- Department of Neurosurgery, University of California Los Angeles, Los Angeles, United States.
- Department of Neurosurgery, Providence Saint John’s Health Center, Santa Monica, California, United States.
- Department of Neurosurgery, Brown University, Providence, Rhode Island, United States.
- Department of Neurosurgery, Children’s Hospital of Philadelphia, Philadelphia, Pennsylvania, United States.
- Department of Anesthesiology, University of California Los Angeles, Los Angeles, California, United States.
- Department of Cardiology, University of California Los Angeles, Los Angeles, California, United States.
Correspondence Address:
Luke Macyszyn , Department of Neurosurgery, University of California Los Angeles, Los Angeles, California, United States.
DOI:10.25259/SNI_337_2021
Copyright: © 2021 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Sophie M. Peeters1, Daniel Nagasawa2, Bilwaj Gaonkar1, Tianyi Niu3, Alexander Tucker4, Mark Attiah1, Diana Babayan1, Natalie Moreland5, Isaac Yang1, Marcela Calfon Press6, Luke Macyszyn1. Perioperative dual antiplatelet therapy for patients undergoing spine surgery soon after drug eluting stent placement. 28-Jun-2021;12:302
How to cite this URL: Sophie M. Peeters1, Daniel Nagasawa2, Bilwaj Gaonkar1, Tianyi Niu3, Alexander Tucker4, Mark Attiah1, Diana Babayan1, Natalie Moreland5, Isaac Yang1, Marcela Calfon Press6, Luke Macyszyn1. Perioperative dual antiplatelet therapy for patients undergoing spine surgery soon after drug eluting stent placement. 28-Jun-2021;12:302. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=10934
Abstract
Background: Performing emergent spinal surgery within 6 months of percutaneous placement of drug-eluting coronary stent (DES) is complex. The risks of spinal bleeding in a “closed space” must be compared with the risks of stent thrombosis or major cardiac event from dual antiplatelet therapy (DAPT) interruption.
Methods: Eighty relevant English language papers published in PubMed were reviewed in detail.
Results: Variables considered regarding surgery in patients on DAPT for DES included: (1) surgical indications, (2) percutaneous cardiac intervention (PCI) type (balloon angioplasty vs. stenting), (3) stent type (drug-eluting vs. balloon mechanical stent), and (4) PCI to noncardiac surgery interval. The highest complication rate was observed within 6 weeks of stent placement, this corresponds to the endothelialization phase. Few studies document how to manage patients with critical spinal disease warranting operative intervention within 6 months of their PCI for DES placement.
Conclusion: The treatment of patients requiring urgent or emergent spinal surgery within 6 months of undergoing a PCI for DES placement is challenging. As early interruption of DAPT may have catastrophic consequences, we hereby proposed a novel protocol involving stopping clopidogrel 5 days before and aspirin 3 days before spinal surgery, and bridging the interval with a reversible P2Y12 inhibitor until surgery. Moreover, postoperatively, aspirin could be started on postoperative day 1 and clopidogrel on day 2. Nevertheless, this treatment strategy may not be appropriate for all patients, and multidisciplinary approval of perioperative antiplatelet therapy management protocols is essential.
Keywords: Cangrelor, Drug-eluting stent, Dual antiplatelet therapy, Emergent spine surgery, P2Y12 inhibitor
INTRODUCTION
At least 6–12 months of dual antiplatelet therapy (DAPT) are routinely utilized after placement of drug-eluting coronary stents (DES).[
Here, we reviewed the literature regarding the feasibility and safety of performing urgent spinal surgery for patients on DAPT soon after DES placement utilizing a novel approach. The latter involves cessation of clopidogrel (5 days) and aspirin (3 days) preoperatively with postoperative reinstitution of aspirin (postoperative day 1) and clopidogrel (postoperative day 2).
MATERIALS AND METHODS
Important variables when considering surgery in a patient on DAPT for recent cardiac stent placement: (1) the urgency of the surgery, (2) the type of percutaneous cardiac intervention (PCI) (balloon angioplasty vs. stenting), (3) the stent type (drug-eluting vs. balloon mechanical stent), and (4) the PCI to noncardiac surgery time interval.[
A thorough PubMed search yielded 510 papers on the topic. Critical variables studied included: outcomes of post-PCI patients undergoing emergent spine surgery while on DAPT, perioperative anticoagulation guidelines, and alternative drugs that lessen the risk of bleeding without increasing the risk of stent thrombosis.
RESULTS
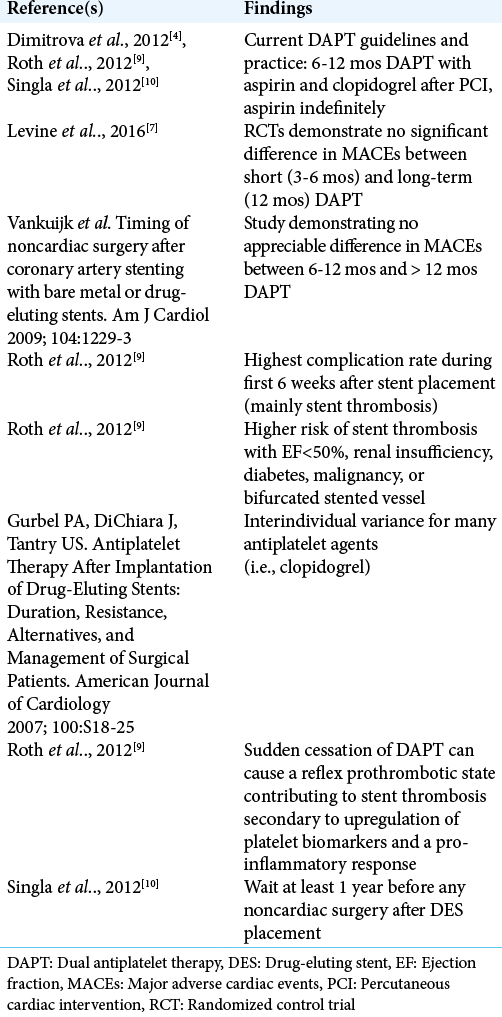
Guidelines for DAPT and timing of noncardiac surgery after PCI [ Table 1 ]
The American College of Cardiology, American Heart Association, and European Society of Cardiology have relatively congruent guidelines regarding the necessity of DAPT for patients with acute coronary syndrome who have undergone PCI with the placement of DES.[
The guidelines currently recommend waiting at least 1 year before any noncardiac surgery after DES placement, to allow sufficient time for endothelialization.[
Urgent surgical treatment for cervical spondylotic myelopathy (CSM): indications and management
With rapidly progressing CSM, postponing surgery risks permanent severe disability. Treatment options for CSM include corpectomy and fusion, anterior cervical discectomy and fusion, posterior cervical decompression (with or without fusion), or any combination thereof.[
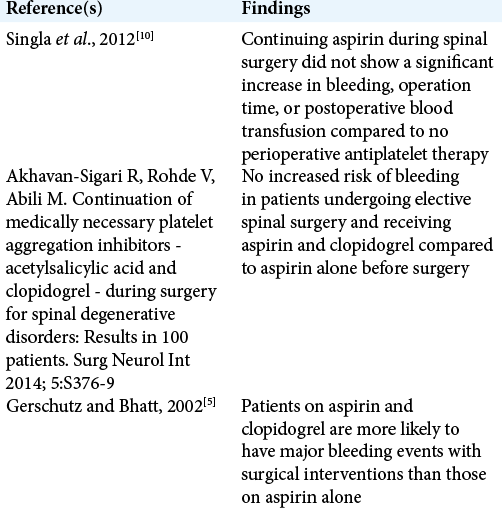
Perioperative management of DAPT for major noncardiac surgery soon after PCI [ Table 2 ]
The Clopidogrel in Unstable Angina to Prevent Recurrent Events study and others concluded that patients on both aspirin and clopidogrel are more likely to have major bleeding events and bleeding complications with surgical interventions (3.4-fold) than those solely on aspirin (1.5-fold) [
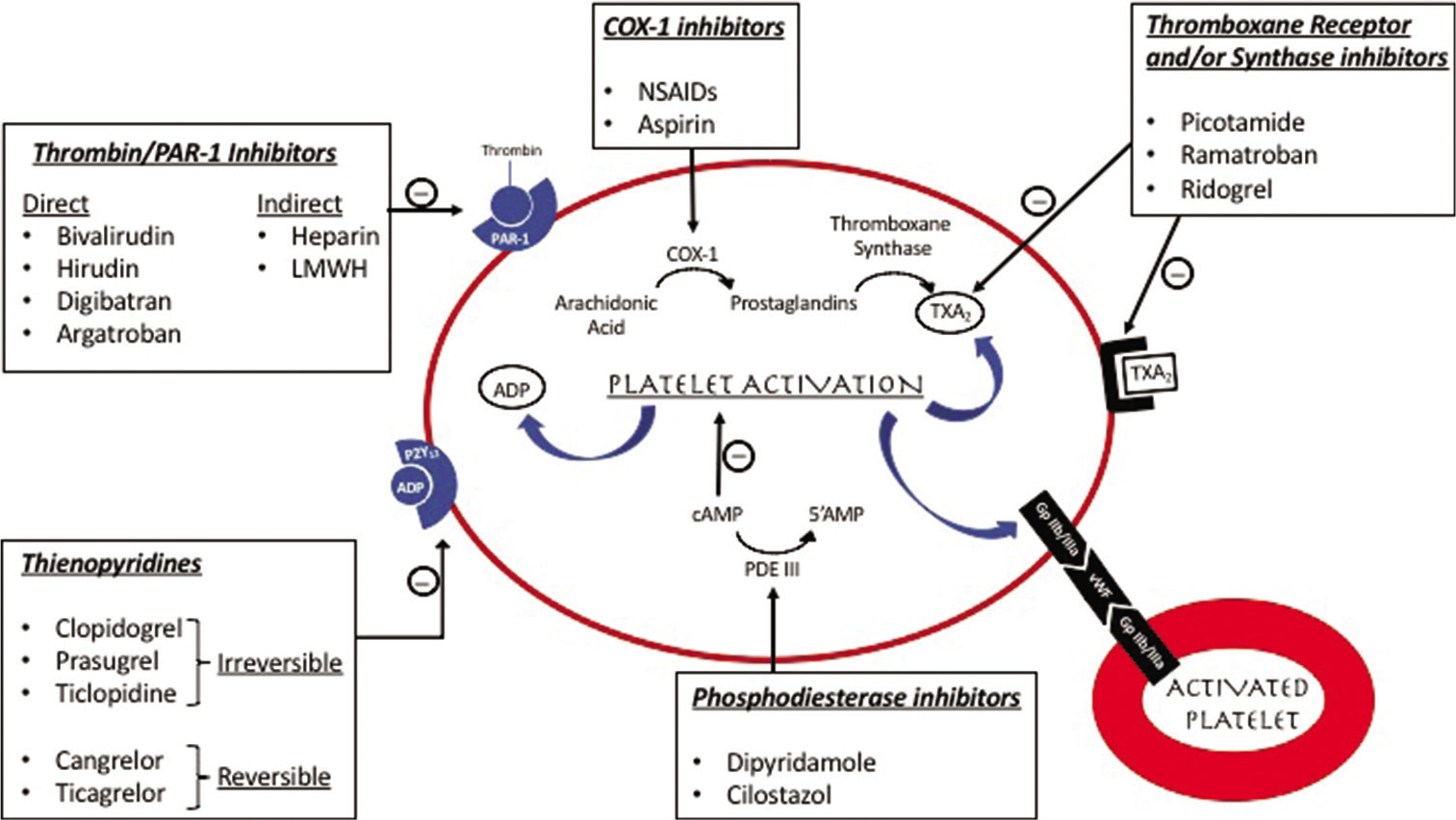
However, as the sudden cessation of DAPT can cause a reflex prothrombotic state possibly contributing to stent thrombosis, an antiplatelet “bridge” is recommended perioperatively.[
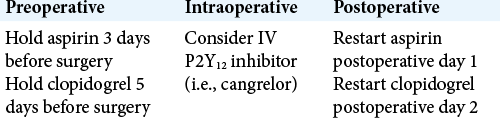
Bridging protocol recommendations [ Table 3 ]
No standard of care exists regarding perioperative management of patients with DES on DAPT undergoing spine surgery. Some recommend holding DAPT up to five half-lives before surgery and starting a bridging agent within 12 months of the PCI to minimize ischemic cardiac events.[
Bridging agents include GP IIb/IIIa receptor inhibitors which interfere with fibrinogen, oral irreversible P2Y12 receptor inhibitors, and thrombin protease-activated receptor inhibitors. Postoperatively, both aspirin and clopidogrel can be safely restarted on postoperative day 1 or 2 with loading doses [
Promise of cangrelor
Cangrelor, a reversible, intravenous P2Y12 inhibitor with rapid onset and return to baseline platelet function when discontinued may be considered as a new bridging agent [
CONCLUSION
There is a great concern regarding the lack of clear guidelines for perioperative antiplatelet therapy for patients requiring urgent or emergent spine surgery within 6 months of PCI with DES implantation. We propose a novel protocol in which clopidogrel and aspirin are stopped 5 and 3 days before surgery, respectively, a reversible P2Y12 inhibitor such as cangrelor is used as bridging agent until the time of surgery, and postoperatively, aspirin and clopidogrel may be restarted on postoperative day 1 and 2, respectively.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors. For this type of study, formal consent is not required.
Declaration of patient consent
Patient’s consent not required as there are no patients in this study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Bhatt DL, Stone GW, Mahaffey KW, Gibson CM, Steg PG, Hamm CW. Effect of platelet inhibition with cangrelor during PCI on ischemic events. N Engl J Med. 2013. 368: 1303-13
2. Broad L, Lee T, Conroy M, Bolsin S, Orford N, Black A. Successful management of patients with a drug-eluting coronary stent presenting for elective, non-cardiac surgery. Br J Anaesth. 2007. 98: 19-22
3. Capodanno D, Musumeci G, Lettieri C, Limbruno U, Senni M, Guagliumi G. Impact of bridging with perioperative low-molecular-weight heparin on cardiac and bleeding outcomes of stented patients undergoing non-cardiac surgery. Thromb Haemost. 2015. 114: 423-31
4. Dimitrova G, Tulman DB, Bergese SD. Perioperative management of antiplatelet therapy in patients with drug-eluting stents. HSR Proc Intensive Care Cardiovasc Anesth. 2012. 4: 153-67
5. Gerschutz GP, Bhatt DL. The CURE trial: Using clopidogrel in acute coronary syndromes without ST-segment elevation. Cleve Clin J Med. 2002. 69: 377-8, 380, 382
6. Kadaňka Z, Bednařík J, Voháňka S, Vlach O, Stejskal L, Chaloupka R. Conservative treatment versus surgery in spondylotic cervical myelopathy: A prospective randomised study. Eur Spine J. 2000. 9: 538-44
7. Levine GN, Bates ER, Bittl JA, Brindis RG, Fihn SD, Fleisher LA. 2016 ACC/AHA guideline focused update on duration of dual antiplatelet therapy in patients with coronary artery disease: A report of the American college of cardiology/American heart association task force on clinical practice guidelines. J Thorac Cardiovasc Surg. 2016. 152: 1243-75
8. Liu JM, Peng HW, Liu ZL, Long XH, Yu YQ, Huang SH. Hybrid decompression technique versus anterior cervical corpectomy and fusion for treating multilevel cervical spondylotic myelopathy: Which one is better?. World Neurosurg. 2015. 84: 2022-9
9. Roth E, Purnell C, Shabalov O, Moguillansky D, Hernandez CA, Elnicki M. Perioperative management of a patient with recently placed drug-eluting stents requiring urgent spinal surgery. J Gen Intern Med. 2012. 27: 1080-3
10. Singla S, Sachdeva R, Uretsky BF. The risk of adverse cardiac and bleeding events following noncardiac surgery relative to antiplatelet therapy in patients with prior percutaneous coronary intervention. J Ame Coll Cardiol. 2012. 60: 2005-16
11. Voeltz MD, Manoukian SV. Cangrelor in patients undergoing cardiac surgery: The BRIDGE study. Expert Rev Cardiovasc Ther. 2013. 11: 811-6
12. Waite LH, Phan YL, Spinler SA. Cangrelor: A novel intravenous antiplatelet agent with a questionable future. Pharmacotherapy. 2014. 34: 1061-76
13. Wang T, Wang H, Liu S, An HD, Liu H, Ding WY. Anterior cervical discectomy and fusion versus anterior cervical corpectomy and fusion in multilevel cervical spondylotic myelopathy: A meta-analysis. Medicine (Baltimore). 2016. 95: e5437