Abstract
Background: The role of probiotics in the treatment of atopic dermatitis (AD) remains controversial. A recent systematic review of the available evidence called for further clinical trials with new probiotic formulations.
Objective: To assess the clinical efficacy and impact of Lactobacillus acidophilus DDS-1, Bifidobacterium lactis UABLA-12 with fructo-oligosaccharide on peripheral blood lymphocyte subsets in preschool children with moderate-to-severe AD.
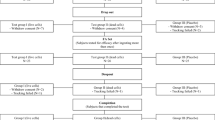
Method: Randomized, double-blind, placebo-controlled, prospective trial of 90 children aged 1–3 years with moderate-to-severe AD who were treated with a mixture of L. acidophilus DDS-1, B. lactis UABLA-12 with fructo-oligosaccharide at a dosage of 5 billion colony-forming units twice daily for 8 weeks versus placebo. The primary outcome measure was the percentage change in Scoring of Atopic Dermatitis (SCORAD) value. Other outcome measures were changes in Infant Dermatitis Quality Of Life (IDQOL) and Dermatitis Family Impact (DFI) scores, frequency and amount of topical corticosteroid used, and lymphocyte subsets in peripheral blood measured by laser flow cytometry.
Results: At the final visit, the percentage decrease in SCORAD was 33.7% in the probiotic group compared with 19.4% in the placebo group (p = 0.001). Children receiving probiotic showed a greater decrease in the mean [SD] SCORAD score than did children from the placebo group at week 8 (−14.2 [9.9] vs −7.8 [7.7], respectively; p = 0.001). IDQOL and DFI scores decreased significantly from baseline by 33.0% and 35.2% in the probiotic group and by 19.0% and 23.8% in the placebo group, respectively (p = 0.013, p = 0.010). Use of topical corticosteroids during the 8-week trial period averaged 7.7 g less in probiotic patients (p = 0.006). CD3, CD16, and CD22 lymphocyte subsets remained unchanged, whereas the percentage of CD4, and the percentage and absolute count of CD25 decreased, and the percentage and absolute count of CD8 increased in the probiotic group at week 8 (p < 0.007 vs placebo). There was a significant correlation between CD4 percentage, CD25 percentage, CD25 absolute count, and SCORAD values (r = 0.642, r = 0.746, r = 0.733, respectively; p < 0.05) in the probiotic group at week 8.
Conclusion: The administration of a probiotic mixture containing L. acidophilus DDS-1, B. lactis UABLA- 12, and fructo-oligosaccharide was associated with significant clinical improvement in children with AD, with corresponding lymphocyte subset changes in peripheral blood. The efficacy of probiotic therapy in adults with AD requires further investigation.








Similar content being viewed by others
References
Schultz LF, Diepgen T, Svensson A. The occurrence of atopic dermatitis in north Europe: an international questionnaire study. J Am Acad Dermatol 1996; 34: 760–4
Laughter D, Istvan JA, Tofte SJ, et al. The prevalence of atopic dermatitis in Oregon schoolchildren. J Am Acad Dermatol 2000; 43: 649–55
Schultz LF, Hanifin JM. Secular change in the occurrence of atopic dermatitis. Acta Derm Venereol Suppl (Stockh) 1992; 176: 7–12
Hanifin J, Tofte S. Patient education in the long-term management of atopic dermatitis. Dermatol Nurs 1999; 11: 284–9
Lapidus CS, Schwartz DF, Honig PJ. Atopic dermatitis in children: who cares? Who pays? J Am Acad Dermatol 1993; 28: 699–703
Akdis CA, Akdis M, Bieber T, et al. Diagnosis and treatment of atopic dermatitis in children and adults: European Academy ofAllergology and Clinical Immunology/American Academy of Allergy, Asthma and Immunology/ PRACTALL Consensus Report. Allergy 2006; 61: 969–87
Strachan DP. Hay fever, hygiene, and household size. BMJ 1989; 299: 1259–60
Prescott SL, Macaubas C, Smallacombe T, et al. Development of allergenspecific T-cell memory in atopic and normal children. Lancet 1999; 353: 196–200
Heller F, Duchmann R. Intestinal flora and mucosal immune responses. Int J Med Microbiol 2003; 293 (1): 77–86
Neaville WA, Tisler C, Bhattacharya A, et al. Developmental cytokine response profiles and the clinical and immunologic expression of atopy during the first year of life. J Allergy Clin Immunol 2003; 112 (4): 740–6
Sepp E, Julga K, Vasar M, et al. Intestinal microflora of Estonian and Swedish infants. Acta Paediatr 1997; 86: 956–61
Kalliomaki M, Kirjavainen P, Eerola E, et al. Distinct patterns of neonatal gut microflora in infants developing or not developing atopy. J Allergy Clin Immunol 2001; 107 (1): 129–34
Majamaa H, Isolauri E. Probiotics: a novel approach in the management of food atopic allergy. J Allergy Clin Immunol 1997; 99 (2): 179–85
Isolauri E, Arvola T, Sutas Y, et al. Probiotics in the management of atopic eczema. Clin Exp Allergy 2000; 30 (11): 1604–10
Rosenfeldt V, Benfeldt E, Nielsen SD, et al.Effect of probioticLactobacillus strains in children with atopic dermatitis. J Allergy Clin Immunol 2003; 111: 389–95
Weston S, Halbert A, Richmond P, et al. Effects of probiotics on atopic dermatitis: randomized controlled trial. Arch Dis Child 2005; 90 (9): 892–7
Viljanen M, Kuitunen M, Haahtela T, et al. Probiotic effects on faecal inflammatory markers and on faecal IgA in food allergic atopic eczema/ dermatitis syndrome in infants. Pediatr Allergy Immunol 2005; 16: 65–71
Sistek D, Kelly R, Wickens K, et al. Is the effect of probiotics on atopic dermatitis confined to food sensitized children? Clin Exp Allergy 2006; 36 (5): 629–33
Folster-Holst R, Muller F, Schnopp N, et al. Prospective, randomised controlled on Lactobacillus rhamnosus in infants with moderate to severe atopic allergy and non-allergic dermatitis. Br J Dermatol 2006; 155: 1256–61
Grüber C, Wendt M, Sulser C, et al. Randomized, placebo-controlled trial of Lactobacillus rhamnosus GG as treatment of atopic dermatitis in infancy. Allergy 2007; 62 (11): 1270–6
Brouwer ML, Wolt-Plompen SA, Dubois AE, et al. No effects of probiotics on atopic dermatitis in infancy: a randomized placebo-controlled trial. Clin Exp Allergy 2006; 36 (7): 899–906
Betsi GI, Papadavid E, Falagas ME. Probiotics for the treatment and prevention of atopic dermatitis: a review of the evidence from randomized controlled trials. Am J Clin Dermatol 2008; 9 (2): 93–103
Boyle RJ, Bath-Hextall FJ, Leonardi-Bee J, et al. Probiotics for treating eczema. Cochrane Database Syst Rev 2008; (4): CD006135
Wickens K, Black PN, Stanley TV. A differential effect of 2 probiotics in the prevention of eczema and atopy: a double-blind, randomized, placebocontrolled trial. J Allergy Clin Immunol 2008; 122 (4): 788–94
Sawada J, Morita H, Tanaka A, et al. Ingestion of heat-treated Lactobacillus rhamnosus GG prevents development of atopic dermatitis in NC/Nga mice. Clin Exp Allergy 2007; 37: 296–303
Machura E, Mazur B, Golemiec E, et al. Staphylococcus aureus skin colonization in atopic dermatitis children is associated with decreased IFN-gamma production by peripheral blood CD4+ and CD8+ T cells. Pediatr Allergy Immunol 2008; 19: 37–45
Roessler A, Friedrich U, Vogelsang H, et al. The immune system in healthy adults and patients with atopic dermatitis seems to be affected differently by a probiotic intervention. Clin Exp Allergy 2007; 38: 93–102
Leung DY, Rhodes AR, Geha RS. Enumeration of T cell subsets in atopic dermatitis using monoclonal antibodies. J Allergy Clin Immunol 1981; 67 (6): 450–5
Chandra RK, Baker M.Numerical and functional deficiency of suppressor T cells precedes development of atopic eczema. Lancet 1983; 17 (2): 1393–4
Hanifin M, Rajka G. Diagnostic features of atopic dermatitis. Acta Dermatol Venerol 1980; 114: S146–8
Niggemann B. Role of oral food challenges in the diagnostic work-up of food allergy in atopic eczema dermatitis syndrome.Allergy 2004; 59 Suppl. 78: 32–4
[No authors listed]. Severity scoring of atopic dermatitis: the SCORAD index. Consensus report of the European Task Force on Atopic dermatitis. Dermatology 1993; 186: 23–31
Lewis-Jones MS, Finlay AY, Dykes PJ. The Infants’ Dermatitis Quality of Life Index. Br J Dermatol 2001; 144 (1): 104–10
Lawson V, Lewis-Jones SM, Finlay AY, et al. The family impact of childhood atopic dermatitis: the Dermatitis Family Impact questionnaire. J Dermatol 1998; 138: 107–13
Kunz B, Oranje A, Labreze L, et al. Clinical validation and guidelines for the SCORAD index: consensus report of the European Task Force on Atopic Dermatitis. Dermatology 1997; 195 (1): 10–9
Hessle C, Hanson LA, Wold AE. Lactobacilli from human gastrointestinal mucosa are strong stimulators of IL-12 production. Clin Exp Immunol 1999; 116: 276–82
Miettinen M, Matikainen S, Vuopio-Varkila J, et al. Lactobacilli and streptococci induce interleukin-12 (IL-12), IL-18, and gamma interferon production in human peripheral blood mononuclear cells. Infect Immun 1998; 66: 6058–62
Pessi T, Sutas Y, Hurme M, et al. Interleukin-10 generation in atopic children following oral Lactobacillus rhamnosus GG. Clin Exp Allergy 2000; 30: 1804–8
Arslanoglu S, Moro GE, Schmitt J, et al. Early dietary intervention with a mixture of prebiotic oligosaccharides reduces the incidence of allergic manifestations and infections during the first two years of life. J Nutr 2008; 138 (6): 1091–5
Passeron T, Lacour JP, Fontas E, et al. Prebiotics and synbiotics: two promising approaches for the treatment of atopic dermatitis in children above 2 years. Allergy 2006; 61 (4): 431–7
Grillo M, Ng M, Gassner L, et al. Pediatric atopic eczema: the impact of an educational intervention. Pediatr Dermatol 2006; 23 (5): 428–36
Acknowledgments
This study was funded by Lviv National Medical University (Ukraine). The authors acknowledge the provision of DDS® Junior bottles by UAS Laboratories (USA), and would like to thank Drs Lewis-Jones and Finley (UK) for permission to use the IDQOL and DFI questionnaires in the study. The authors are also grateful to Prof. M. Thaler (USA) for careful revision of the manuscript. The authors have no conflicts of interest that are directly relevant to the content of this study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Gerasimov, S.V., Vasjuta, V.V., Myhovych, O.O. et al. Probiotic Supplement Reduces Atopic Dermatitis in Preschool Children. Am J Clin Dermatol 11, 351–361 (2010). https://doi.org/10.2165/11531420-000000000-00000
Published:
Issue Date:
DOI: https://doi.org/10.2165/11531420-000000000-00000