Abstract
Complete remission of symptoms and prevention of symptomatic recurrence are among the main therapeutic aims in gastro-oesophageal reflux disease (GORD). In this context, a potent pharmacologic inhibition of gastric acid secretion plays a central role. The goal of antisecretory treatment in GORD is to maintain an intragastric pH greater than 4.0 for the longest possible time. This is best achieved by the administration of proton pump inhibitors (PPIs). Tolerability and safety of different PPIs are similar and consistently high, but therapeutic efficacy may differ among them. Esomeprazole appears to achieve an intragastric pH greater than 4.0 for a larger number of hours compared with any other PPI. This is associated with a greater therapeutic efficacy of esomeprazole compared with omeprazole, lansoprazole and pantoprazole in both complete remission of symptoms and prevention of symptomatic recurrence in GORD. This review provides evidence-based recommendations for the treatment of GORD-related symptoms in clinical practice.
Similar content being viewed by others
1. Introduction
Together with the healing of the lesions constituting oesophagitis, the main objective of treatment in gastro-oesophageal reflux disease (GORD) is to eliminate symptoms and, in the long term, to prevent recurrence. Considering that about 80% of patients who consult their Primary Health Care physician because of GORD and 60% of those referred to the gastroenterologist do not exhibit evidence of oesophagitis on endoscopy (non-erosive or endoscopically negative GORD), the obvious conclusion is that the main therapeutic aim in this disease is remission of symptoms.
GORD manifests typically through the presence of heartburn or acid regurgitation, or both. The presence of these symptoms is more frequent during postprandial periods; nocturnal symptoms — which may even wake the patient — are usually associated with more severe GORD. Atypically, GORD may manifest with other oesophageal symptoms (chest pain, dysphagia) or even extra-oesophageal ones (chronic cough, hoarseness and bronchial asthma, among others), which should be borne in mind in the adequate management of the disease. These atypical symptoms tend to show a less evident response to antisecretory treatment than the typical symptoms, and tend to require longer periods of treatment for achieving that response.
Even though the origin of symptoms in GORD remains uncertain and is probably multifactorial, there is no doubt that the acidic pH of the refluxed material and the enzymatic activity of pepsin are relevant. This assertion is supported, among other facts and factors, by the evident symptomatic response to therapeutic inhibition of gastric acid secretion. For this reason, at present, adequate suppression of acid constitutes the treatment of choice in GORD, in spite of the fact that this therapeutic intervention does not interfere in the pathophysiological mechanisms that favour gastro-oesophageal reflux.
2. Relationship Between pH, Inhibition of Acid Secretion and Symptomatic Response
The objective of antisecretory treatment in GORD is to maintain an intragastric pH greater than 4.0 for the greatest possible number of hours during the day. The rationale of this objective is that the enzymatic activity of pepsin requires an acidic environment, and the enzyme is inactivated when the environmental pH is greater than 4.0. The linear correlation between the number of hours during which the intragastric pH remains greater than 4.0 and the probability that the oesophagitis will heal is already established,[1] and a number of meta-analyses have demonstrated that the proportion of patients with oesophagitis whose lesions heal is directly related to the degree and duration of acid suppression.[1,2] Equally relevant from the clinical point of view, and most especially for the patient, is the rapidity of healing, which may be expressed as the proportion of patients healed per given unit of time. Both concepts — proportion of patients healed and rapidity of healing — are equally applicable to the symptomatic response. The choice of the drug to be used, the daily dose of that drug and its mode and timing of administration are essential instruments in optimising the results of treatment.[1,3]
A number of drugs have been used in the management of GORD, with the initial aim of achieving remission of symptoms (acute treatment) and with the long-term aim of preventing the recurrence of symptoms (maintenance treatment). Among these drugs are the antacids and alginates, which act by neutralising gastric acidity, the histamine2 (H2) receptor antagonists and the proton pump inhibitors (PPIs), which induce a more or less potent inhibition of gastric acid secretion, and finally the prokinetics, which attempt to improve the oesophageal clearance of the refluxed material and to increase the lower oesophageal sphincter pressure, besides indirectly limiting gastro-oesophageal reflux by accelerating gastric emptying.
3. Acute Treatment of GORD: Achievement of a Symptomatic Response
The aim of the initial treatment of a patient with GORD is to achieve remission of the symptoms in the shortest possible time. This holds true regardless of the type of symptom or symptoms — typical or atypical — and of the presence (Los Angeles Classification of oesophagitis grade A–D) or absence (non-erosive GORD) of endoscopic lesions. There is no correlation between the severity of symptoms and the presence and grade of endoscopic lesion, and highly symptomatic patients may have mild or even absent endoscopic lesions. Conversely, the various clinical trials published in this field have been carried out both in patients with oesophagitis, in those who gave negative results on endoscopy, and even in patients for whom there was no knowledge of the degree of endoscopic lesion (empiric treatment). Bearing this in mind, in the present paper we will not make any differentiation between patients with or without oesophagitis when describing the symptomatic responses to drug treatments. However, different responses are to be expected in the resolution of atypical symptoms, as discussed in detail in the accompanying paper (by Rodríguez-Téllez) on extra-oesophageal manifestations of GORD.
3.1 Antacids and Alginates
Even though antacids and alginates remain frequently used drugs, scientific evidence concerning their effects on the symptoms of GORD is rather limited. Their therapeutic superiority compared with placebo is restricted to the point control of mild symptoms.[4,5] Furthermore, the effect of antacids and alginates on intragastric pH is of very short duration, as the decrease in gastric acidity induces a stimulation of gastric acid secretion mediated by gastrin (rebound effect). At present, therefore, the use of these drugs in the therapeutic management of GORD cannot be considered adequate.
3.2 Prokinetics
The only prokinetic agents to have been assessed in the management of GORD in randomised, double-blind, placebo-controlled clinical trials are cisapride and metoclopramide.[6,7] The effect of cisapride is superior to that of placebo and probably similar to that of H2 receptor antagonists, without a clear dose–response relationship. Because of important cardiovascular side effects, the use of cisapride is at present restricted to severe gastrointestinal motor disturbances, so that it has no role in the management of GORD.
3.3 Inhibition of Gastric Acid Secretion: H2 Receptor Antagonists vs PPIs
For some years, there was heated discussion as to whether it was better to initiate treatment of GORD with a less potent drug and subsequently escalate treatment according to the clinical response (up-scaling protocol) or, conversely, to begin treatment with the most potent drug and then scale down to other less potent ones (down-scaling protocol). On the basis of the available scientific evidence, the initial treatment of GORD is at present aimed at potent inhibition of gastric acid secretion. This treatment seeks to achieve complete remission of symptoms in the shortest possible time. In this context, many publications have consistently reported the superiority of PPIs over the H2 receptor antagonists. Most of these studies formed a part of the — already classical — meta-analysis by Chiba et al.,[8] which demonstrated a significantly superior efficacy of the PPIs over the H2 receptor antagonists, both in the proportion of patients free of symptoms (77.4 ± 10.4% and 47.6 ± 15.5%, respectively) and in the rapidity with which this complete clinical response was achieved (11.5% per week and 6.4% per week, respectively). This superiority of the PPIs over the H2 receptor antagonists in the control of GORD-associated symptoms has been confirmed both in patients with oesophagitis and in those with endoscopically negative GORD, and even in empiric treatment — confirmation of which was well presented in a recently published systematic review.[9] This improvement in symptoms during PPI treatment is associated with an improvement in measures of quality of life, which has been confirmed in a prospective cohort study (ProGERD initiative) in more than 6000 patients.[10] The greater efficacy of PPIs over H2 receptor antagonists also translates into better cost-efficacy.[8,11,12] As compared with the H2 receptor antagonists, besides greater antisecretory potency, the PPIs demonstrate a longer-lasting effect and absence of tolerance phenomena, which constitute additional advantages in long-term treatment, as discussed later. On the basis of those advantages of PPIs, H2 receptor antagonists nowadays have no therapeutic role in the management of GORD.
3.4 Differences Between the Various PPIs
The marked superiority of the PPIs over the H2 receptor antagonists reflects the importance of potent acid inhibition in the relief of symptoms in patients with GORD. In this context, metabolic differences between the various PPIs might lead to their exhibiting different efficacies. Such aspects as cost and potential pharmacological interactions may be important in the selection of the drug to be used, but only if the clinical efficacy of the various PPIs in the therapeutic management of the GORD is the same. A recent meta-analysis of randomised, controlled and comparative clinical trials of two or more PPIs in the acute treatment of GORD demonstrated that the differences between them depend more on the dose used than on the specific PPI chosen:[13] greater doses achieved greater efficacy, again confirming the importance of potent acid inhibition in the treatment of GORD. That same meta-analysis did not reveal any differences in tolerability and safety between the various PPIs.[13]
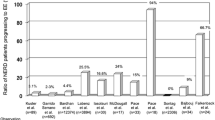
Recent randomised, controlled and comparative clinical trials comparing esomeprazole with the other PPIs (omeprazole, lansoprazole, pantoprazole and rabeprazole) demonstrated greater efficacy of esomeprazole in the control of gastric acid secretion in terms of the number of hours during which the intragastric pH remained greater than 4.0.[14–17] As potent acid inhibition is an absolute requirement for an optimal therapeutic effect, and in view of the direct correlation between the period of time during which the intragastric pH remains greater than 4.0 and the rapidity and efficacy of the antisecretory treatment, esomeprazole would be expected to exhibit a greater efficacy over the other PPIs in the therapeutic management of GORD, and this superiority has indeed been confirmed in randomised, double-blind, controlled and comparative clinical trials of esomeprazole and omeprazole,[18] lansoprazole[19] and pantoprazole.[20] However, the findings of recently published comparative studies of esomeprazole and pantoprazole, both at a dose of 40 mg/day, suggest equivalence of the two drugs in the treatment of the symptoms of GORD.[21,22] Unlike the EXPO trial,[20] which included more than 3000 patients with GORD, the last two studies, both carried out by the same group of authors, involved only slightly more than 200 patients, so that their statistical power to demonstrate equivalence is debatable. A systematic review of the literature demonstrates that esomeprazole is the only PPI that is more effective than omeprazole in the acute treatment of GORD, after both 4 and 8 weeks of treatment.[23]
The greatest difference between esomeprazole and the other PPIs becomes evident in those patients who require particularly potent inhibition of gastric acid secretion. This situation occurs in patients who are Helicobacter pylori negative and in those with severe GORD. The PPIs are less effective in patients who are not infected by H. pylori. However, esomeprazole has demonstrated evidence of high efficacy regardless of the presence or absence of H. pylori.[20] In this context, the difference in efficacy between esomeprazole and the other PPIs increases in favour of the former in patients not infected by H. pylori.[24]
Up to 30% of patients with GORD who are treated with single daily doses of a PPI continue to experience heartburn at some time during the day or the night. These patients usually respond to the administration of the PPI in two daily doses (before breakfast and before dinner), which achieves a significant prolongation of the period during which the intragastric pH remains greater than 4.0.[25–27] In these cases, if the patient was receiving treatment with a PPI other than esomeprazole, switching from that PPI to a single daily dose of esomeprazole 40mg could be as effective as doubling the dose of the original PPI,[28] although this requires confirmation in further, more appropriately designed, trials. In fact, and contrary to the other PPIs, esomeprazole given in a single dose before breakfast has been shown to be effective in preventing the occurrence of night-time heartburn and in improving the quality of sleep.[29] Nevertheless, a recent large trial in non-erosive reflux disease failed to show a superiority of esomeprazole in the control of symptoms.[30]
In summary, potent acid inhibition is necessary in the therapeutic management of GORD-associated symptoms, in order to achieve rapid and effective remission of symptoms. This assertion is supported by the following evidence (degrees of evidence and recommendation are rated according to the criteria established in the introduction of this Supplement):
-
PPIs are significantly more effective than H2 receptor antagonists in achieving remission of symptoms in patients with GORD (level of evidence 1 a).
-
The greater efficacy of the PPIs in achieving remission of the symptoms of GORD holds both for patients with oesophagitis and for those with non-erosive GORD, and in the empirical treatment of patients without upper digestive tract endoscopy (level of evidence 1 a).
-
With the exception of esomeprazole, all other PPIs show similar efficacy in healing oesophagitis when used at equivalent dosage (level of evidence 1 b).
-
Esomeprazole renders it possible to achieve a more protracted inhibition of gastric acid secretion than do the other PPIs at equivalent dosages (level of evidence 1 a).
-
Esomeprazole demonstrates evidence of greater efficacy than omeprazole, lansoprazole and pantoprazole in the management of the symptoms of GORD (level of evidence 1 a).
-
The efficacy of esomeprazole in the treatment of GORD is independent of the presence or absence of H. pylori infection (level of evidence 1 b).
3.5 Recommendations
-
PPIs are the drugs of first choice in the acute symptomatic treatment of patients with GORD (degree of recommendation A).
-
The administration of full doses of the chosen PPI in a single daily dose before breakfast is the most efficient method of acute symptomatic treatment in patients with GORD (degree of recommendation A).
4. Maintenance Treatment of GORD for Preventing the Recurrence of Symptoms
Withdrawal of antisecretory treatment after clinical remission has been achieved with the above acute treatment leads to the recurrence of GORD in a majority of cases. For this reason, most patients with GORD will require some form of maintenance treatment.
As in acute therapy, potent acid inhibition is also required in maintenance of the remission of symptoms in patients with GORD, both in those with previous oesophagitis and in those with endoscopically negative GORD. Thus neither antacids nor alginates will have any role in the maintenance treatment of GORD, and their use will remain restricted to point control of episodes of heartburn in individuals not diagnosed with GORD. In fact, no single randomised, controlled clinical trial has been published on the usefulness of antacids in the maintenance treatment in GORD. Neither is the use of prokinetics effective in this context. In the latter case, five randomised and controlled clinical trials of cisapride and placebo have been published, involving a cumulative total of almost 1400 patients. Four of these trials revealed no superiority of cisapride over placebo in the maintenance of remission in GORD; only one trial[31] showed better results with cisapride, with remission of symptoms in 66% of patients after 1 year of treatment with cisapride, compared with remission in 49% of those receiving placebo.
The efficacy of the H2 receptor antagonists in the maintenance treatment of GORD is questionable. The findings of only one small clinical trial (69 patients) have been published, which did not demonstrate superiority of the active drug over placebo. There are also no comparative studies available comparing H2 receptor antagonists with antacids or prokinetic drugs. In contrast, it is well known that maintenance treatment with H2 receptor antagonists is significantly less effective than maintenance treatment with PPIs.[32]
In contrast to the H2 receptor antagonists, the PPIs have an efficacy in the maintenance treatment of GORD that has been amply demonstrated. To take the symptomatic response, the PPIs are significantly superior to placebo in preventing recurrence, as confirmed in 12 randomised, controlled clinical trials including a total of 3000 patients; most of these trials have been assessed in a systematic review.[33] Six clinical trials including some 1000 patients and assessed in the review[33] have demonstrated the significant superiority of the PPIs over the H2 receptor antagonists in the prevention of recurrence of symptoms in patients with GORD. The already classical study by Vigneri et al.[34] demonstrated a superiority of PPIs over all other treatments used in GORD, be they H2 receptor antagonists, prokinetics or even a combination of both, in preventing recurrence of the disease.
All the above data and arguments confirm the need for potent acid inhibition in the prevention of the recurrence of symptoms in patients with GORD. This inhibition must, beyond question, be carried out with a PPI, the dosage of which must be carefully individualised. It is a standard procedure in maintenance treatment to prescribe a PPI at one-half the dose used for achieving the remission of symptoms. This approach is appropriate for about 80% of patients. However, in the remaining 20%, reducing the dose of the PPI is associated with a greater risk of recurrence, mainly in those with severe GORD.[32] A more profound inhibition of gastric acid secretion guarantees a lower rate of recurrence in this disease.
The particular antisecretory potency of esomeprazole may constitute the exception to the above statement. In fact, the rate of recurrence in patients treated with esomeprazole is very low, regardless of whether the daily maintenance dose is 20mg or 40mg, and regardless of the severity of the disease.[35] On the basis of the findings of that study, maintenance treatment in severe GORD should be carried out with full doses of a PPI, esomeprazole being the first choice when the use of half-doses is preferred. This has been confirmed in a randomised, double-blind comparative clinical trial of esomeprazole and lansoprazole, both administered at one-half the standard dose (20mg and 15mg, respectively).[36] In this study of more than 1000 patients over a period of 6 months, the overall rate of endoscopically demonstrated recurrence was 9% lower with esomeprazole than with lansoprazole — a highly significant difference, both statistically and clinically, considering the high efficacy of this group of drugs. This difference increased to 17% in a subanalysis of patients with severe GORD.[35] Similar differences were observed in analysis of the recurrence of symptoms.
A similar randomised, comparative study of more than 2700 patients who were treated for 6 months with esomeprazole 20mg or pantoprazole 20mg after healing of their oesophagitis lesions had been achieved showed greater efficacy of the former than of the latter in the prevention of endoscopically demonstrated recurrence (87% of those receiving esomeprazole remained in remission, compared with 75% of those treated with pantoprazole; p < 0.001).[37] In that same study, the remission of symptoms was achieved in 94% of the patients treated with esomeprazole 20 mg/day and in 87% of those receiving pantoprazole 20 mg/day (p < 0.001).[37]
On the basis of our critical review of the literature on the effects of the various PPIs in the maintenance treatment of GORD, the conclusion can be drawn that any PPI at full dosage is more effective than the same PPI at half dosage. In addition, among the various PPIs used at half dosage, esomeprazole is the only one to have proved more effective than lansoprazole or pantoprazole.
4.1 On-Demand Maintenance Treatment
In patients with endoscopically negative GORD and with less frequent symptoms, on-demand maintenance treatment may be cost-effective, and is well accepted by most. In fact, in the long term, a considerable proportion of patients voluntarily abandon daily maintenance treatment and turn instead to on-demand treatment based on the appearance of symptoms.[38] The particular drug to be used in on-demand treatment should induce potent inhibition of gastric acid secretion, should have a rapid onset of action, should have a long-lasting effect and should have a predictable inter-individual response. All these criteria may be fulfilled by esomeprazole. In two randomised, double-blind, placebo-controlled clinical trials, esomeprazole (both 20mg and 40mg) has been shown to be effective in the on-demand maintenance treatment of non-erosive GORD.[39,40] In these two trials, more than 90% of patients achieved adequate control with on-demand esomeprazole, requiring a mean of one tablet every 3 days. This was associated with a reduction in direct costs of up to 61% as compared with once-daily maintenance treatment with a PPI.[41] More recently, on-demand esomeprazole has been shown to be significantly more frequently preferred than daily lansoprazole as maintenance treatment of non-erosive reflux disease (93% compared with 88% after 6 months, respectively; p = 0.02).[42] In addition, direct costs of maintenance treatment are 36% lower with on-demand esomeprazole than with daily lansoprazole.[42]
In summary, potent acid inhibition is required in the maintenance of the remission of symptoms in patients with GORD. This assertion is supported by the following evidence:
-
PPIs are significantly more effective in the maintenance of the remission of symptoms in patients with GORD than are H2 receptor antagonists (level of evidence 1 a).
-
The greater efficacy of PPIs in the maintenance of the remission of symptoms in GORD is independent of the endoscopically demonstrated severity of the condition — that is, it is evident both in patients with previous oesophagitis and in those with previous non-erosive GORD (level of evidence 1 a).
-
The efficacy of the various PPIs in the maintenance treatment of GORD is greater when full doses are used than when only half-doses are given (level of evidence 1 a).
-
When half-doses are given, esomeprazole has been shown to be superior to lansoprazole and pantoprazole (level of evidence 1 a).
-
Esomeprazole is highly effective in on-demand maintenance treatment in patients with non-erosive GORD (level of evidence 1 a).
4.2 Recommendations
-
PPIs are the drugs of first choice in maintenance treatment for preventing the recurrence of symptoms in patients with GORD (degree of recommendation A).
-
When a PPI is to be used at one-half the standard dose in the maintenance treatment of GORD, esomeprazole has been shown to be more adequate than lansoprazole and pantoprazole (degree of recommendation A).
-
Esomeprazole is an adequate drug for on-demand maintenance treatment in GORD. Patients without previous oesophagitis and with less frequent symptoms are those who will most benefit from this treatment modality (degree of recommendation A).
References
Bell NJ, Burget D, Howden CW, et al. Appropriate acid suppression for the management of gastro-esophageal reflux disease. Digestion 1992; 51 Suppl 1: 59–67
Bell NJV. Hunt RH. Role of gastric acid suppression in the treatment of gastro-esophageal reflux disease. Gut 1992; 33: 118–24
Hunt RH. Importance of pH control in the management of GERD. Arch Intern Med 1999; 159: 649–57
Graham DY, Patterson DJ. Double-blind comparison of liquid antacid and placebo in the treatment of symptomatic reflux esophagitis. Dig Dis Sci 1983; 28: 559–63
Chatfield S. Comparison of the efficacy of the alginate preparation, Gaviscon Advance, with placebo in the treatment of gastro-esophageal reflux disease. Curr Med Res Opin 1999; 15: 152–9
Richter JE, Long JF. Cisapride for gastroesophageal reflux disease: a placebo-controlled, double-blind study. Am J Gastroenterol 1995; 90: 423–30
McCallum RW, Fink SM, Winnan GR, et al. Metoclopramide in gastroesophageal reflux disease: rationale for its use and results of a double-blind trial. Am J Gastroenterol 1984; 79: 165–72
Chiba N, De Gara CJ, Wilkinson JM, et al. Speed of healing and symptom relief in grade II to IV gastroesophageal reflux disease: a meta-analysis. Gastroenterology 1997; 112: 1798–810
van Pinxteren B, Numans ME, Lau J, et al. Short-term treatment of gastroesophageal reflux disease: a systematic review and meta-analysis of the effect of acid-suppressant drugs in empirical treatment and in endoscopy-negative patients. J Gen Intern Med 2003; 18: 755–63
Kulig M, Leodolter A, Vieth M, et al. Quality of life in relation to symptoms in patients with gastro-esophageal reflux disease — an analysis based on the ProGERD initiative. Aliment Pharmacol Ther 2003; 18: 767–76
Stalhammar NO, Carlsson J, Peacock R, et al. Cost effectiveness of omeprazole and ranitidine in intermittent treatment of symptomatic gastro-esophageal reflux dis-ease. Pharmacoeconomics 1999; 16: 483–97
Bardhan KD, Muller-Lissner S, Bigard MA, et al. Symptomatic gastro-esophageal reflux disease: double blind controlled study of intermittent treatment with omeprazole or ranitidine. The European Study Group. BMJ 1999; 318: 502–7
Klok RM, Postma MJ, van Hout BA, et al. Meta-analysis: comparing the efficacy of proton pump inhibitors in short-term use. Aliment Pharmacol Ther 2003; 17: 1237–45
Rohss K, Hasselgren G, Hedenstrom H. Effect of esomeprazole 40 mg vs omeprazole 40 mg on 24-hour intragastric pH in patients with symptoms of gastroesophageal reflux disease. Dig Dis Sci 2002; 47: 954–8
Lind T, Rydberg L, Kyleback A, et al. Esomeprazole provides improved acid control vs. omeprazole in patients with symptoms of gastro-esophageal reflux disease. Aliment Pharmacol Ther 2000; 14: 861–7
Miner P Jr, Katz PO, Chen Y, et al. Gastric acid control with esomeprazole, lansoprazole, omeprazole, pantoprazole, and rabeprazole: a five-way crossover study. Am J Gastroenterol 2003; 98: 2616–20
Wilder-Smith CH, Rohss K, Nilsson-Pieschl C, et al. Esomeprazole 40 mg provides improved intragastric acid control as compared with lansoprazole 30 mg and rabeprazole 20 mg in healthy volunteers. Digestion 2003; 68: 184–8
Richter JE, Kahrilas PJ, Johanson J, et al. Esomeprazole Study Investigators. Efficacy and safety of esomeprazole compared with omeprazole in GERD patients with erosive esophagitis: a randomized controlled trial. Am J Gastroenterol 2001; 96: 656–65
Castell DO, Kahrilas PJ, Richter JE, et al. Esomeprazole (40 mg) compared with lansoprazole (30 mg) in the treatment of erosive esophagitis. Am J Gastroenterol 2002; 97: 575–83
Labenz J, Armstrong D, Lauritsen K, Katelaris P, Schmidt S, Schutze K, et al. A randomized comparative study of esomeprazole 40 mg versus pantoprazole 40 mg for healing erosive oesophagitis: the EXPO study. Aliment Pharmacol Ther 2005; 21: 739–46
Scholten T, Gatz G, Hole U. Once-daily pantoprazole 40mg and esomeprazol 40mg have equivalent overall efficacy in relieving GERD-related symptoms. Aliment Pharmacol Ther 2003; 18: 587–94
Gillesen A, Beil W, Modlin IM, et al. 40 mg pantoprazole and 40 mg esomeprazole are equivalent in the healing of esophageal lesions and relief from gastroesophageal reflux disease-related symptoms. J Clin Gastroenterol 2004; 38: 332–40
Edwards SJ, Lind T, Lundell L. Systematic review of proton pump inhibitors for the acute treatment of reflux esophagitis. Aliment Pharmacol Ther 2001; 15: 1729–36
Labenz J, Nauclér E, Keeling N, et al. Esomeprazol 40 mg heals significantly more Helicobacter pylori-negative erosive esophagitis patients than pantoprazole 40 mg. Gastroenterology 2004; 126: A–338
Pehlivanov ND, Olyaee M, Sarosiek I, et al. Comparison of morning and evening administration of rabeprazole for gastro-esophageal reflux and nocturnal gastric acid break through in patients with reflux disease: adouble-blind, crossover study. Aliment Pharmacol Ther 2003; 18: 883–90
Hatlebakk JG, Katz PO, Kuo B, et al. Nocturnal gastric acidity and acid breakthrough on different regimens of omeprazole 40 mg daily. Aliment Pharmacol Ther 1998; 12: 1235–40
Katz PO, Hatlebakk JG, Castell DO. Gastric acidity and acid breakthrough with twice-daily omeprazole or lansoprazole. Aliment Pharmacol Ther 2000; 14: 709–14
Fass R, Thomas S, Traxler B, et al. Patient-reported outcome of heartburn improvement: doubling the proton pump inhibitor dose in patients who failed standard dose PPI versus switching to a different proton pump inhibitor. Gastroenterology 2004; 126: A–37
Johnson D, Orr W, Cuccia A, et al. Esomeprazole for the relief of moderate to severe nighttime heartburn and associated sleep disturbance in patients with GERD: a multicentre, randomized, double-blind, placebo-controlled, 4-week study. Gastroenterology 2004; 126: A–336
Armstrong D, Talley NJ, Lauritsen K, et al. The role of acid suppression in patients with endoscopy-negative reflux disease: the effect of treatment with esomeprazole or omeprazole. Aliment Pharmacol Ther 2004; 20: 413–21
Blum AL, Adami B, Bouzo MH, et al. Effect of cisapride on relapse of esophagitis: a multinational, placebo-controlled trial in patients healed with an antisecretory drug. The Italian Eurocis Trialists. Dig Dis Sci 1993; 38: 551–60
Hetzel DJ, Dent J, Reed WD, et al. Healing and relapse of severe peptic esophagitis after treatment with omeprazole. Gastroenterology 1988; 95: 903–12
Caro JJ, Salas M, Ward A. Healing and relapse rate in gastroesophageal reflux disease treated with the newer proton pump inhibitors lansoprazole, rabeprazole and pantoprazole compared with omeprazole, ranitidine and placebo; evidence from randomised clinical trials. Clin Ther 2001; 23: 998–1017
Vigneri S, Termini R, Leandro G, et al. A comparison of five maintenance therapies for reflux esophagitis. N Engl J Med 1995; 333: 1106–10
Vakil NB, Shaker R, Johnson DA, et al. The new proton pump inhibitor esomeprazole is effective as a maintenance therapy in GERD patients with healed erosive esophagitis: a 6-month, randomized, double-blind, placebo-controlled study of efficacy and safety. Aliment Pharmacol Ther 2001; 15: 927–35
Lauritsen K, Deviere J, Bigard MA, et al. Esomeprazole 20 mg and lansoprazole 15 mg in maintaining healed reflux esophagitis: Metropole Study results. Aliment Pharmacol Ther 2003; 17: 333–41
Labenz J, Armstrong D, Katelaris PH, et al. A comparison of esomeprazole and pantoprazole for maintenance treatment of healed erosive esophagitis. Gut 2004; 53 Suppl VI: A108
Schindlbeck NE, Klauser AG, Berghammer G, et al. Three year follow up of patients with gastroesophageal reflux disease. Gut 1992; 33: 1016–9
Talley NJ, Lauritsen K, Tunturi-Hihnala H, et al. Esomeprazole 20 mg maintains symptom control in endoscopy-negative gastro-esophageal reflux disease: a controlled trial of ‘on-demand’ therapy for 6 months. Aliment Pharmacol Ther 2001; 15: 347–54
Talley NJ, Venables TL, Green JR, et al. Esomeprazole 40 mg and 20 mg is efficacious in the long-term management of patients with endoscopy-negative gastro-esophageal reflux disease: a placebo-controlled trial of on-demand therapy for 6 months. Eur J Gastroenterol Hepatol 2002; 14: 857–63
Wahlqvist P, Junghard O, Higgins A, et al. Cost-effectiveness of proton pump inhibitors in gastroesophageal reflux disease without esophagitis: comparison of on-demand esomeprazole with conventional omeprazole strategies. Pharmacoeconomics 2002; 20: 267–77
Tsai HH, Chapman R, Shepherd A, et al. Esomeprazole 20 mg on-demand is more acceptable to patients than continuous lansoprazole 15 mg in the long-term maintenance of endoscopy-negative gastro-oesophageal reflux patients: the COMMAND Study. Aliment Pharmacol Ther 2004; 20: 657–65
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Domínguez-Muñoz, J.E., Sobrino, M. Clinical Response (Remission of Symptoms) in Erosive and Non-Erosive Gastro-Oesophageal Reflux Disease. Drugs 65 (Suppl 1), 43–50 (2005). https://doi.org/10.2165/00003495-200565001-00007
Published:
Issue Date:
DOI: https://doi.org/10.2165/00003495-200565001-00007