Summary
Abstract
The humanised monoclonal antibody daclizumab is an immunosuppressive agent that reduces acute rejection in solid organ transplantation. It is specific for the α subunit (Tac/CD25) of the interleukin (IL)-2 receptor on activated T cells and achieves immunosuppression by competitive antagonism of IL-2-induced T cell proliferation.
When added to standard triple immunosuppression regimens, daclizumab significantly reduces the rate of acute rejection at 1 year in renal transplantation by 36% and there are indications that it may be effective in other solid organ transplantations. Three-year outcomes of two phase III clinical trials in renal transplantation indicate similar values for graft and patient survival between daclizumab and placebo when given in addition to triple immunosuppression; however, these pivotal trials were not designed with sufficient power to demonstrate any statistical significance.
The addition of daclizumab induction shows potential in allowing calcineurin inhibitor- and corticosteroid-sparing regimens without increasing the rate of acute graft rejection or adverse effects in renal and liver transplantation.
Preliminary reports indicate that daclizumab may also be a useful agent in delayed graft function and graft versus host disease (GVHD). Further investigation of its efficacy in these groups and in children is needed.
Data from clinical trials show daclizumab to be well tolerated in solid organ transplantation. It does not increase the incidence of infection, including cytomegalovirus infection, when compared with placebo or no induction groups. Preliminary comparative data with muromonab CD3 indicate that daclizumab may be associated with a lower rate of infectious complications and similar or better efficacy.
Conclusions: In conclusion, daclizumab has been proven to reduce acute rejection in renal transplant recipients when given in addition to traditional baseline immunosuppression. It has shown potential to reduce acute rejection in other solid organ transplants; however, well designed, randomised studies are required to confirm this.
Clinical experience from trials to date indicate that daclizumab has a tolerability profile similar to placebo with no significant effect on the incidence of infection. The relative efficacy and tolerability of daclizumab compared with other induction agents has yet to be defined. Available data suggest that daclizumab may allow the use of calcineurin inhibitor-sparing and corticosteroid-sparing regimens and may have potential in the treatment of GVHD.
Pharmacodynamic Properties
Daclizumab is a humanised monoclonal antibody which binds specifically to the α chain (Tac/CD25) of the IL-2 receptor (IL-2R) on the surface of activated lymphocytes. Pharmacodynamic studies suggest that daclizumab acts at the receptor level by inhibiting the association and subsequent phosphorylation of the IL-2R β and γ chains. Rapid saturation of lymphocytes (up to 95%) occurs and lasts for 90 to 120 days with a five-dose regimen. One- and two-dose regimens provide effective saturation for up to 70 days in renal transplantation.
Daclizumab competitively antagonises T cell proliferation induced by IL-2. It triggers antibody-dependent cell-mediated cytotoxicity, down-regulates IL-2R expression and increases the shedding of daclizumab-bound IL-2R. It may also have an effect on antibody-dependent cytotoxicity (type II) reactions mediated by monocytes and polymorphonuclear leucocytes and may impair the induction of activation-induced cell death.
Pharmacokinetic Properties
Available data suggest that the intravenous dose of daclizumab required to maintain sufficient serum concentrations to provide immunosuppression differs depending on the type of transplantation. A dose of 1 mg/kg given once every 2 weeks for a total of five doses in adult renal transplant recipients was sufficient to maintain therapeutic serum concentrations (5 to 10 mg/L). Peak serum concentrations reported with this regimen were 21 mg/L after the first dose and 32 mg/L after the fifth dose. The same regimen in liver transplant recipients became subtherapeutic within hours of the preoperative dose and within 4 to 6 days of the dose given immediately postoperatively. Probable causes include the large blood and fluid losses observed in liver transplantation. In small bowel and multiorgan transplant recipients an intravenous dose of 2 mg/kg given once every 2 weeks for six doses followed by 1 mg/kg for a further six doses was also subtherapeutic.
Daclizumab has a small volume of distribution (about 5.3L), and systemic clearance is low (estimated at 15.1 ml/h for an 80kg male renal transplant recipient). The elimination half-life varies, with mean values of approximately 20 days in renal and 3 to 4 days in bone marrow transplant recipients. Dosage adjustments are not required on the basis of age, race, gender or degree of proteinuria.
Therapeutic Efficacy
Renal Transplantation: Well designed studies have demonstrated the efficacy of a five-dose regimen of daclizumab 1 mg/kg in reducing the incidence of acute biopsy-proven rejection in renal transplant recipients receiving baseline immunosuppression.
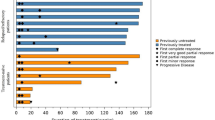
In 1-year pooled data from two large phase III multicentre studies, the rate of acute rejection was significantly lower (27.7 vs 43.3%, a reduction of 36%; p < 0.001), the mean number of rejection episodes in the first 6 months was significantly lower (0.5 vs 0.8; p < 0.001) and the median time to first rejection episode was longer (40 vs 18 days) in daclizumab-treated patients than in those receiving placebo. The number of patients requiring antilymphocyte therapy to treat rejection and the required doses of corticosteroids were significantly lower in daclizumab recipients versus placebo recipients in one of the trials.
Three-year outcomes of the two phase III clinical trials revealed that graft and patient survival were not significantly different between daclizumab and placebo in patients receiving triple therapy baseline immunosuppression. However, these trials were not sufficiently powered to reveal such a difference.
Evidence is unclear as to the comparative efficacy of daclizumab with that of muromonab CD3. Acute rejection rates were similar or lower in patients treated with daclizumab in retrospective studies and a tendency to a higher incidence of severe rejections was observed with daclizumab in one small randomised study. One large retrospective study in 169 patients reported a lower incidence of acute rejection (18 vs 32%; p < 0.005) and a significant lower decline in the rate of hospital readmission at 6 months (32 vs 50%; p < 0.005) for patients treated with daclizumab (n = 169) than for those receiving muromonab CD3 (n = 124).
Preliminary data from a small study (n = 23) suggest daclizumab and basiliximab have similar efficacy in the prevention of acute rejection in renal transplant recipients. Similar rates of patient and graft survival and time to first acute rejection were also reported.
A number of mostly noncomparative studies have indicated that daclizumab may have potential as part of a calcineurin inhibitor- or corticosteroid-sparing regimen; one study indicated a similar rate of acute rejection with a full-dose cyclosporin versus a half-dose cyclosporin regimen.
In small noncomparative trials using daclizumab in patients with delayed graft function, daclizumab enabled the delayed introduction of a calcineurin inhibitor without significantly increasing the rate of acute rejection.
Liver Transplantation: Preliminary information from two small trials suggest daclizumab and corticosteroid-free induction may reduce the rate of hepatitis C virus (HCV) recurrence in HCV-positive patients versus those that received standard corticosteroid treatment. In a noncomparative study where daclizumab 2 mg/kg was given weekly as part of a corticosteroid-free regimen, a significant reduction in hepatitis C viraemia in liver transplant recipients with recurrent HCV infection previously unresponsive to therapy was observed.
Daclizumab 1 mg/kg (1 dose) and delayed calcineurin inhibitor treatment appears not to reduce the rate of recurrence of hepatitis C infection versus early tacrolimus treatment in HCV-positive patients. In a comparative study, using daclizumab 1 mg/kg (one to three doses), a similar effect on the rates of acute rejection in both HCV-positive and -negative patients was observed.
Daclizumab appears to be effective in liver transplant recipients with impaired renal function, allowing delayed introduction of calcineurin inhibitors without an increase in the rate of acute rejection. At 1 month post-transplantation, two retrospective studies (n < 130) reported similar figures for patient (100 and 97.4%) and graft survival (100 and 97.4%) in daclizumab recipients. One trial found a statistically significant difference in acute rejection rates between daclizumab recipients and those receiving tacrolimus 0.1 mg/kg/day (18 vs 40%; p = 0.02) at 6 months post transplantation and the other reported a significantly shorter time to reach improved renal function in daclizumab recipients than for those receiving low-dose tacrolimus (3.6 vs 12.2 days; p = 0.05).
Some preliminary results on the use of daclizumab in corticosteroid-sparing regimens in liver transplant recipients appear promising.
There is some evidence that the dosage of daclizumab needs to be higher in patients undergoing liver transplantation than in those receiving renal transplants. This has been attributed to the heavy blood and fluid loss seen in liver transplantation.
Cardiac Transplantation: Daclizumab induction reduced the incidence (18 vs 63%; p < 0.05) and severity of acute rejection in cardiac transplant recipients who continued to receive baseline immunosuppression (n = 28) compared with patients not receiving induction (n = 27). Significantly fewer daclizumab-treated patients required rescue therapy with antilymphocyte therapy (3.6 vs 22.2%; p = 0.04).
Other Solid Organ Transplantation: In simultaneous pancreas-kidney transplantation, preliminary data indicate that daclizumab 1 mg/kg for two doses may reduce the rate of acute rejection compared with induction with muromonab CD3 5 mg/day for 10 days. However, one trial indicated no significant improvement in the rate of acute rejection over no induction in these patients. There is also preliminary evidence to indicate that daclizumab may reduce the rate of acute rejection and improve graft function in lung transplant recipients.
Preliminary information from small, poorly designed clinical trials among intestinal and multivisceral transplant recipients indicates reduced frequency and severity of biopsy-proven acute rejection in patients treated with daclizumab, 1 to 2 mg/kg fortnightly for up to 12 doses, compared with no induction.
Graft Versus Host Disease: Two small (n < 45), preliminary studies have investigated the efficacy of daclizumab in graft versus host disease. Complete response rates (complete resolution of rash) ranged from 27 to 47% with daclizumab 1 mg/kg weekly for five doses over a month (one study also used daily doses for the first 5 days), assessed at 28 to 43 days. Values reported for median duration of patient survival were 70 and >120 days and survival rates reported were 29 and 53% on day 120.
Paediatric Use: Reports from three preliminary studies in children, one in lung and two in renal transplant recipients, although poorly designed, have been encouraging. Two studies used a five-dose regimen of daclizumab 1 mg/kg given every 2 weeks and demonstrated lower rates of acute rejection in patients treated with daclizumab versus those receiving no induction. The third study among renal transplant recipients used daclizumab as part of a corticosteroid-free regimen and compared it with a regimen containing corticosteroids. Both regimens had low rates of acute rejection.
Tolerability
Data from clinical trials in renal and other solid organ transplantation indicate that daclizumab is well tolerated with a similar adverse events profile to placebo or no induction therapy. Daclizumab has a low potential for immunogenicity. Malignancy and lymphoproliferative disorders are uncommon and daclizumab is not associated with either local or systemic adverse events when administered through a peripheral vein.
Data from phase III clinical studies in renal transplantation showed gastrointestinal disturbance was the most common adverse event but it was not thought to be treatment related. Cellulitis and wound infections were the only adverse events that occurred more often in daclizumab than placebo recipients; however, this was not statistically significant.
Randomised studies in heart, liver and kidney/pancreas transplant recipients indicate a similar tolerability profile to that seen in renal transplantation. Infectious disorders including cytomegalovirus infection, fungal infections, pneumonia and local infections have been reported in daclizumab recipients; however, the incidence was no different from that in patients receiving no induction therapy.
Nonrandomised studies to date indicate that daclizumab may be associated with a lower incidence of infectious complications than muromonab CD3 in recipients of various solid organ transplants; however, further data from well designed trials are needed.
Daclizumab is well tolerated as part of a calcineurin inhibitor- or corticosteroid-sparing regimen and the tolerability in children appears to be similar to that in adults.
Dosage and Administration
Daclizumab is licensed for immunosuppression in renal transplantation in several markets worldwide including the US and Europe. The recommended dosage of daclizumab is 1 mg/kg administered within 24 hours before surgery and once every 2 weeks thereafter for a total of five doses. Daclizumab 1 mg/kg should be diluted in 50ml of sterile 0.9% saline and administered intravenously via a peripheral or central vein over a 15-minute period.
Many variations on this recommended dosage have been used in clinical trials both in renal and other forms of solid organ transplantation. The dose has varied from 1 to 2 mg/kg and the number of doses given has varied widely. Recent data in renal transplant recipients suggest a two-dose strategy may be as effective as a five-dose regimen.
No dosage adjustment is needed in severe renal impairment and no drug interactions have been reported.











Similar content being viewed by others
References
Vincenti F, Kirkman R, Light S, et al. Interleukin-2-receptor blockade with daclizumab to prevent acute rejection in renal transplantation. N Engl J Med 1998; 338: 161–5
Wiseman LR, Faulds D. Daclizumab: a review of its use in the prevention of acute rejection in renal transplant recipients. Drugs 1999; 58(6): 1029–42
Zenapax product monograph. Basel, Switzerland: F. Hoffmann-La Roche (Basel), 1997
Goebel J, Stevens E, Forrest K, et al. Daclizumab (Zenapax) inhibits early interleukin-2 receptor signal transduction events. Transplant Immunology 2000 Nov; 8(3): 153–9
Junghans RP, Waldmann TA, Landolfi NF, et al. Anti-Tac-H, a humanized antibody to the interleukin 2 receptor with new features for immunotherapy in malignant and immune disorders. Cancer Res 1990 Mar 1; 50: 1495–502
Xu H, Cruzata D, Tadaki DK, et al. The IL-2 receptor alpha chain (CD25) plays an important role in regulating CD40 expression during human anti-porcine cellular responses [online]. Available from URL: http://www.abstracts-on-line.com/abstracts/TRANS [Accessed 2001 May 21]
Vincenti F, Lantz M, Birnbaum J, et al. Aphase I trial of humanized anti-interleukin 2 receptor antibody in renal transplantation. Transplantation 1997; 63: 33–8
Baan CC, Boelaars-van Haperen MJAM, van Riemsdijk IC, et al. IL-7 and IL-15 bypass the immunosuppressive action of anti-CD25 monoclonal antibodies. Transplant Proc 2001; 33: 2244–6
Baan CC, Balk AH, Mol WM, et al. Anti-CD25 therapy affects the death signals of activated T-cells after clinical heart transplantation [abstract]. J Heart Lung Transplant 2001 Feb; 20: 220
ter Meulen CG, van Riemsdijk I, Hene RJ, et al. Two doses of daclizumab are sufficient for prolonged IL-2RA-chain blockade[online]. Available from URL: http://www.abstracts-on-line.com/abstracts/TRANS [Accessed 2001 May 21]
Vincenti F, Lantz MV, Birnbaum JL, et al. Pharmacokinetic and pharmacodynamic studies of one or two doses of daclizumab in renal transplant patients [online]. Available from URL: http://www.abstracts-on-line.com/abstracts/TRANS [Accessed 2001 May 21]
Hirose R, Roberts JP, Quan D, et al. Experience with daclizumab in liver transplantation: renal transplant dosing without calcineurin inhibitors is insufficient to prevent acute rejection in liver transplantation. Transplantation 2000; 69(2): 307–11
Carreño MR, Kato T, Weppler D, et al. Induction therapy with Daclizumab as part of the immunosuppressive regimen in human small bowel and multiorgan transplants. Transplant Proc 2001 Feb–Mar; 33: 1015–7
Hakimi J, Ha VC, Lin P, et al. Humanized Mikβ1, a humanized antibody to the IL-2 receptor β-chain that acts synergistically with humanized anti-TAC. J Immunol 1993 Jul 15; 151: 1075–85
Phillips KE, Herring B, Wilson LA, et al. IL-2R-alpha-directed monoclonal antibodies provide effective therapy in a murine model of adult T-cell leukemia by a mechanism other than blockade of IL-2/IL-2R-alpha interaction. Cancer Res 2000 Dec 15; 60: 6977–84
Summary of product characteristics for Zenapax (dacliximab). New Jersey, USA: F. Hoffmann-La Roche (NJ), 1997. Report no. RO 24-7375. (Data on file)
Nevins T, Ettenger R, Potter D, et al. Daclizumab (Zenapax) in pediatric (PED) renal allografts: final data [abstract no. 469]. Transplantation 1999; 67: S124
Anasetti C, Light SE, Waldmann TA, et al. Treatment of acute graft-versus-host disease with H-anti-TAC: a humanized antibody that binds to the interleukin-2 receptor. 1st International Symposium on Cytokines in Bone Marrow Transplantation 1993; 145
Nashan B, Light S, Hardie IR, et al. Reduction of acute renal allograft rejection by daclizumab. Transplantation 1999; 67: 110–5
Nelson DR, Soldevila-Pico C, Lauwers G, et al. The effect of anti-interleukin-2 receptor therapy on the course of hepatitis C recurrency after liver transplantation [abstract]. Hepatology 2000 Oct; 32 (Pt 2): 208
Heffron TG, Smallwood GA, de VM, et al. Hepatitis C recurrence following daclizumab induction in liver transplantation [abstract]. Hepatology 2000 Oct; 32 (Pt 2): 346
Beniaminovitz A, Itescu S, Lietz K, et al. Prevention of rejection in cardiac transplantation by blockade of the interleukin-2 receptor with a monoclonal antibody. N Engl J Med 2000; 342(9): 613–9
Van der Werf WJ, Reed AI, Hemming AW, et al. Two doses of daclizumab provides effective induction for simultaneous pancreas and kidney transplantations[online]. Available from URL: http://www.abstracts-on-line.com/abstracts/TRANS [Accessed 2001 May 21]
Garrity ER Jr, Villanueva J, Bhorade SM, et al. Low rate of acute lung allograft rejection after the use of daclizumab, an interleukin 2 receptor antibody. Transplantation 2001 Mar 27; 71(6): 773–7
Terasaki PI, Cecka JM, Gjertson DW. High survival rates of kidney transplants from spousal and living unrelated donors. N Engl J Med 1995 Aug 10; 333(6): 333–6
Smith CR, Woodward RS, Cohen DS. Cadaveric versus living donor kidney transplantation. Transplantation 2000 Jan 27; 69(2): 311–4
Iverson AJ, Vick SC, Sarnacki CT, et al. Daclizumab in live donor renal transplantation. Transplant Proc 2000; 32(4): 790–2
Rehman LU, Atkinson RC, Minich PJ. Two dose daclizumab (Zenapax) is safe and effective induction therapy in adult renal transplantation[online]. Available from URL: http://www.abstracts-on-line.com/abstracts/TRANS [Accessed 2001 May 21]
Ekberg H, Bäckman L, Tufveson G, et al. Daclizumab prevents acute rejection and improves patient survival post transplantation: 1 year pooled analysis. Transpl Int 2000; 13(2): 151–9
Vincenti F, Nashan B, Bumgardner G, et al. Three year outcome of the phase III clinical trials with daclizumab [abstract]. Transplantation 2000 Apr 27; 69 Suppl.: S261
Vincenti F. Daclizumab: novel biologic immunoprophylaxis for prevention of acute rejection in renal transplantation. Transplant Proc 1999 Sep; 31: 2206–7
Meier-Kriesche H-U, Kaza H, Palekar SS, et al. The effect of Daclizumab in a high-risk renal transplant population. Clin Transpl 2000; 14(5): 509–13
Lacha J, Simova M, Noskova L, et al. Zenapax versus OKT-3 prophylaxis in immunologically high-risk kidney transplant recipients [abstract]. Transplantation 2000 Apr 27; 69 Suppl.: S158
Deierhoi MH, Hudson SL, Gaston RS. Clinical experience with a two dose regimen of Daclizumab in cadaveric renal transplantation [abstract]. Transplantation 2000 Apr 27; 69 Suppl.: S260
Flapan D. Reduced regimen is safe and effective in kidney transplant recipients [online]. Available from URL: http://www.cardiology.medscape.com/MedscapeWire [Accessed 2001 May 15]
Nair MP, Nampoory MRN, Johny KV, et al. Induction immunosuppression with interleukin-2 receptor antibodies (basiliximab and daclizumab) in renal transplant recipients. Transplant Proc 2001 Aug; 33: 2767–9
Vincenti F, Ramos E, Brattstrom C, et al. Multicenter trial exploring calcineurin inhibitors avoidance in renal transplantation. Transplantation 2001 May 15; 71(9): 1282–7
Tran HTB, Acharya MK, McKay DB, et al. Avoidance of cyclosporine in renal transplantation: effects of daclizumab, mycophenolate mofetil, and steroids. J Am Soc Nephrol 2000; 11(10): 1903–9
Kreis H, Puget S, Mourad M, et al. Is it possible to reduce ciclosporin early with daclizumab and mycophenolate mofetil in renal transplant recipients? Preliminary results in 169 patients of a randomized multicentric trial [online]. Available from URL http://www.abstracts-on-line.com/abstracts/TRANS [Accessed 2001 May 21]
Landsberg DN, Cole EH, Russell D, et al. Renal transplantation without steroids — one year results of a multicentre Canadian pilot study [abstract]. Transplantation 2000 Apr 27; 69 Suppl.: S134
Ingle GR, Moudgil A, Vo A, et al. Daclizumab and mycophenolate mofetil reduce the need for cyclosporine without increasing risk for acute rejection in renal transplantation [online]. Available from URL: http://www.abstracts-on-line.com/abstracts [Accessed 2001 Mar 5]
Chang GJ, Mahanty HD, Vincenti F, et al. A calcineurin inhibitor-sparing regimen with sirolimus, mycophenolate mofetil, and anti-CD25 mAb provides effective immunosuppression in kidney transplant recipients with delayed or impaired graft function. Clin Transpl 2000; 14(6): 550–4
Golconda MS, Rayhill SC, Hunsicker LG. Daclizumab permits delayed introduction of calcineurin inhibitors in renal transplant recipients at risk for delayed graft function [abstract]. Transplantation 2000 Apr 27; 69(8) Suppl.: S158
Sarwal MM, Yorgin PD, Alexander S, et al. Promising early outcomes with a novel, complete steroid avoidance immunosuppression protocol in pediatric renal transplantation. Transplantation 2001 Jul 15; 72(1): 13–21
Islam KK, Rustgi VK, Kuo PC, et al. Zenapax and effect of clinical outcome of hepatitis C post liver transplant [abstract]. Gastroenterology 2000 Apr; 118Suppl. 2 (Pt 1): A995
Heffron T, Smallwood G, Pillen T, et al. Pediatric and adult evaluation of daclizumab as induction therapy following liver transplantation while witholding calcineurin inhibition [online]. Availablse from URL: http://www.abstracts-on-line.com/abstracts/TRANS [Accessed 2001 May 21]
Emre S, Gondolesi G, Polat K, et al. Use of daclizumab as initial immunosuppression in liver transplant recipients with impaired renal function. Liver Transpl 2001 Mar; 7: 220–5
Kato T, Neff G, Montalbano M, et al. Steroid-free induction with tacrolimus and daclizumab in liver transplant recipients with Hepatitis C-A preliminary report of a prospective randomized trial. Am J Transplant 2001; 1Suppl. 1: 179
Pinna AD, Ricordi C, Weppler D, et al. Treatment of recurrent hepatitis C after liver transplantation with IL-2r antibody. Transplant Proc 2001 Feb–Mar; 33: 1087–9
Marino G, Rustgi VK, Marroquin CE, et al. Early recurrence of hepatitis C after liver transplantation with daclizumab induction [online]. Available from URL: http://www.abstract-on-line.com/abstracts/TRANS [Accessed 2001 May 21]
Eckhoff DE, McGuire B, Sellers M, et al. The safety and efficacy of a two-dose daclizumab (Zenapax) induction therapy in liver transplant recipients. Transplantation 2000; 69(9): 1867–72
Washburn K, Speeg KV, Esterl R, et al. Liver transplantation using minimal steroids, prograf, cellcept and daclizumab [abstract]. Transplantation 2000 Apr 27; 69 Suppl.: S166
Mancini D, Beniaminovitz A, Edwards N, et al. Effect of daclizumab induction therapy on the development of cardiac transplant vasculopathy [abstract]. J Heart Lung Transplant 2001 Feb; 20: 194
Lietz K, Beniaminovitz A, Burke E, et al. Effectiveness of treatment with anti-Cd25 Mab to reduce immunologic risk factors for high-grade cardiac allograft rejection depends on donor/recipient HLA-DR matching [abstract]. Circulation 1999 Nov 2; 100 Suppl.: 1–526
Stratta RJ, Alloway RR, Lo A, et al. A multicenter trial of 2 daclizumab dosing strategies vs no antibody induction in simultaneous kidney-pancreas transplantation: interim analysis. Transplant Proc 2001 Feb–Mar; 33: 1692–3
Stratta RJ, Alloway RR, Lo A, et al. A multicenter, open label, comparative trial of 2 daclizumab dosing strategies vs no antibody induction in combination with tacrolimus, mycophenolate mofetil, and steroids in simultaneous kidney-pancreas transplantation: 6 month analysis. Am J Transplant 2001; 1Suppl. 1: 159
Dy-Liacco MS, Collins BH, Butterly DW, et al. A comparison of readmission rates of simultaneous kidney pancreas transplant recipients receiving induction with muromonab-CD3 versus Daclizumab [online]. Available from URL: http://www.abstracts-on-line.com/abstracts/TRANS/ [Acces sed 2001 May 21st]
58. Golconda MS, Rayhill SC, Hunsicker LG. A low rate of acute rejection in simultaneous pancreas-kidney transplant recipients receiving daclizumab induction [online]. Available from: URL: http://www.abstracts-on-line.com/abstracts/TRANS/ [Accessed 2001 May 21]
Hayney MS, Cornwell RD, Meyer KC, et al. Efficacy of interleukin-2 receptor antibodies in lung transplantation [abstract]. Am J Respir Crit Care Med 2000 Mar; 161 Suppl.(Pt2): 369
Sweet SC, De La Morena MT, Shapiro SD, et al. Interleukin-2-receptor blockade with daclizumab decreases the incidence of acute rejection in pediatric lung transplant recipients [abstract]. J Heart Lung Transplant 2001 Feb; 20: 221–2
Pinna AD, Weppler D, Nery JR, et al. Induction therapy for clinical intestinal transplantation: comparison of four different regimens. Transplant Proc 2000 Sep; 32: 1193–4
Shapiro AMJ, Lakey JRT, Ryan EA, et al. Islet transplantation in seven patients with type 1 diabetes mellitus using a glucocorticoid-free immunosuppressive regimen. N Engl J Med 2000; 343(4): 230–8
Shapiro AMJ, Ryan EA, Rajotte RV, et al. Two-year insulin independence and metabolic follow-up after islet-alone transplantation in autoimmune diabetes [online]. Available from: URL: http://www.abstracts-on-line.com/abstracts/ [Accessed 2001 Mar 5th]
Vogelsang GB, Morris LE. Prevention and management of graft-versus-host disease: practical recommendations. Drugs 1993 May; 45: 668–76
Ringdén O. Management of graft-versus-host disease. Eur J Haematol 1993 Jul; 51: 1–12
Przepiorka D, Kernan NA, Ippoliti C, et al. Daclizumab, a humanized anti-interleukin-2 receptor alpha chain antibody, for treatment of acute graft-versus-host disease. Blood 2000; 95(1): 83–9
Willenbacher W, Basara N, Kirsten D, et al. Treatment of severe steroid-resistant GVHD with a monoclonal interleukin-2 receptor antagonist (daclizumab [DC]) [abstract]. Bone Marrow Transplant 2000 Mar; 25Suppl. 1: S156
Villanueva J, Bhorade SM, McCabe MA, et al. Daclizumab, an anti-interleukin receptor antibody, may decrease the acute rejection in lung transplant patients [abstract]. J Heart Lung Transplant 2000 Jan; 19: 83
Abu-Elmagd K, Fung J, McGhee W, et al. The efficacy of daclizumab for intestinal transplantation: preliminary report. Transplant Proc 2000 Sep; 32: 1195–6
Ferguson R. Acute rejection episodes: best predictor of long-term primary cadaveric renal transplant survival. Clin Transpl 1994; 8(3): 328–31
Matas A. Chronic rejection in renal transplant recipients: risk factors and correlates. Clin Transpl 1994; 8(3): 332–5
Hariharan S, Alexander JW, Schroeder TJ, et al. Impact of first acute rejection episode and severity of rejection on cadaveric renal allograft survival. Clin Transpl 1996; 10(6): 538–41
Gaston RS, Meyer KV. Development and clinical utility of daclizumab (Zenapax registered), a humanized anti-Tac monoclonal antibody, in renal transplantation. Today’s Ther Trends 1998; 16(4): 309–24
Sarwal MM, Yorgin PD, Alexander S. Promising early outcomes with a novel, complete steroid avoidance immunosuppression protocol in pediatri renal transplantation [online]. Available from URL: http://www.abstracts-on-line.com/abstracts [Accessed 2001 Mar 5]
Denton MD, Magee CC, Sayegh MH. Immunosuppressive strategies in transplantation. Lancet 1999; 353(9158): 1083–91
Schrand LM. Recent additions to the growing biotechnology armamentarium: a critical assessment. Formulary 1999; 34(11): 920–42
Mazariegos GV, Salzedas AA, Zavatsky J, et al. Long term management of liver transplant rejection in children. BioDrugs 2000; 14(1): 31–48
Simulect (basiliximab) product monograph. Basel, Switzerland: Novartis Pharma AG (Basel) 2001
Shin GP, Johnson N, Vasquez E, et al. Cost-effectiveness of basiliximab, daclizumab, and OKT3 as induction agents in kidney transplantation [abstract]. Value Health 2000 Mar–Apr; 3(2): 140
Light JA, Barhyte DY, Ennis JA, et al. Is using daclizumab (DAC) cost effective in kidney transplantation? [online]. Available from URL: http://www.abstracts-on-line.com/abstracts/TRANS [Accessed 2001 May 21]
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Carswell, C.I., Plosker, G.L. & Wagstaff, A.J. Daclizumab. BioDrugs 15, 745–773 (2001). https://doi.org/10.2165/00063030-200115110-00005
Published:
Issue Date:
DOI: https://doi.org/10.2165/00063030-200115110-00005