: 773-91
10. Uribe JS, Vale FL. Limited access inferior temporal gyrus approach to mesial basal temporal lobe tumors. J Neurosurg. 2009. 110: 137-46
11. Vajkoczy P, Krakow K, Stodieck S, Pohlmann-Eden B, Schmiedek P. Modified approach for the selective treatment of temporal lobe epilepsy: Transsylvian-transcisternal mesial en bloc resection. J Neurosurg. 1998. 88: 855-62
12. Weiner HL, Kelly PJ. A novel computer-assisted volumetric stereotactic approach for resecting tumors of the posterior parahippocampal gyrus. J Neurosurg. 1996. 85: 272-7
13. Wen HT, Rhoton AL, de Oliveira E, Cardoso AC, Tedeschi H, Baccanelli M. Microsurgical anatomy of the temporal lobe: Part 1: Mesial temporal lobe anatomy and its vascular relationships as applied to amygdalohippocampectomy. Neurosurgery. 1999. 45: 549-91
14. Wheatley BM. Selective amygdalohippocampectomy: The trans-middle temporal gyrus approach. Neurosurg Focus. 2008. 25: E4-
15. Wieser HG, Yaşargil MG. Selective amygdalohippocampectomy as a surgical treatment of mesiobasal limbic epilepsy. Surg Neurol. 1982. 17: 445-57
16. Yasargil MG, Reeves JD. Tumours of the limbic and paralimbic system. Acta Neurochir (Wien). 1992. 116: 147-9
17. Yaşargil MG, Teddy PJ, Roth P. Selective amygdalo-hippocampectomy. Operative anatomy and surgical technique. Adv Tech Stand Neurosurg. 1985. 12: 93-123
18. Yasargil MG.editorsLimbic and 0Paralimbic Tumors, in Microneur- osurgery IV B. New York: Thieme Medical Publishers; 1996. p. 252-90
19. Yonekawa Y, Imhof HG, Taub E, Curcic M, Kaku Y, Roth P. Supracerebellar transtentorial approach to posterior temporomedial structures. J Neurosurg. 2001. 94: 339-45