Abstract
This article briefly summarizes the burden of bipolar disorder and the clinical profile of quetiapine (Seroquel®) in the management of bipolar disorder, followed by a detailed review of pharmacoeconomic analyses. Quetiapine is an atypical antipsychotic that is available in numerous countries as immediate-release and extended-release tablets for the treatment of major psychiatric disorders, including bipolar disorder. Randomized, double-blind, placebo-controlled trials with quetiapine have demonstrated its efficacy in bipolar I and II disorders, and the drug has been generally well tolerated in clinical trials.
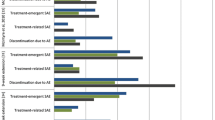
Three cost-effectiveness analyses of maintenance therapy in bipolar I disorder, which used similar Markov models and incorporated data from key clinical trials and a number of other sources, showed that quetiapine, as adjunctive therapy with mood stabilizers (lithium or divalproex), was a cost-effective treatment option from the healthcare payer perspective in the UK and the US. Quetiapine either dominated comparators (typically mood stabilizers alone) or was associated with incremental cost-effectiveness ratios that were usually well below widely accepted thresholds of cost effectiveness. One of the studies evaluated extended-release quetiapine, although clinical efficacy data used in the Markov model were for the immediate-release formulation. In another analysis, which used a discrete-event simulation model and was conducted from the perspective of the UK healthcare payer, quetiapine monotherapy was cost effective compared with olanzapine monotherapy as maintenance treatment for all phases of bipolar I or II disorder. In this model, favourable results were also shown for quetiapine (with or without mood stabilizers) compared with a wide range of maintenance therapy regimens. Another modelled analysis conducted from the UK healthcare payer perspective showed that quetiapine was dominated by haloperidol in the short-term treatment of a manic episode in patients with bipolar I disorder. Both favourable and unfavourable results have been reported in cost analyses of quetiapine in bipolar disorder (type I or type not specified).
Possible explanations for some of the variability in results of the pharmacoeconomic analyses include heterogeneity among the models in terms of input parameters or assumptions in the base-case analyses, country- or region-specific differences in estimates of healthcare resource use and associated costs, variability in treatment alternatives, and differences in the year of costing and discounting used in the analyses. In addition, some of the studies had short time horizons and focused on acute manic episodes only, whereas others were longer-term analyses that considered the full spectrum of health states in patients with bipolar disorder. Various limitations of the studies have been recognized, and results from one country may not be applicable to other countries.
In conclusion, results of available pharmacoeconomic analyses provide evidence of the cost effectiveness of quetiapine as an adjunct to mood stabilizers for maintenance therapy in (primarily type I) bipolar disorder from a healthcare payer perspective in the UK and the US. Some evidence is available to support the cost effectiveness of quetiapine monotherapy or the use of extended-release quetiapine as adjunctive therapy with mood stabilizers in this setting, although further analyses appear to be warranted. Whether these findings apply to other geographical regions requires further study. Evidence for the long-term (>2-year) cost effectiveness of quetiapine in bipolar disorder is currently limited and further studies are also needed to address the cost effectiveness of quetiapine from a societal perspective and in bipolar II disorder.



Similar content being viewed by others
References
Kupfer DJ. The increasing medical burden in bipolar disorder. JAMA 2005 May 25; 293 (20): 2528–30
Michalak EE, Murray G, Young AH, et al. Burden of bipolar depression: impact of disorder and medications on quality of life. CNS Drugs 2008; 22 (5): 389–406
Kessler RC, Berglund P, Demler O, et al. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry 2005 Jun; 62 (6): 593–602
American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th ed. Washington, DC: American Psyciatric Association, 2000
Manning JS. Burden of illness in bipolar depression. Prim Care Companion J Clin Psych 2006; 7 (6): 259–67
Malhi GS, Adams D, Cahill CM, et al. The management of individuals with bipolar disorder: a review of the evidence and its integration into clinical practice. Drugs 2009 Oct 22; 69 (15): 2063–101
Scott J, Colom F, Popova E, et al. Long-term mental health resource utilization and cost of care following group psychoeducation or unstructured group support for bipolar disorders: a cost-benefit analysis. J Clin Psychiatry 2009; 70 (3): 378–86
National Institute for Health and Clinical Excellence. Bipolar disorder: the management of bipolar disorder in adults, children and adolescents, in primary and secondary care (NICE clinical guideline no. 38) [online]. Available from URL: http://publications.nice.org.uk/bipolar-disorder-cg38 [Accessed 2011 Dec 5]
Hirschfeld RMA. Guideline watch: practice guideline for the treatment of patients with bipolar disorder. 2nd ed. American Psychiatric Association [online]. Available from URL: http://psychiatryonline.org/content.aspx?bookid=28§ionid=1682557 [Accessed 2011 Dec 5]
Fleurence RL, Dixon JM, Revicki DA. Economics of atypical antipsychotics in bipolar disorder: a review of the literature. CNS Drugs 2006; 20 (7): 591–9
AstraZeneca. Seroquel® (quetiapine fumarate) tablets: US prescribing information [online]. Available from URL: http://www1.astrazeneca-us.com/pi/Seroquel.pdf [Accessed 2011 Oct 3]
AstraZeneca. Seroquel XR® (quetiapine fumarate) extended-release tablets: US prescribing information [online]. Available from URL: http://www1.astrazeneca-us.com/pi/seroquelxr.pdf [Accessed 2011 Oct 3]
AstraZeneca. Seroquel® (quetiapine) film-coated tablets: summary of product characteristics [online]. Available from URL: http://www.medicines.org.uk/emc/medicine/2295 [Accessed 2011 Oct 3]
AstraZeneca. Seroquel® (quetiapine) prolonged-release tablets: summary of product characteristics [online]. Available from URL: http://www.medicines.org.uk/emc/medicine/21175 [Accessed 2011 Oct 3]
Fajutrao L, Locklear J, Priaulx J, et al. A systematic review of the evidence of the burden of bipolar disorder in Europe. Clin Pract Epidemiol Ment Health 2009; 5: 3
Bryant-Comstock L, Stender M, Devercelli G. Health care utilization and costs among privately insured patients with bipolar I disorder. Bipolar Disord 2002 Dec; 4 (6): 398–405
Weissman MM, Bland RC, Canino GJ, et al. Cross-national epidemiology of major depression and bipolar disorder. JAMA 1996; 276 (4): 293–9
Hirschfeld RM, Vornik LA. Bipolar disorder: costs and comorbidity. Am J Manag Care 2005 Jun; 11 (3 Suppl.): S85–90
Frye MA, Calabrese JR, Reed ML, et al. Healthcare resource utilization in bipolar depression compared with unipolar depression: results of a United States population-based study. CNS Spectr 2006 Sep; 11 (9): 704–10
Kasper S. Issues in the treatment of bipolar disorder. Eur Neuropsychopharmacol 2003 Aug; 13 Suppl. 2: S37–42
Murray CJ, Lopez AD. Global mortality, disability, and the contribution of risk factors: global burden of disease study. Lancet 1997 May 17; 349 (9063): 1436–42
Wyatt RJ, Henter I. An economic evaluation of manic-depressive illness: 1991. Soc Psychiatry Psychiatr Epidemiol 1995 Aug; 30 (5): 213–9
Das Gupta R, Guest JF. Annual cost of bipolar disorder to UK society. Br J Psychiatry 2002 Mar; 180: 227–33
Hakkaart-van Roijen L, Hoeijenbos MB, Regeer EJ, et al. The societal costs and quality of life of patients suffering from bipolar disorder in the Netherlands. Acta Psychiatr Scand 2004 Nov; 110 (5): 383–92
Runge C, Grunze H. Annual costs of bipolar disorders in Germany [in German]. Nervenarzt 2004 Sep; 75 (9): 896–903
Begley CE, Annegers JF, Swann AC, et al. The lifetime cost of bipolar disorder in the US: an estimate for new cases in 1998. Pharmacoeconomics 2001; 19 (5 Pt 1): 483–95
Peele PB, Xu Y, Kupfer DJ. Insurance expenditures on bipolar disorder: clinical and parity implications. Am J Psychiatry 2003 Jul; 160 (7): 1286–90
Simon GE, Unutzer J. Health care utilization and costs among patients treated for bipolar disorder in an insured population. Psychiatr Serv 1999 Oct; 50 (10): 1303–8
Stender M, Bryant-Comstock L, Phillips S. Medical resource use among patients treated for bipolar disorder: a retrospective, cross-sectional, descriptive analysis. Clin Ther 2002 Oct; 24 (10): 1668–76
Perlick D, Clarkin JF, Sirey J, et al. Burden experienced by care-givers of persons with bipolar affective disorder. Br J Psychiatry 1999 Jul; 175: 56–62
Chatterton ML, Ke X, Lewis BE, et al. Impact of bipolar disorder on the family: utilization and cost of health care resources. P T 2008 Jan; 33 (1): 15–34
Turner EH, Matthews AM, Linardatos E, et al. Selective publication of antidepressant trials and its influence on apparent efficacy. N Engl J Med 2008 Jan 17; 358 (3): 252–60
Chiesa A, Chierzi F, De Ronchi D, et al. Quetiapine for bipolar depression: a systematic review and meta-analysis. Int Clin Psychopharmacol 2012 Mar; 27 (2): 76–90
Vieta E, Gunther O, Locklear J, et al. Effectiveness of psychotropic medications in the maintenance phase of bipolar disorder: a meta-analysis of randomized controlled trials. Int J Neuropsychopharmacol 2011 Sep; 14 (8): 1029–49
Vieta E, Locklear J, Gunther O, et al. Treatment options for bipolar depression: a systematic review of randomized, controlled trials. J Clin Psychopharmacol 2010 Oct; 30 (5): 579–90
Sanford M, Keating GM. Quetiapine: a review of its use in the management of bipolar depression. CNS Drugs. In press
Keating GM, Robinson DM. Quetiapine: a review of its use in the treatment of bipolar depression. Drugs 2007; 67 (7): 1077–95
Cristancho MA, Thase ME. The role of quetiapine extended release in the treatment of bipolar depression. Adv Ther 2010 Nov; 27 (11): 774–84
Brahm NC, Gutierres SL, Carnahan RM. Quetiapine for acute mania in bipolar disorder. Am J Health Syst Pharm 2007 May 15; 64 (10): 1045–53
Cipriani A, Barbui C, Salanti G, et al. Comparative efficacy and acceptability of antimanic drugs in acute mania: a multiple-treatments meta-analysis. Lancet 2011 Oct 8; 378 (9799): 1306–15
Bowden CL, Grunze H, Mullen J, et al. A randomized, double-blind, placebo-controlled efficacy and safety study of quetiapine or lithium as monotherapy for mania in bipolar disorder. J Clin Psychiatry 2005 Jan; 66 (1): 111–21
McIntyre RS, Brecher M, Paulsson B, et al. Quetiapine or haloperidol as monotherapy for bipolar mania: a 12-week, double-blind, randomised, parallel-group, placebo-controlled trial. Eur Neuropsychopharmacol 2005 Oct; 15 (5): 573–85
Sachs G, Chengappa KN, Suppes T, et al. Quetiapine with lithium or divalproex for the treatment of bipolar mania: a randomized, double-blind, placebo-controlled study. Bipolar Disord 2004 Jun; 6 (3): 213–23
Calabrese JR, Keck Jr PE, Macfadden W, et al. A randomized, double-blind, placebo-controlled trial of quetiapine in the treatment of bipolar I or II depression. Am J Psychiatry 2005 Jul; 162 (7): 1351–60
McElroy SL, Weisler RH, Chang W, et al. A double-blind, placebo-controlled study of quetiapine and paroxetine as monotherapy in adults with bipolar depression (EMBOLDEN II). J Clin Psychiatry 2010 Feb; 71 (2): 163–74
Suppes T, Datto C, Minkwitz M, et al. Effectiveness of the extended release formulation of quetiapine as monotherapy for the treatment of acute bipolar depression. J Affect Disord 2010 Feb 1; 121: 106–15
Thase ME, Macfadden W, Weisler RH, et al. Efficacy of quetiapine monotherapy in bipolar I and II depression: a double-blind, placebo-controlled study (the BOLDER II study). J Clin Psychopharmacol 2006 Dec; 26 (6): 600–9
Young AH, McElroy SL, Bauer M, et al. A double-blind, placebo-controlled study of quetiapine and lithium monotherapy in adults in the acute phase of bipolar depression (EMBOLDEN I). J Clin Psychiatry 2010 Feb; 71 (2): 150–62
Suppes T, Vieta E, Liu S, et al. Maintenance treatment for patients with bipolar I disorder: results from a North American study of quetiapine in combination with lithium or divalproex (trial 127). Am J Psychiatry 2009 Apr; 166 (4): 476–88
Vieta E, Suppes T, Eggens I, et al. Efficacy and safety of quetiapine in combination with lithium or divalproex for maintenance of patients with bipolar I disorder (international trial 126). J Affect Disord 2008 Aug; 109 (3): 251–63
Weisler RH, Nolen WA, Neijber A, et al. Continuation of quetiapine versus switching to placebo or lithium for maintenance treatment of bipolar I disorder (trial 144: a randomized controlled study). J Clin Psychiatry 2011 Nov; 72(11): 1452–64
Gianfrancesco F, Pesa J, Wang RH. Comparison of mental health resources used by patients with bipolar disorder treated with risperidone, olanzapine, or quetiapine. J Manage Care Pharm 2005 Apr; 11 (3): 220–30
Jing Y, Kim E, You M, et al. Healthcare costs associated with treatment of bipolar disorder using a mood stabilizer plus adjunctive aripiprazole, quetiapine, risperidone, olanzapine or ziprasidone. J Med Econ 2009 Jun; 12 (2): 104–13
Gianfrancesco F, Rajagopalan K, Goldberg JF, et al. Hospitalization risks in the treatment of bipolar disorder: comparison of antipsychotic medications. Bipolar Disord 2007 May; 9 (3): 252–61
Qiu Y, Christensen DB, Fu AZ, et al. Cost analysis in a Medicaid program for patients with bipolar disorder who initiated atypical antipsychotic monotherapy. Curr Med Res Opin 2009 Feb; 25 (2): 351–61
Caro JJ, Huybrechts KF, Xenakis JG, et al. Budgetary impact of treating acute bipolar mania in hospitalized patients with quetiapine: an economic analysis of clinical trials. Curr Med Res Opin 2006 Nov; 22 (11): 2233–42
Klok RM, Al Hadithy AF, van Schayk NP, et al. Pharmacoeconomics of quetiapine for the management of acute mania in bipolar I disorder. Expert Rev 2007 Oct; 7 (5): 459–67
Fajutrao L, Paulsson B, Liu S, et al. Cost-effectiveness of quetiapine plus mood stabilizers compared with mood stabilizers alone in the maintenance therapy of bipolar I disorder: results of a Markov model analysis. Clin Ther 2009 Jun; 31 Pt 1: 1456–68
Woodward TC, Tafesse E, Quon P, et al. Cost-effectiveness of quetiapine with lithium or divalproex for maintenance treatment of bipolar I disorder. J Med Econ 2009; 12 (4): 259–68
Woodward TC, Tafesse E, Quon P, et al. Cost effectiveness of adjunctive quetiapine fumarate extended-release tablets with mood stabilizers in the maintenance treatment of bipolar I disorder. Pharmacoeconomics 2010 Sep 1; 28 (9): 751–64
Bridle C, Palmer S, Bagnall AM, et al. A rapid and systematic review and economic evaluation of the clinical and cost-effectiveness of newer drugs for treatment of mania associated with bipolar affective disorder. Health Technol Assess 2004 May; 8 (19): iii–v
Ekman M, Lindgren P, Miltenburger C, et al. Cost effectiveness of quetiapine in patients with acute bipolar depression and in maintenance treatment after an acute depressive episode. Pharmacoeconomics 2012; 30 (6): 513–30
National Institute for Health and Clinical Excellence. Guide to the methods of technology appraisal. London: NICE, 2008 Jun [online]. Available from URL: http://www.nice.org.uk/media/B52/A7/TAMethodsGuideUpdatedJune2008.pdf [Accessed 2011 Apr 7]
Boersma C, Broere A, Postma MJ. Quantification of the potential impact of cost-effectiveness thresholds on Dutch drug expenditures using retrospective analysis. Value Health 2010; 13 (6): 853–6
Jonsson B. Changing health environment: the challenge to demonstrate cost-effectiveness of new compounds. Pharmacoeconomics 2004; 22 Suppl. 4: 5–10
Eichler HG, Kong SX, Gerth WC, et al. Use of cost-effectiveness analysis in health-care resource allocation decision-making: how are cost-effectiveness thresholds expected to emerge? Value Health 2004; 7 (5): 518–28
Figueroa C, Brecher M, Hamer-Maansson JE, et al. Pharmacokinetic profiles of extended release quetiapine fumarate compared with quetiapine immediate release. Prog Neuropsychopharmacol Biol Psychiatry 2009 Mar 17; 33 (2): 199–204
Caldwell DM, Ades AE, Higgins JPT. Simultaneous comparison of multiple treatments: combining direct and indirect evidence. BMJ 2005 Oct 15; 331: 897–900
Hillman AL, Eisenberg JM, Pauly MV, et al. Avoiding bias in the conduct and reporting of cost-effectiveness research sponsored by pharmaceutical companies. N Engl J Med 1991 May 9; 324 (19): 1362–5
Hassan M, Lage MJ. Risk of rehospitalization among bipolar disorder patients who are nonadherent to antipsychotic therapy after hospital discharge. Am J Health Syst Pharm 2009 Feb 15; 66 (4): 358–65
Gianfrancesco FD, Sajatovic M, Rajagopalan K, et al. Antipsychotic treatment adherence and associated mental health care use among individuals with bipolar disorder. Clin Ther 2008 Jul; 30 (7): 1358–74
Hassan M, Madhavan SS, Kalsekar ID, et al. Comparing adherence to and persistence with antipsychotic therapy among patients with bipolar disorder. Ann Pharmacother 2007 Nov; 41 (11): 1812–8
Gianfrancesco FD, Rajagopalan K, Sajatovic M, et al. Treatment adherence among patients with bipolar or manic disorder taking atypical and typical antipsychotics. J Clin Psychiatry 2006 Feb; 67 (2): 222–32
Author information
Authors and Affiliations
Corresponding author
Additional information
Various sections of the manuscript reviewed by: J.C. Bouvy, Division of Pharmacoepidemiology and Clinical Pharmacology, Utrecht Institute for Pharmaceutical Sciences, Utrecht University, Utrecht, the Netherlands; M. Geitona, School of Social Sciences, University of Peloponnese, Corinth, Greece; I. Mavranezouli, National Collaborating Centre for Mental Health, Centre for Outcomes, Research and Effectiveness (CORE), Department of Clinical, Educational and Health Psychology, University College London, London, UK; T. Stargardt, Hamburg Center for Health Economics, University of Hamburg, Hamburg, Germany.
Data Selection
Sources: Medical literature (including published and unpublished data) on ‘quetiapine’ was identified by searching databases since 1996 (including MEDLINE and EMBASE and in-house AdisBase), bibliographies from published literature, clinical trial registries/databases and websites (including those of regional regulatory agencies and the manufacturer). Additional information (including contributory unpublished data) was also requested from the company developing the drug.
Search strategy: MEDLINE search terms were ‘quetiapine’ and (‘bipolar disorder’ or ‘bipolar depression’ or ‘bipolar mania’) and (‘economics’ or ‘health-policy’ or ‘quality-of-life’ or ‘models-statistical’ or ‘health-planning’ or ‘epidemiology’ or ‘guideline in pt’ or ‘practice-guidelines in pt’). EMBASE search terms were ‘quetiapine’ and (‘bipolar disorder’ or ‘bipolar depression’ or ‘bipolar mania’) and (‘economics’ or ‘health economics’ or ‘economic evaluation’ or ‘health status’ or ‘pharmacoeconomics’ or ‘drug cost’ or ‘drug utilization’ or ‘utilization review’ or ‘health survey’ or ‘practice guideline’ or ‘quality of life’ or ‘treatment outcome’ or ‘cost’ or ‘cost benefit analysis’ or ‘cost control’ or ‘cost effectiveness analysis’ or ‘cost minimisation analysis’ or ‘cost of illness’ or ‘cost utility analysis’). AdisBase search terms were ‘quetiapine’ and (‘bipolar disorder’ or ‘bipolar’) and (‘mania’ or ‘depression’) and (‘health-economics’ or ‘pharmacoepidemiology’ or ‘prescribing’ or ‘hospitalisation’ or ‘formularies’ or ‘drug-utilisation’ or ‘meta-analysis’ or ‘therapeutic-substitution’ or ‘epidemiology’). Searches were last updated 26 March 2012.
Selection: Economic analyses in patients with bipolar disorder who received quetiapine. Inclusion of studies was based mainly on the methods section of the trials. Relevant background data on epidemiology and cost of illness are also included.
Index terms: Quetiapine, bipolar disorder, bipolar depression, bipolar mania, maintenance therapy, pharmacoeconomics, cost effectiveness, therapeutic use, tolerability.
Rights and permissions
About this article
Cite this article
Plosker, G.L. Quetiapine. PharmacoEconomics 30, 611–631 (2012). https://doi.org/10.2165/11208500-000000000-00000
Published:
Issue Date:
DOI: https://doi.org/10.2165/11208500-000000000-00000