- Department of Neurosurgery, Avicenne Military Hospital of Marrakech and Mohammed V University in Rabat, Morocco,
- Departments of Radiology, Avicenne Military Hospital of Marrakech, Marrakech, Morocco
- Anesthesiology, Avicenne Military Hospital of Marrakech, Marrakech, Morocco.
Correspondence Address:
Ali Akhaddar, Department of Neurosurgery, Avicenne Military Hospital of Marrakech and Mohammed V University in Rabat, Morocco.
DOI:10.25259/SNI_197_2022
Copyright: © 2022 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Ali Akhaddar1, Salah Bellasri2, Ayoub Belhadj3, Hassan Baallal1. Remote bifrontal epidural hematoma following hemispheric glioma resection. A rare life-threatening postoperative complication. 15-Apr-2022;13:149
How to cite this URL: Ali Akhaddar1, Salah Bellasri2, Ayoub Belhadj3, Hassan Baallal1. Remote bifrontal epidural hematoma following hemispheric glioma resection. A rare life-threatening postoperative complication. 15-Apr-2022;13:149. Available from: https://surgicalneurologyint.com/surgicalint-articles/11534/
Abstract
Background: Postoperative acute epidural hematoma (EDH) is a well-known serious complication that usually occurs at the operated site after cranial surgery. However, epidural bleeding, distant from the site of the previous craniotomy, is relatively rare and may sometimes cause significant neurological morbidity or even mortality. We report such a case.
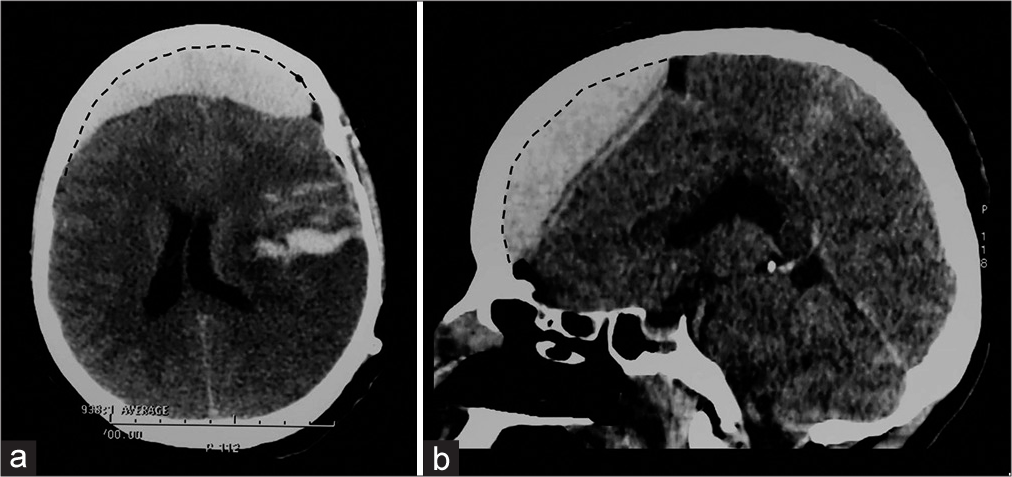
Case Description: A 35-year-old woman, previously healthy, was operated on for a left temporo-parieto-fronto-insular anaplastic astrocytoma. Between 2 and 4 h after the surgery, the patient had trouble waking-up following the general anesthesia. Emergent computed tomography (CT) scan revealed an acute bifrontal EDH away from the initial surgical field. The patient underwent an immediate reoperation, a decompressive bifrontal craniotomy, and the evacuation of the hematoma. Despite the neurologic improvement, she died 24 days after the surgery due to severe sepsis caused by pulmonary infection with pseudomonas aeruginosa.
Conclusion: The pathophysiology of postoperative remote EDH is poorly understood, although various hypotheses have been suggested including the loss of tamponade effect, the vasomotor mechanisms, and the coagulopathy. As seen in the present case report, we suspected that the intensive use of perioperative mannitol may also promote this complication. In the early postoperative period, every patient with neurological deterioration should have a rapid cranial CT-scan because early detection and removal of postoperative acute EDH can be life-saving.
Keywords: Brain tumors, Craniotomy, Epidural hematoma, Glioma, Postoperative complication, Remote
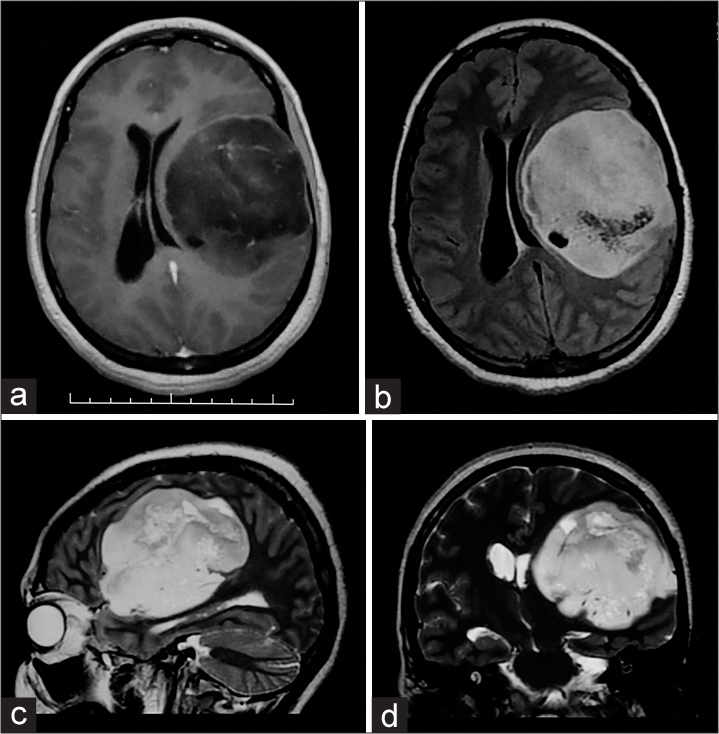
A 35-year-old woman, previously healthy, was referred to our department with a 12-month history of headache and a right hemiparesis that started 2 months before her admission. Magnetic resonance imaging of the patient’s head showed a left intraxial temporo-parietofronto-insular tumor (7.2 × 7.8 × 6.9 cm) with a 1.2 cm midline shift to the right [
Figure 1:
Voluminous tumor involving the left frontal, parietal, and temporal lobes in a 35-year-old woman. Brain magnetic resonance imaging: Axial post gadolinum T1-weighted image (a) and on FLAIR sequences (b). Sagittal (c) and coronal (d) T2-weighted images. Histopathological diagnosis was an anaplastic astrocytoma.
Postoperative acute EDH is a well-known serious complication that usually occurs at the site of the cranial surgery.[
The pathophysiology of this unusual condition is poorly understood although various hypotheses have been suggested including the loss of tamponade effect, the vasomotor mechanisms, and the coagulopathy.[
Depending on its location, the distant postsurgical EDH can be classified as in the adjacent site, on the contralateral side, or more rarely on bilateral side. Between 1974 and 2015, 23 cases of remote postoperative EDH after brain tumor surgery were reported in the literature.[
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflict of interest.
References
1. Akhaddar A, Ajja A, Boucetta M. Combined epidural and intracerebral hematomas after evacuation of bilateral chronic subdural hematoma. Neurochirurgie. 2008. 54: 728-30
2. Akhaddar A. Letter to the editor: Talking about our own complications: Is it still a taboo subject in neurosurgery?. World Neurosurg. 2020. 142: 579
3. Chung HJ, Park JS, Park JH, Jeun SS. Remote postoperative epidural hematoma after brain tumor surgery. Brain Tumor Res Treat. 2015. 3: 132-7
4. Dash C, Gurjar H, Garg K, Sharma BS, Singla R. Massive life-threatening bifrontal epidural hematoma following placement of an external ventricular drain. Childs Nerv Syst. 2016. 32: 237-9
5. Kim SH, Lee JH, Joo W, Chough CK, Park HK, Lee KJ. Analysis of the risk factors for development of post-operative extradural hematoma after intracranial surgery. Br J Neurosurg. 2015. 29: 243-8
6. Przepiórka Ł, Kunert P, Żyłkowski J, Fortuniak J, Larysz P, Szczepanek D. Necessity of dural tenting sutures in modern neurosurgery: Protocol for a systematic review. BMJ Open. 2019. 9: e027904
7. Tyagi G, Bhat DI, Devi BI, Shukla D. Multiple remote sequential supratentorial epidural hematomas-an unusual and rare complication after posterior fossa surgery. World Neurosurg. 2019. 128: 83-90
8. Yakar F, Dogan I, Bahadır B, Ozates MO, Ozgural O, Attar A. Epidural hematoma: Postoperative complication. Int Surg J. 2017. 4: 2058-62
9. Yu J, Yang H, Cui D, Li Y. Retrospective analysis of 14 cases of remote epidural hematoma as a postoperative complication after intracranial tumor resection. World J Surg Oncol. 2016. 14: 1