Abstract
Objective: In the treatment of epilepsy, as in all areas of drug therapy, generic formulations are becoming more important as pressure to reduce drug costs increases. In clinical practice, the interchangeability of reference and generic preparations is often assumed. However, in individual patients with a narrow therapeutic range, switching to another formulation of an antiepileptic agent with low water solubility and nonlinear pharmacokinetics may lead to breakthrough seizures or toxicity The purpose of this study was to examine the bioequivalence and clinical effects after switch of equal daily dosages of two commercially available sustained-release preparations of carbamazepine (CBZ).
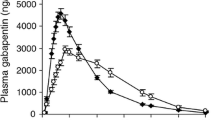
Patients and Study Design: This was a nonblinded intra-individual trial in 14 patients aged 18 to 52 years with focal epilepsy who had been receiving mono-therapy with the reference preparation of sustained-release carbamazepine (mean dosage 1985 mg/day given twice daily) for at least 35 days. After a minimum of 3 further days, the reference preparation (denoted CBZ-R) was immediately replaced by an identical dosage of the generic preparation (denoted CBZ-G). Under steady-state conditions, for each preparation we determined area under the serum concentration-time curve (AUC), maximum serum concentration (Cmax), minimum serum concentration (Cmin) and peak-trough fluctuation (PTF) of carbamazepine and carbamazepine 10,11-epoxide.
Results: One patient dropped out because of intolerable adverse effects with CBZ-G. For carbamazepine, the data for the remaining 13 patients, expressed as CBZ-G/CBZ-R, were: AUC 111.5% [90% confidence interval (CI) 105.6-117.8%]; PTF 90.9% (90% CI 73.4-112.8%); Cmax110.1% (90% CI 100.4-117.0%). These data indicate a higher bioavailability for CBZ-G. For carbamazepine 10,11-epoxide, about 20% higher average concentrations were measured with CBZ-G. Applying the usual inclusion rule [90% CI within the range 80 to 125% (AUC) or 70to 143% (PTF and Cmax) of the reference preparation], the two formulations can be considered as bioequivalent. In contrast, we observed marked adverse effects, such as dizziness, nausea, ataxia, diplopia and nystagmus, in eight of the remaining 13 patients after switching to CBZ-G.
Conclusions: Proof of bioequivalence between reference and generic preparations of antiepileptic drugs does not mean that they are freely interchangeable. Generic formulations with proven bioequivalence to branded preparations can be used, for example, at the beginning of treatment or in poorly controlled patients with serum concentrations in the mid range. The results demonstrate that the usual rules for bioequivalence and the range of acceptability for preparations of carbamazepine are problematic.
Similar content being viewed by others
References
Blume H, Mutschier E. Bioäquivalenz: qualitätsbewertung inhaltsgleicher Fertigarzneimittel. Im: Auftrag der Bundesvereinigung Dt. Apothekerverband ed. Frankfurt: Govi-Verlag, 1996
CPMP (Committee for Proprietary Medicinal Products) Working Party on the Efficacy of Medicinal Products. Notes for guidance: investigation of bioavailability and bioequivalence. The rules governing medicinal products in the European Community 1991; 3: 149–67
Balla J. Dilantin overdosage [letter]. Med J Aust 1968; 2: 480–1
Eadie MJ, Sutherland JM, Tyrer JH. Dilantin overdosage [letter]. Med J Aust 1968; 2: 515
Tyrer JH, Eadie, MJ, Sutherland JM, et al. Outbreak of anticonvulsant intoxication in an Australian city. BMJ 1970; 4: 271–3
Therapeutics and Technology Assessment Subcommittee of the American Academy of Neurology. Assessment: generic substitution for antiepileptic medication. Neurology 1990; 40: 1641–3
Jürgens U. HPLC analysis of antiepileptic drugs in blood samples: microbore separation of fourteen compounds. J Liquid Chromatogr 1987; 10(2,3): 507–32
Holmes GL. Carbamazepine toxicity. In: Levy RH, Mattson RH, editors. Antiepileptic drugs, 4th edition. New York: Raven Press, 1995: 667–72
Busch RL. Generic carbamazepine and erythema multiforme: generic-drug nonequivalence [letter]. N Engl J Med 1989; 316: 692–3
Gashko MA. Generic substitution for antiepileptic drugs [letter]. Neurology 1991; 44: 1165
Glende M, Hüller H, Mai I, et al. Comparative bioavailability of two carbamazepine tablets. Int J Clin Pharmacol Ther Toxicol 1983; 21(12): 631–3
Hartley R, Aleksandowicz J, Ng PC, et al. Breakthrough seizures with generic carbamazepine: a consequence of poorer bioavailability? Br J Clin Pract 1990; 44(7): 270–3
Hartley R, Aleksandowicz J, Bowmer CJ, et al. Dissolution and relative bioavailability of two carbamazepine preparations for children with epilepsy. J Pharm Pharmacol 1991; 43: 117–9
Hirji MR, Measuria H, Kuhn S, et al. A comparative study of the bioavailability of five different phenytoin preparations. J Pharm Pharmacol 1985; 37: 570–2
Jain KK. Investigation and management of loss of efficacy of an antiepileptic medication using carbamazepine as an example. J R Soc Med 1993; 86: 133–6
Jumao-as A, Bella I, Craig B, et al. Comparison of steady-state blood levels of two carbamazepine formulations. Epilepsia 1989; 30: 67–70
Kauko K, Tammistro P. Comparison of two generically equivalent carbamazepine preparations. Ann Clin Res 1974; 6Suppl. 11: 21–5
Meyer MC, Straughn AB, Jarvi EJ, et al. The bioinequivalence of carbamazepine tablets with a history of clinical failures. Pharm Res 1992; 9(12): 1612–6
Neuvonen PJ. Bioavailability and central side effects of different carbamazepine tablets. Int J Clin Pharmacol Ther Toxicol 1985; 23(4): 226–32
Nuwer MR, Browne TR, Dodson WE, et al. Generic substitutions for antiepileptic drugs. Neurology 1990; 40: 1647–51
Oles KS, Penry JK, Smith LD, et al. Therapeutic bioequivalency study of brand name versus generic carbamazepine. Neurology 1992; 42: 1147–53
Sachdeo, RC, Belendiuk G. Generic versus branded carbamazepine [letter]. Lancet 1987: 1: 1432
Silpakit O, Amornpichetkoon M, Kaojarem S. Comparative study of bioavailability and clinical efficacy of carbamazepine in epileptic patients. Ann Pharmacother 1997; 31 548–52
Trimble MR. Generic prescribing. Hum Psychopharmacol 1987; 2: 1–2
Welty TE, Pickering PR, Hale BC, et al. Loss of seizure control associated with generic substitution of carbamazepine. Ann Pharmacother 1992; 26: 775–7
Wolf P, May Th, Tiska G, et al. Steady state concentrations and diurnal fluctuations of carbamazepine in patients after different slow release formulations. Arzneimforschung Drug Res 1992; 42(3): 3–15
Wolf P. Die Generika kommen. Epilepsie-Blätter 1993; 6: 40–2
Wolf P. Die Generika sind da. Epilepsie-Blätter 1996; 9: 16–7
Crawford P, Hall WH, Collings J, et al. Generic prescribing for epilepsy. Is it safe? Seizure 1996; 5(1): 1–5
Beach R, Reading R. Correspondence: generic prescribing for epilepsy. Is it safe? [letter]. Seizure 1997; 6: 327
Richens A. Impact of generic substitution of anticonvulsants in the treatment of epilepsy. CNS Drugs 1997; 8: 124–33
Bialer M, Yacobi A, Moros D, et al. Criteria to assess in vivo performance and bioequivalence of generic controlled-re-lease formulations of carbamazepine. Epilepsia 1998; 39(5): 513–9
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Mayer, T., May, T.W., Altenmüller, D.M. et al. Clinical Problems with Generic Antiepileptic Drugs. Clin. Drug Investig. 18, 17–26 (1999). https://doi.org/10.2165/00044011-199918010-00003
Published:
Issue Date:
DOI: https://doi.org/10.2165/00044011-199918010-00003