Abstract
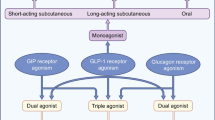
Type 2 diabetes mellitus is associated with a progressive decline in insulinproducing pancreatic β-cells, an increase in hepatic glucose production, and a decrease in insulin sensitivity. The incretin hormones glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) stimulate glucose-induced insulin secretion; however, in patients with type 2 diabetes, the incretin system is impaired by loss of the insulinotropic effects of GIP as well as a possible reduction in secretion of GLP-1. Agents that modify GLP-1 secretion may have a role in the management of type 2 diabetes. The currently available incretin-based therapies, GLP-1 receptor agonists (incretin mimetics) and dipeptidyl peptidase-4 (DPP-4) inhibitors (CD26 antigen inhibitors) [incretin enhancers], are safe and effective in the treatment of type 2 diabetes. However, they may be unable to halt the progression of type 2 diabetes, perhaps because they do not increase secretion of endogenous GLP-1. Therapies that directly target intestinal L cells to stimulate secretion of endogenous GLP-1 could possibly prove more effective than treatment with GLP-1 receptor agonists and DPP-4 inhibitors. Potential new approaches to modifying intestinal GLP-1 secretion in patients with type 2 diabetes include G-protein-coupled receptor (GPCR) agonists, α-glucosidase inhibitors, peroxisome proliferator-activated receptor (PPAR) agonists, metformin, bile acid mimetics and bile acid sequestrants. Both the GPCR agonist AR231453 and the novel bile acid mimetic INT-777 have been shown to stimulate GLP-1 release, leading to increased insulin secretion and improved glucose tolerance in mice. Similarly, a study in insulin-resistant rats demonstrated that the bile acid sequestrant colesevelam increased GLP-1 secretion and improved glucose levels and insulin resistance. In addition, the bile acid sequestrant colestimide (colestilan) has been shown to increase GLP-1 secretion and decrease glucose levels in patients with type 2 diabetes; these results suggest that the glucose-lowering effects of bile acid sequestrants may be partly due to their ability to increase endogenous GLP-1 levels. Evidence suggests that GPCR agonists, α-glucosidase inhibitors, PPAR agonists, metformin, bile acid mimetics and bile acid sequestrants may represent a new approach to management of type 2 diabetes via modification of endogenous GLP-1 secretion.





Similar content being viewed by others
References
National Diabetes Information Clearinghouse. National Diabetes Statistics, 2007 [online]. Available from URL: http://www.diabetes.niddk.nih.gov/dm/pubs/statistics/#allages [Accessed 2010 Mar 22]
Wild S, Roglic G, Green A, et al. Global prevalence of diabetes: estimates for the year 2000 and projections for 2030. Diabetes Care 2004 May; 27(5): 1047–53
Steffes MW, Sibley S, Jackson M, et al. Beta-cell function and the development of diabetes-related complications in the diabetes control and complications trial. Diabetes Care 2003 Mar; 26(3): 832–6
Panero F, Novelli G, Zucco C, et al. Fasting plasma C-peptide and micro- and macrovascular complications in a large clinic-based cohort of type 1 diabetic patients. Diabetes Care 2009 Feb; 32(2): 301–5
Holman RR, Paul SK, Bethel MA, et al. 10-year follow-up of intensive glucose control in type 2 diabetes. N Engl J Med 2008 Oct 9; 359(15): 1577–89
UK Prospective Diabetes Study Group. UK Prospective Diabetes Study 16. Overview of 6 years' therapy of type II diabetes: a progressive disease. Diabetes 1995 Nov; 44(11): 1249–58
Rudenski AS, Hadden DR, Atkinson AB, et al. Natural history of pancreatic islet B-cell function in type 2 diabetes mellitus studied over six years by homeostasis model assessment. Diabet Med 1988 Jan; 5(1): 36–41
Prando R, Odetti P, Melga P, et al. Progressive deterioration of beta-cell function in nonobese type 2 diabetic subjects: postprandial plasma C-peptide level is an indication of insulin dependency. Diabetes Metab 1996 Jun; 22(3): 185–91
Ostgren CJ, Lindblad U, Ranstam J, et al. Glycaemic control, disease duration and beta-cell function in patients with type 2 diabetes in a Swedish community. Skaraborg Hypertension and Diabetes Project. Diabet Med 2002 Feb; 19(2): 125–9
Amori RE, Lau J, Pittas AG. Efficacy and safety of incretin therapy in type 2 diabetes: systematic review and meta-analysis. JAMA 2007 Jul 11; 298(2): 194–206
Moretto TJ, Milton DR, Ridge TD, et al. Efficacy and tolerability of exenatide monotherapy over 24 weeks in antidiabetic drug-naive patients with type 2 diabetes: a randomized, double-blind, placebo-controlled, parallel-group study. Clin Ther 2008 Aug; 30(8): 1448–60
Zinman B, Hoogwerf BJ, Duran Garcia S, et al. The effect of adding exenatide to a thiazolidinedione in suboptimally controlled type 2 diabetes: a randomized trial. Ann Intern Med 2007 Apr 3; 146(7): 477–85
Aschner P, Kipnes MS, Lunceford JK, et al. Effect of the dipeptidyl peptidase-4 inhibitor sitagliptin as monotherapy on glycemic control in patients with type 2 diabetes. Diabetes Care 2006 Dec; 29(12): 2632–7
Rosenstock J, Sankoh S, List JF. Glucose-lowering activity of the dipeptidyl peptidase-4 inhibitor saxagliptin in drug-naive patients with type 2 diabetes. Diabetes Obes Metab 2008 May; 10(5): 376–86
DeFronzo RA, Fleck PR, Wilson CA, et al. Efficacy and safety of the dipeptidyl peptidase-4 inhibitor alogliptin in patients with type 2 diabetes and inadequate glycemic control: a randomized, double-blind, placebo-controlled study. Diabetes Care 2008 Dec; 31(12): 2315–7
Vilsboll T, Brock B, Perrild H, et al. Liraglutide, a once-daily human GLP-1 analogue, improves pancreatic B-cell function and arginine-stimulated insulin secretion during hyperglycaemia in patients with type 2 diabetes mellitus. Diabet Med 2008 Feb; 25(2): 152–6
Nauck M, Schmidt WE, Ebert R, et al. Insulinotropic properties of synthetic human gastric inhibitory polypeptide in man: interactions with glucose, phenylalanine, and cholecystokinin-8. J Clin Endocrinol Metab 1989 Sep; 69(3): 654–62
Kreymann B, Williams G, Ghatei MA, et al. Glucagon-like peptide-1 7–36: a physiological incretin in man. Lancet 1987 Dec 5; 2(8571): 1300–4
McIntyre N, Holdsworth CD, Turner DS. New interpretation of oral glucose tolerance. Lancet 1964 Jul 4; 2(7349): 20–1
Elrick H, Stimmler L, Hlad Jr CJ, et al. Plasma insulin response to oral and intravenous glucose administration. J Clin Endocrinol Metab 1964 Oct; 24: 1076–82
Nauck M, Stockmann F, Ebert R, et al. Reduced incretin effect in type 2 (non-insulin-dependent) diabetes. Diabetologia 1986 Jan; 29(1): 46–52
Vilsboll T, Krarup T, Deacon CF, et al. Reduced postprandial concentrations of intact biologically active glucagon-like peptide 1 in type 2 diabetic patients. Diabetes 2001 Mar; 50(3): 609–13
Vollmer K, Holst JJ, Baller B, et al. Predictors of incretin concentrations in subjects with normal, impaired, and diabetic glucose tolerance. Diabetes 2008 Mar; 57(3): 678–87
Nauck MA, Heimesaat MM, Orskov C, et al. Preserved incretin activity of glucagon-like peptide 1 [7-36 amide] but not of synthetic human gastric inhibitory polypeptide in patients with type-2 diabetes mellitus. J Clin Invest 1993 Jan; 91(1): 301–7
Ross SA, Brown JC, Dupre J. Hypersecretion of gastric inhibitory polypeptide following oral glucose in diabetes mellitus. Diabetes 1977 Jun; 26(6): 525–9
Crockett SE, Mazzaferri EL, Cataland S. Gastric inhibitory polypeptide (GIP) in maturity-onset diabetes mellitus. Diabetes 1976 Oct; 25(10): 931–5
Ebert R, Creutzfeldt W. Hypo- and hypersecretion of GIP in maturity-onset diabetics [abstract]. Diabetologia 1980; 19: 271–2
Meier JJ, Nauck MA. Is the diminished incretin effect in type 2 diabetes just an epi-phenomenon of impaired beta-cell function? Diabetes 2010 May; 59(5): 1117–25
Meier JJ, Nauck MA. Is secretion of glucagon-like peptide-1 reduced in type 2 diabetes mellitus? Nat Clin Pract Endocrinol Metab 2008 Nov; 4(11): 606–7
Toft-Nielsen MB, Damholt MB, Madsbad S, et al. Determinants of the impaired secretion of glucagon-like peptide-1 in type 2 diabetic patients. J Clin Endocrinol Metab 2001 Aug; 86(8): 3717–23
Mannucci E, Ognibene A, Cremasco F, et al. Glucagon-like peptide (GLP)-1 and leptin concentrations in obese patients with type 2 diabetes mellitus. Diabet Med 2000 Oct; 17(10): 713–9
Muscelli E, Mari A, Casolaro A, et al. Separate impact of obesity and glucose tolerance on the incretin effect in normal subjects and type 2 diabetic patients. Diabetes 2008 May; 57(5): 1340–8
Vilsboll T, Krarup T, Sonne J, et al. Incretin secretion in relation to meal size and body weight in healthy subjects and people with type 1 and type 2 diabetes mellitus. J Clin Endocrinol Metab 2003 Jun; 88(6): 2706–13
Theodorakis MJ, Carlson O, Michopoulos S, et al. Human duodenal enteroendocrine cells: source of both incretin peptides, GLP-1 and GIP. Am J Physiol Endocrinol Metab 2006 Mar; 290(3): E550–9
Orskov C, Jeppesen J, Madsbad S, et al. Proglucagon products in plasma of noninsulin-dependent diabetics and nondiabetic controls in the fasting state and after oral glucose and intravenous arginine. J Clin Invest 1991 Feb; 87(2): 415–23
Ahren B, Larsson H, Holst JJ. Reduced gastric inhibitory polypeptide but normal glucagon-like peptide 1 response to oral glucose in postmenopausal women with impaired glucose tolerance. Eur J Endocrinol 1997 Aug; 137(2): 127–31
Nauck MA, Vardarli I, Deacon CF, et al. Secretion of glucagon-like peptide-1 (GLP-1) in type 2 diabetes: what is up, what is down? Diabetologia 2011 Jan; 54(1): 10–8
Rask E, Olsson T, Soderberg S, et al. Impaired incretin response after a mixed meal is associated with insulin resistance in nondiabetic men. Diabetes Care 2001 Sep; 24(9): 1640–5
Vilsboll T, Krarup T, Madsbad S, et al. Defective amplification of the late phase insulin response to glucose by GIP in obese type II diabetic patients. Diabetologia 2002 Aug; 45(8): 1111–9
Nauck MA, Niedereichholz U, Ettler R, et al. Glucagon-like peptide 1 inhibition of gastric emptying outweighs its insulinotropic effects in healthy humans. Am J Physiol 1997 Nov;273 (5 Pt 1): E981–8
Herrmann C, Goke R, Richter G, et al. Glucagon-like peptide-1 and glucose-dependent insulin-releasing polypeptide plasma levels in response to nutrients. Digestion 1995; 56(2): 117–26
Crockett SE, Cataland S, Falko JM, et al. The insulinotropic effect of endogenous gastric inhibitory polypeptide in normal subjects. J Clin Endocrinol Metab 1976 Jun; 42(6): 1098–103
Eissele R, Goke R, Willemer S, et al. Glucagon-like peptide-1 cells in the gastrointestinal tract and pancreas of rat, pig and man. Eur J Clin Invest 1992 Apr; 22(4): 283–91
Mortensen K, Christensen LL, Holst JJ, et al. GLP-1 and GIP are colocalized in a subset of endocrine cells in the small intestine. Regul Pept 2003 Jul 15; 114(2-3): 189–96
Orskov C, Wettergren A, Holst JJ. Secretion of the incretin hormones glucagon-like peptide-1 and gastric inhibitory polypeptide correlates with insulin secretion in normal man throughout the day. Scand J Gastroenterol 1996 Jul; 31(7): 665–70
Hansen L, Deacon CF, Orskov C, et al. Glucagon-like peptide-1-(7–36)amide is transformed to glucagon-like peptide-1-(9–36)amide by dipeptidyl peptidase IV in the capillaries supplying the L cells of the porcine intestine. Endocrinology 1999 Nov; 140(11): 5356–63
Mentlein R. Dipeptidyl-peptidase IV (CD26): role in the inactivation of regulatory peptides. Regul Pept 1999 Nov 30; 85(1): 9–24
Vilsboll T, Agerso H, Krarup T, et al. Similar elimination rates of glucagon-like peptide-1 in obese type 2 diabetic patients and healthy subjects. J Clin Endocrinol Metab 2003 Jan; 88(1): 220–4
Deacon CF, Nauck MA, Meier J, et al. Degradation of endogenous and exogenous gastric inhibitory polypeptide in healthy and in type 2 diabetic subjects as revealed using a new assay for the intact peptide. J Clin Endocrinol Metab 2000 Oct; 85(10): 3575–81
Vilsboll T, Agerso H, Lauritsen T, et al. The elimination rates of intact GIP as well as its primary metabolite, GIP 3–42, are similar in type 2 diabetic patients and healthy subjects. Regul Pept 2006 Dec 10; 137(3): 168–72
Holst JJ. The physiology of glucagon-like peptide 1. Physiol Rev 2007 Oct; 87(4): 1409–39
Rocca AS, Brubaker PL. Role of the vagus nerve in mediating proximal nutrient-induced glucagon-like peptide-1 secretion. Endocrinology 1999 Apr; 140(4): 1687–94
Roberge JN, Brubaker PL. Regulation of intestinal proglucagon-derived peptide secretion by glucose-dependent insulinotropic peptide in a novel enteroendocrine loop. Endocrinology 1993 Jul; 133(1): 233–40
Brubaker PL. Regulation of intestinal proglucagon-derived peptide secretion by intestinal regulatory peptides. Endocrinology 1991 Jun; 128(6): 3175–82
Hansen L, Holst JJ. The effects of duodenal peptides on glucagon-like peptide-1 secretion from the ileum: a duo-deno-ileal loop? Regul Pept 2002 Dec 31; 110(1): 39–45
Hansen L, Lampert S, Mineo H, et al. Neural regulation of glucagon-like peptide-1 secretion in pigs. Am J Physiol Endocrinol Metab 2004 Nov; 287(5): E939–47
Layer P, Holst JJ, Grandt D, et al. Ileal release of glucagon-like peptide-1 (GLP-1): association with inhibition of gastric acid secretion in humans. Dig Dis Sci 1995 May; 40(5): 1074–82
American Diabetes Association. Dyslipidemia management in adults with diabetes. Diabetes Care 2004 Jan; 27 Suppl. 1: S68–71
Lim GE, Brubaker PL. Glucagon-like peptide 1 secretion by the L-cell. Diabetes 2006; 55 Suppl. 2: S70–S7
Anini Y, Brubaker PL. Muscarinic receptors control glu- cagon-like peptide 1 secretion by human endocrine L cells. Endocrinology 2003 Jul; 144(7): 3244–50
Anini Y, Hansotia T, Brubaker PL. Muscarinic receptors control postprandial release of glucagon-like peptide-1: in vivo and in vitro studies in rats. Endocrinology 2002 Jun; 143(6): 2420–6
Roberge JN, Gronau KA, Brubaker PL. Gastrin-releasing peptide is a novel mediator of proximal nutrient-induced proglucagon-derived peptide secretion from the distal gut. Endocrinology 1996 Jun; 137(6): 2383–8
Lu M, Wheeler MB, Leng XH, et al. The role of the free cytosolic calcium level in beta-cell signal transduction by gastric inhibitory polypeptide and glucagon-like peptide I(7-37). Endocrinology 1993 Jan; 132(1): 94–100
Ding WG, Gromada J. Protein kinase A-dependent stimulation of exocytosis in mouse pancreatic beta-cells by glucose-dependent insulinotropic polypeptide. Diabetes 1997 Apr; 46(4): 615–21
Lahlou H, Guillermet J, Hortala M, et al. Molecular signaling of somatostatin receptors. Ann N Y Acad Sci 2004 Apr; 1014: 121–31
Gameiro A, Reimann F, Habib AM, et al. The neurotransmitters glycine and GABA stimulate glucagon-like peptide-1 release from the GLUTag cell line. J Physiol 2005 Dec 15; 569 (Pt 3): 761–72
Reimann F, Habib AM, Tolhurst G, et al. Glucose sensing in L cells: a primary cell study. Cell Metab 2008 Dec; 8(6): 532–9
Hirasawa A, Tsumaya K, Awaji T, et al. Free fatty acids regulate gut incretin glucagon-like peptide-1 secretion through GPR120. Nat Med 2005 Jan; 11(1): 90–4
Elliott RM, Morgan LM, Tredger JA, et al. Glucagon-like peptide-1 (7–36)amide and glucose-dependent insulinotropic polypeptide secretion in response to nutrient ingestion in man: acute post-prandial and 24-h secretion patterns. J Endocrinol 1993 Jul; 138(1): 159–66
Holst JJ. On the physiology of GIP and GLP-1. Horm Metab Res 2004 Nov–Dec; 36(11-12): 747–54
Gautier JF, Choukem SP, Girard J. Physiology of incretins (GIP and GLP-1) and abnormalities in type 2 diabetes. Diabetes Metab 2008 Feb; 34 Suppl. 2: S65–72
Kim W, Egan JM. The role of incretins in glucose homeostasis and diabetes treatment. Pharmacol Rev 2008 Dec; 60(4): 470–512
Holst JJ, Vilsboll T, Deacon CF. The incretin system and its role in type 2 diabetes mellitus. Mol Cell Endocrinol 2009 Jan 15; 297(1-2): 127–36
Pamir N, Lynn FC, Buchan AM, et al. Glucose-dependent insulinotropic polypeptide receptor null mice exhibit compensatory changes in the enteroinsular axis. Am J Physiol Endocrinol Metab 2003 May; 284(5): E931–9
Trumper A, Trumper K, Trusheim H, et al. Glucose-dependent insulinotropic polypeptide is a growth factor for beta (INS-1) cells by pleiotropic signaling. Mol Endocrinol 2001 Sep; 15(9): 1559–70
Xu G, Kaneto H, Lopez-Avalos MD, et al. GLP-1/exendin-4 facilitates beta-cell neogenesis in rat and human pancreatic ducts. Diabetes Res Clin Pract 2006 Jul; 73(1): 107–10
Kim SJ, Winter K, Nian C, et al. Glucose-dependent insulinotropic polypeptide (GIP) stimulation of pancreatic beta-cell survival is dependent upon phosphatidylinositol 3-kinase (PI3K)/protein kinase B (PKB) signaling, inactivation of the forkhead transcription factor Foxo1, and down-regulation of bax expression. J Biologic Chem 2005 Jun 10; 280(23): 22297–307
Farilla L, Bulotta A, Hirshberg B, et al. Glucagon-like peptide 1 inhibits cell apoptosis and improves glucose responsiveness of freshly isolated human islets. Endocrinology 2003 Dec; 144(12): 5149–58
Prigeon RL, Quddusi S, Paty B, et al. Suppression of glucose production by GLP-1 independent of islet hormones: a novel extrapancreatic effect. Am J Physiol Endocrinol Metab 2003 Oct; 285(4): E701–7
Yamada C, Yamada Y, Tsukiyama K, et al. The murine glucagon-like peptide-1 receptor is essential for control of bone resorption. Endocrinology 2008 Feb; 149(2): 574–9
Xie D, Zhong Q, Ding KH, et al. Glucose-dependent insulinotropic peptide-overexpressing transgenic mice have increased bone mass. Bone 2007 May; 40(5): 1352–60
Meier JJ, Gallwitz B, Siepmann N, et al. Gastric inhibitory polypeptide (GIP) dose-dependently stimulates glucagon secretion in healthy human subjects at euglycaemia. Diabetologia 2003 Jun; 46(6): 798–801
Luque MA, Gonzalez N, Marquez L, et al. Glucagon-like peptide-1 (GLP-1) and glucose metabolism in human myocytes. J Endocrinol 2002 Jun; 173(3): 465–73
Flint A, Raben A, Astrup A, et al. Glucagon-like peptide 1 promotes satiety and suppresses energy intake in humans. J Clin Invest 1998 Feb 1; 101(3): 515–20
Gutzwiller JP, Drewe J, Goke B, et al. Glucagon-like peptide-1 promotes satiety and reduces food intake in patients with diabetes mellitus type 2. Am J Physiol 1999 May; 276 (5 Pt 2): R1541–4
Nikolaidis LA, Mankad S, Sokos GG, et al. Effects of glucagon-like peptide-1 in patients with acute myocardial infarction and left ventricular dysfunction after successful reperfusion. Circulation 2004 Mar 2; 109(8): 962–5
Meier JJ, Gethmann A, Gotze O, et al. Glucagon-like peptide 1 abolishes the postprandial rise in triglyceride concentrations and lowers levels of non-esterified fatty acids in humans. Diabetologia 2006 Mar; 49(3): 452–8
Hsieh J, Longuet C, Baker CL, et al. The glucagon-like peptide 1 receptor is essential for postprandial lipoprotein synthesis and secretion in hamsters and mice. Diabetologia 2010 Mar; 53(3): 552–61
Polonsky KS, Given BD, Hirsch LJ, et al. Abnormal patterns of insulin secretion in non-insulin-dependent diabetes mellitus. N Engl J Med 1988 May 12; 318(19): 1231–9
DeFronzo RA, Simonson D, Ferrannini E. Hepatic and peripheral insulin resistance: a common feature of type 2 (non-insulin-dependent) and type 1 (insulin-dependent) diabetes mellitus. Diabetologia 1982 Oct; 23(4): 313–9
Unger RH, Aguilar-Parada E, Muller WA, et al. Studies of pancreatic alpha cell function in normal and diabetic subjects. J Clin Invest 1970 Apr; 49(4): 837–48
Butler AE, Janson J, Bonner-Weir S, et al. Beta-cell deficit and increased beta-cell apoptosis in humans with type 2 diabetes. Diabetes 2003 Jan; 52(1): 102–10
Nguyen NT, Nguyen XM, Lane J, et al. Relationship between obesity and diabetes in a US adult population: findings from the National Health and Nutrition Examination Survey, 1999–2006. Obes Surg 2011 Mar; 21(3): 351–5
Campbell RK, Miller S. New therapeutic horizons: mapping the future of glycemic control with incretin-based therapy. Diabetes Educ 2009 Sep–Oct; 35(5): 731–4, 8–40, 42-4 passim
Pratley RE, Kipnes MS, Fleck PR, et al. Efficacy and safety of the dipeptidyl peptidase-4 inhibitor alogliptin in patients with type 2 diabetes inadequately controlled by glyburide monotherapy. Diabetes Obes Metab 2009 Feb; 11(2): 167–76
Knop FK. Bile-induced secretion of glucagon-like peptide-1: pathophysiological implications in type 2 diabetes? Am J Physiol Endocrinol Metab 2010 Jul; 299(1): E10–3
Chu ZL, Carroll C, Alfonso J, et al. A role for intestinal endocrine cell-expressed g protein-coupled receptor 119 in glycemic control by enhancing glucagon-like peptide-1 and glucose-dependent insulinotropic peptide release. Endocrinology 2008 May; 149(5): 2038–47
Turton MD, O'Shea D, Gunn I, et al. A role for glucagon-like peptide-1 in the central regulation of feeding. Nature 1996 Jan 4; 379(6560): 69–72
Chu ZL, Jones RM, He H, et al. A role for beta-cell-expressed G protein-coupled receptor 119 in glycemic control by enhancing glucose-dependent insulin release [Published erratum appears in Endocrinology 2007 Oct; 148 (10): 4753]. Endocrinology 2007 Jun; 148(6): 2601–9
Scheen AJ. Is there a role for alpha-glucosidase inhibitors in the prevention of type 2 diabetes mellitus? Drugs 2003; 63(10): 933–51
Lee A, Patrick P, Wishart J, et al. The effects of miglitol on glucagon-like peptide-1 secretion and appetite sensations in obese type 2 diabetics. Diabetes Obes Metab 2002 Sep; 4(5): 329–35
Goke B, Fuder H, Wieckhorst G, et al. Voglibose (AO-128) is an efficient alpha-glucosidase inhibitor and mobilizes the endogenous GLP-1 reserve. Digestion 1995; 56(6): 493–501
Qualmann C, Nauck MA, Holst JJ, et al. Glucagon-like peptide 1 (7–36 amide) secretion in response to luminal sucrose from the upper and lower gut: a study using alpha-glucosidase inhibition (acarbose). Scand J Gastroenterol 1995 Sep; 30(9): 892–6
Seifarth C, Bergmann J, Holst JJ, et al. Prolonged and enhanced secretion of glucagon-like peptide 1 (7–36 amide) after oral sucrose due to alpha-glucosidase inhibition (acarbose) in type 2 diabetic patients. Diabet Med 1998 Jun; 15(6): 485–91
Arakawa M, Ebato C, Mita T, et al. Miglitol suppresses the postprandial increase in interleukin 6 and enhances active glucagon-like peptide 1 secretion in viscerally obese subjects. Metabolism 2008 Sep; 57(9): 1299–306
Hucking K, Kostic Z, Pox C, et al. Alpha-glucosidase inhibition (acarbose) fails to enhance secretion of glucagon-like peptide 1 (7–36 amide) and to delay gastric emptying in type 2 diabetic patients. Diabet Med 2005 Apr; 22(4): 470–6
Moritoh Y, Takeuchi K, Hazama M. Chronic administration of voglibose, an alpha-glucosidase inhibitor, increases active glucagon-like peptide-1 levels by increasing its secretion and decreasing dipeptidyl peptidase-4 activity in ob/ob mice. J Pharmacol Exp Ther 2009 May; 329(2): 669–76
Daoudi M, Hennuyer N, Borland MG, et al. PPARbeta/ delta activation induces enteroendocrine L cell GLP-1 production. Gastroenterology 2011 May; 140(5): 1564–74
Wan J, Jiang L, Lu Q, et al. Activation of PPARdelta up-regulates fatty acid oxidation and energy uncoupling genes of mitochondria and reduces palmitate-induced apoptosis in pancreatic beta-cells. Biochem Biophys Res Commun 2010 Jan 15; 391(3): 1567–72
Coll T, Rodriguez-Calvo R, Barroso E, et al. Peroxisome proliferator-activated receptor (PPAR) beta/delta: a new potential therapeutic target for the treatment of metabolic syndrome. Curr Mol Pharmacol 2009 Jan; 2(1): 46–55
Maida A, Lamont BJ, Cao X, et al. Metformin regulates the incretin receptor axis via a pathway dependent on peroxisome proliferator-activated receptor in mice. Diabetologia 2011 Feb; 54(2): 339–49
Cho YM, Kieffer TJ. New aspects of an old drug: metformin as a glucagon-like peptide 1 (GLP-1) enhancer and sensitiser. Diabetologia 2011 Feb; 54(2): 219–22
Lauffer LM, Grieco A, Iakoubov R, et al. Metformin activates the AMPK pathway and improves survival of murine and human L-cells but does not directly increase GLP-1 secretion [abstract 198]. Diabetologia 2009; 52 Suppl. 1: S87
Yao X, Chen L, McIntyre MS, et al. Biguanide antidiabetic agents increase fecal bile acids via inhibition of apical sodium-dependent bile acid transporter [abstract 611-P]. Diabetes 2010; (Suppl. 1): 59
Migoya EM, Bergeron R, Miller JL, et al. Dipeptidyl peptidase-4 inhibitors administered in combination with metformin result in an additive increase in the plasma concentration of active GLP-1. Clin Pharmacol Ther Dec 2010; 88(6): 801–8
Katsuma S, Hirasawa A, Tsujimoto G. Bile acids promote glucagon-like peptide-1 secretion through TGR5 in a murine enteroendocrine cell line STC-1. Biochem Biophys Res Comm 2005 Apr 1; 329(1): 386–90
Thomas C, Gioiello A, Noriega L, et al. TGR5-mediated bile acid sensing controls glucose homeostasis. Cell Metab 2009 Sep; 10(3): 167–77
Patti ME, Houten SM, Bianco AC, et al. Serum bile acids are higher in humans with prior gastric bypass: potential contribution to improved glucose and lipid metabolism. Obesity 2009 Sep; 17(9): 1671–7
{le} Roux CW, Aylwin SJ, Batterham RL, et al. Gut hormone profiles following bariatric surgery favor an anorectic state, facilitate weight loss, and improve metabolic parameters. Ann Surg 2006 Jan; 243(1): 108–14
Goldberg RB, Fonseca VA, Truitt KE, et al. Efficacy and safety of colesevelam in patients with type 2 diabetes mellitus and inadequate glycemic control receiving insulin-based therapy. Arch Intern Med 2008 Jul 28; 168(14): 1531–40
Fonseca VA, Rosenstock J, Wang AC, et al. Colesevelam HCl improves glycemic control and reduces LDL cholesterol in patients with inadequately controlled type 2 diabetes on sulfonylurea-based therapy. Diabetes Care 2008 Aug; 31(8): 1479–84
Bays HE, Goldberg RB, Truitt KE, et al. Colesevelam hydrochloride therapy in patients with type 2 diabetes mellitus treated with metformin: glucose and lipid effects. Arch Intern Med 2008 Oct 13; 168(18): 1975–83
Shang Q, Saumoy M, Holst JJ, et al. Colesevelam improves insulin resistance in a diet-induced obesity (F-DIO) rat model by increasing the release of GLP-1. Am J Physiol Gastrointest Liver Physiol 2010; 298(3): G419–24
Suzuki T, Oba K, Igari Y, et al. Colestimide lowers plasma glucose levels and increases plasma glucagon-like PEPTIDE- 1 (7–36) levels in patients with type 2 diabetes mellitus complicated by hypercholesterolemia. J Nippon Med Sch 2007 Oct; 74(5): 338–43
Bays HE, Cohen DE. Rationale and design of a prospective clinical trial program to evaluate the glucose-lowering effects of colesevelam HCl in patients with type 2 diabetes mellitus. Curr Med Res Opin 2007 Jul; 23(7): 1673–84
Staels B, Kuipers F. Bile acid sequestrants and the treatment of type 2 diabetes mellitus. Drugs 2007; 67(10): 1383–92
Garg A, Grundy SM. Cholestyramine therapy for dyslipidemia in non-insulin-dependent diabetes mellitus: a short-term, double-blind, crossover trial. Ann Intern Med 1994 Sep 15; 121(6): 416–22
Guzelian P, Boyer JL. Glucose reabsorption from bile: evidence for a biliohepatic circulation. J Clin Invest 1974 Feb; 53(2): 526–35
Chiang JY, Kimmel R, Weinberger C, et al. Farnesoid X receptor responds to bile acids and represses cholesterol 7alpha-hydroxylase gene (CYP7A1) transcription. J Biol Chem 2000 Apr 14; 275(15): 10918–24
Acknowledgements
Funding for medical writing services was provided by Daiichi Sankyo, Inc., Parsippany, NJ, USA. Dr Holst has received research grants from Merck and Novartis, served as a consultant for Merck and NovoNordisk, and served as a speaker for Amylin Pharmaceuticals, GlaxoSmithKline, Novartis and NovoNordisk. Maria McGill is a medical writer employed by inScience Communications, a Wolters Kluwer business.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Holst, J.J., McGill, M.A. Potential New Approaches to Modifying Intestinal GLP-1 Secretion in Patients with Type 2 Diabetes Mellitus. Clin Drug Investig 32, 1–14 (2012). https://doi.org/10.2165/11595370-000000000-00000
Published:
Issue Date:
DOI: https://doi.org/10.2165/11595370-000000000-00000