Abstract
Background: Use of pregnancy registries is a common method of postmarketing surveillance of pregnancy outcomes to identify potential teratogens. However, with the increase in electronic capture of healthcare data for administrative, audit and research purposes, data generated during routine clinical practice might be used to address questions similar to those explored using pregnancy registries.
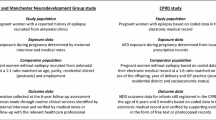
Objectives: To establish how data from the UK General Practice Research Database (GPRD) compares with data from the UK Epilepsy and Pregnancy Register and to assess how it can contribute to postmarketing surveillance of pregnancy outcomes.
Methods: Pregnancy outcomes were identified from the GPRD for women aged 14–49 years with a diagnosis of epilepsy and supporting evidence. Outcomes with a major congenital malformation (MCM) were identified and the relative risks (RRs) of an MCM following a range of first-trimester anti-epileptic drug (AED) exposures were calculated and compared with those reported by the UK Epilepsy and Pregnancy Register. In addition, we also evaluated whether the known association between valproate and spina bifida could be identified using data from the GPRD. The study period ran from 1 January 1990 until 31 December 2006.
Results: A total of 1766 live mother-baby pairs were identified, as well as 551 pregnancy terminations, 13 stillbirths and 1 neonatal death. Including those that resulted in a termination, there were 62 unique pregnancy outcomes with an MCM. An increased risk of spina bifida was identified using the GPRD following first-trimester monotherapy exposure to valproate when compared with those with no AED exposure (RR 8.02; 95% CI 1.5, 43.5). More generally, comparing the GPRD with the UK register, the GPRD ascertained a lower number of first-trimester AED exposures: monotherapy 711 versus 2468; polytherapy 156 versus 718. We reproduced the UK register results of an increased MCM risk following first-trimester polytherapy AED exposure compared with no AED exposure (RR 2.89; 95% CI 1.43, 5.84). Using the GPRD, we identified similar point estimates to the UK register following monotherapy and polytherapy exposures (4.1% vs 3.7% and 7.1% vs 6.0%, respectively) but we were unable to reproduce the level of statistical significance. For individual AEDs, the MCM rate following valproate exposure was 4.9% (11/225) in the GPRD compared with 6.2% (44/715) in the UK register.
Conclusions: The GPRD has potential for the identification of malformations and of a teratogenic association. For epilepsy, the GPRD does, however, identify fewer exposed pregnancies than a pregnancy registry. Therefore, in many circumstances pregnancy registries are likely to remain preferable as a method of surveillance. The GPRD may be better suited to monitoring medicines used in the treatment of more prevalent conditions, such as depression, or for monitoring medicines that have been on the market for a long time and for which no registry has been set up.







Similar content being viewed by others
Notes
1AEDs included acetazolamide, beclamide, carbamazepine, clobazam, clonazepam, ethosuximide, gabapentin, lamotrigine, levetiracetam, oxcarbazepine, phenobarbital (phenobarbitone), phenytoin, pregabalin, tiagabine, topiramate, valproate and vigabatrin.
References
Honein MA, Paulozzi LJ, Cragan JD, et al. Evaluation of selected characteristics of pregnancy drug registries. Teratology 1999; 60: 356–64
Schirm E, Meijer WM, Tobi H, et al. Drug use by pregnant women and comparable non-pregnant women in The Netherlands with reference to the Australian classification system. Eur J Obstet Gynecol Reprod Biol 2004; 114(2): 182–8
Lakha F, Glasier A. Unintended pregnancy and use of emergency contraception among a large cohort of women attending for antenatal care or abortion in Scotland. Lancet 2006; 368(9549): 1782–7
Henshaw SK. Unintended pregnancy in the United States. Fam Plann Perspect 1998; 30(1): 24–9
Koren G, Pastuszak A, Ito S. Drugs in pregnancy. N Engl J Med 1998; 338(16): 1128–37
Mitchell A. Special considerations in studies of drug-induced birth defects. In: Strom BL, editor. Pharmaco-epidemiology. 3rd ed. Chichester: John Wiley and Sons Ltd
Charlton RA, Cunnington MC, de Vries CS, et al. Data resources for investigating drug exposure during pregnancy and associated outcomes: the General Practice Research Database (GPRD) as an alternative to pregnancy registries. Drug Saf 2008; 31(1): 39–51
Hardy JR, Holford TR, Hall GC, et al. Strategies for identifying pregnancies in the automated medical records of the General Practice Research Database. Pharmacoepidemiol Drug Saf 2004; 13: 749–59
Snowball JM, de Vries CS. Determination of pregnancy on the General Practice Research Database [abstract]. Pharmacoepidemiol Drug Saf 2007; 16: S118
Devine S, West S, Andrews E, et al. The identification of pregnancies within the General Practice Research Database. Pharmacoepidemiol Drug Saf 2010; 19(1): 45–50
Hardy JR, Leaderer BP, Holford TR, et al. Safety of medications prescribed before and during early pregnancy in a cohort of 81 975 mothers from the UK General Practice Research Database. Pharmacoepidemiol Drug Saf 2006; 15: 555–64
Wurst KE, Ephross SA, Loehr J, et al. The utility of the general practice research database to examine selected congenital heart defects: a validation study. Pharmaco-epidemiol Drug Saf 2007; 16: 867–77
Devine S, West SL, Andrews E, et al. Validation of neural tube defects in the full featured-general practice research database. Pharmacoepidemiol Drug Saf 2008; 17: 434–44
Morrow J, Russell A, Guthrie E, et al. Malformation risks of antiepileptic drugs in pregnancy: a prospective study from the UK Epilepsy and Pregnancy Register. J Neurol Neurosurg Psychiatry 2006; 77(2): 193–8
Robert E, Guibaud P. Maternal valproic acid and congenital neural tube defects [letter]. Lancet 1982; II: 937
Lindhout D, Meinardi H. Spina bifida and in-utero exposure to valproate [letter]. Lancet 1984; II: 396
Dolk H, Jentink J, Loane M, et al., on behalf of the EUROCAT Antiepileptic Drug Working Group. Does lamotrigine use in pregnancy increase orofacial cleft risk relative to other malformations? Neurology 2008; 71: 714–22
Wood L, Martinez C. The General Practice Research Database: role in pharmacovigilance. Drug Saf 2004; 27(12): 871–81
MHRA. The General Practice Research Database (2009) [online]. Available from URL: http://www.gprd.com/home/default.asp [Accessed 2010 Mar 1]
Charlton RA, Weil JG, Cunnington MC, et al. Identifying major congenital malformations in the UK General Practice Research Database (GPRD): a study reporting on the sensitivity and added value of photocopied medical records and free text in the GPRD. Drug Saf 2010; 33(9): 741–50
Hart AC, Hopkins CA, editors. ICD-9-CM professional for hospitals. Vol. 1, 2 and 3. International classification of 171 diseases 9th revision, clinical modification. 6th ed. Reston (VA): Ingenix Inc., St Anthony Publishing/Medicode, 2003
EUROCAT. List of minor anomalies for exclusion up to birth year 2004 [online]. Available from URL: http://www.eurocat-network.eu/content/EUROCAT-Old-List-Minor-Anomalies.pdf [Accessed 2010 Feb 6]
EUROCAT. Minoranomalies for exclusion (chapter 3.2, guide 1.3) 2005 [online]. Available from URL: http://www.eurocat-network.eu/content/EUROCAT-Guide-1.3.pdf [Accessed 2010 Feb 6]
Kendle International Inc. The lamotrigine pregnancy registry: interim report, 1 September 1992 through 31 March 2009 [online]. Available from URL: http://pregnancyregistry.gsk.com/documents/lam_report_spring2009.pdf [Accessed 2010 Feb 6]
Mitchell A. Systematic identification of drugs that cause birth defects: a new opportunity. N Engl J Med 2003; 349(26): 2556–9
Charlton RA, Cunnington M, Weil JG, et al. Regarding the need, or lack thereof, of a comparator group for pregnancy registries [letter]. Birth Defects Res A Clin Mol Teratol 2009; 85: 808
Samren EB, van Duijn CM, Christiaens GCML, et al. Anti-epileptic drug regimens and major congenital abnormalities in the offspring. Ann Neurol 1999; 46: 739–46
Kaneko S, Battino D, Andermann E, et al. Congenital malformations due to antiepileptic drugs. Epilepsy Res 1999; 33(2–3): 145–58
Wide K, Winbladh B, Kallen B. Major malformations in infants exposed to antiepileptic drugs in utero, with emphasis on carbamazepine and valproic acid: a nation-wide, population-based register study. Acta Paediatr 2004; 93: 174–6
Wyszynski DF, Nambisan M, Surve T, et al. Increased rate of major malformations in offspring exposed to valproate during pregnancy. Neurology 2005; 64(6): 961–5
Vajda FJE, O’Brien T, Hitchcock A, et al. Antiepileptic drugs in pregnancy: great promise from pregnancy registries. J Clin Neurosci 2005; 10: 543–9
Acknowledgements
The authors wish to thank Brinda Bhaskar for her contribution to the early stages of the programming and analyses. This study is based in part on data from the Full Feature GPRD obtained under licence from the UK MHRA, and covers the data collection time period up to 31 March 2007. However, the interpretation and conclusions contained in this report are those of the authors alone. The study was funded in part by GlaxoSmithKline and in part by the University of Bath. Drs Cunnington and Weil and Mrs Ray are employees of GlaxoSmithKline, and Miss Charlton is a past employee of GlaxoSmithKline. Drs Cunnington and Weil and Miss Charlton hold shares in GlaxoSmithKline. Professor de Vries has no conflicts of interest that are relevant to the content of this study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Charlton, R.A., Weil, J.G., Cunnington, M.C. et al. Comparing the General Practice Research Database and the UK Epilepsy and Pregnancy Register as Tools for Postmarketing Teratogen Surveillance. Drug-Safety 34, 157–171 (2011). https://doi.org/10.2165/11584970-000000000-00000
Published:
Issue Date:
DOI: https://doi.org/10.2165/11584970-000000000-00000