Summary
Abstract
Rapacuronium bromide (rapacuronium) is an aminosteroid, nondepolarising neuromuscular blocking agent (NMBA). At the recommended dose for endotracheal intubation (1.5 mg/kg), an intravenous bolus of rapacuronium has a rapid onset (≈1.2 to 1.8 minutes) and short duration of action (10.2 to 16.5 minutes) in adults undergoing elective surgery. Rapacuronium 1.5 mg/kg produced clinically acceptable intubating conditions in 68 to 89% of these patients at about 1 minute after administration. The onset, extent and duration of action and clinical efficacy of an intubating dose of rapacuronium appeared to be similar in the general adult population, adult patients with renal or hepatic dysfunction, patients undergoing Caesarean section, and elderly, paediatric or obese adult patients.
Onset time with rapacuronium 1.3 to 2.5 mg/kg (0.9 to 1.8 minutes) was similar to or slower than that with a 1 mg/kg dose of the depolarising NMBA suxamethonium chloride (0.8 to 1.2 minutes). Intubating conditions were clinically acceptable about 1 minute after administration in 86 to 100% of patients with rapacuronium 1.3 to 2.5 mg/kg compared with in 88 to 97% of patients with suxamethonium chloride 1 or 1.5 mg/kg. Spontaneous recovery was slower with rapacuronium than with suxamethonium chloride, but neostigmine 0.04 or 0.05 mg/kg administered 2 or 5 minutes after rapacuronium 1.3 or 1.5 mg/kg acceler-ated recovery.
In the few available comparative clinical trials, rapacuronium 1.5 mg/kg appeared to have a more rapid onset of action than the nondepolarising NMBAs mivacurium chloride 0.25 mg/kg, rocuronium bromide 0.45 or 0.6 mg/kg or vecuronium bromide 0.07 mg/kg, and a shorter duration of action than rocuronium bromide 0.45 or 0.6 mg/kg or vecuronium bromide 0.07 mg/kg.
Additional boluses (≤3) of rapacuronium 0.5 or 0.55 mg/kg after an intubating bolus of 1.5 mg/kg provided continued skeletal muscle relaxation during short surgical procedures in adult patients. However, these patients may recover more slowly than those who receive a single bolus of the drug.
Bronchospasm was the most common treatment-related adverse event with rapacuronium 0.3 to 3 mg/kg (3.4% of adult patients). Tachycardia, injection site reaction and hypotension were also reported in small proportions of patients (1.6, 1.1 and 0.9%). The overall incidence of drug-related adverse events was similar with rapacuronium 1.5 or 2.5 mg/kg or suxamethonium chloride 1 mg/kg (8 vs 6%) but bronchospasm, tachycardia and injection site reaction tended to occur more often with rapacuronium.
Conclusions: At the recommended dose of 1.5 mg/kg, the nondepolarising NMB A rapacuronium has a rapid onset and short duration of action. It may provide a nondepolarising alternative to suxamethonium chloride for endotracheal intubation. Rapacuronium may be preferred over rocuronium bromide, vecuronium bromide or mivacurium chloride in this indication.
Pharmacodynamic Properties
Neuromuscular block. At the dose recommended for endotracheal intubation (1.5 mg/kg), rapacuronium bromide (rapacuronium) administered as a single intravenous bolus dose has a rapid onset of action. Onset time (time to maximum twitch suppression) is ≈1.2 to 1.8 minutes with rapacuronium 1.5 mg/kg and is inversely correlated with doses in the range 0.3 to 2.5 mg/kg. With rapacuronium 2.5 mg/kg, onset time is ≈1 or 1.3 minutes.
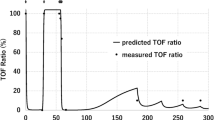
The duration of action is short with rapacuronium 1.5 mg/kg but intermediate with rapacuronium 2.5 mg/kg. Clinical duration (time to recovery of twitch response to 25% of baseline) is 10.2 to 16.5 minutes with the 1.5 mg/kg dose versus 18.6 to 25.4 minutes with the 2.5 mg/kg dose. Recovery from neuromuscular block is accelerated about 40 to 50% by administration of an anticholinesterase agent (usually neostigmine 0.04 to 0.07 mg/kg) 2 or 5 minutes after a bolus dose of rapacuronium 1.5 mg/kg in adult patients.
The onset and extent of action of rapacuronium was similar in adult (aged 18 to 64 years) and elderly patients (aged 65 to 85 years) and appeared to be similar in healthy adults and in adult patients with renal or hepatic dysfunction. Spontaneous recovery may be slower in elderly patients and more rapid in adult patients with hepatic dysfunction than in other adult patients, but the difference was not significant or statistics were not reported. There was no significant difference in duration of recovery between patients with and without renal dysfunction, but data are limited. The onset and duration of action of rapacuronium in paediatric patients (aged ≤13 years) appeared to be within the ranges observed in adults.
The onset of action (based on onset time) appeared to be more rapid with rapacuronium 1.5 mg/kg than with rocuronium bromide 0.45 or 0.6 mg/kg, vecuronium bromide 0.07 mg/kg or mivacurium chloride 0.25 mg/kg in the few available comparative trials, but was similar to or slower than that of the fast-acting depolarising NMBA suxamethonium chloride 1 mg/kg. Onset time was 0.9 to 1.8 minutes with rapacuronium 1.3 to 2.5 mg/kg versus 0.8 to 1.2 minutes with suxamethonium chloride 1 mg/kg. Twitch suppression at 1 minute varied, but did not differ significantly between rapacuronium (70 to 93%) and suxamethonium chloride (80 or 95%).
Duration of action (based on clinical duration) with rapacuronium 1.5 mg/kg tended to be shorter than that with rocuronium bromide 0.45 or 0.6 mg/kg or vecuronium bromide 0.07 mg/kg but did not differ significantly from that with mivacurium chloride 0.25 mg/kg. However, clinical duration was similar with the 2.5 mg/kg dose of rapacuronium and with mivacurium chloride 0.25 mg/kg or rocuronium bromide 0.45 mg/kg. Clinical duration was longer with rapacuronium 1.5 mg/kg or 2.5 mg/kg than with suxamethonium chloride 1 or 1.5 mg/kg. The duration of recovery from neuromuscular block induced with rapacuronium 1.3 or 1.5 mg/kg and accelerated by an anticholinesterase agent relative to that with suxamethonium chloride 1 mg/kg alone varied in different clinical trials.
Neuromuscular block induced with a single bolus of rapacuronium 1.5 mg/kg can be maintained (twitch response ≤25% of baseline) with ≤3 additional boluses of rapacuronium 0.5 or 0.55 mg/kg. The duration of neuromuscular block can increase with each successive maintenance bolus of rapacuronium 0.5 or 0.55 mg/kg, suggesting that accumulation of the drug may occur.
Other Effects. Plasma histamine levels did not increase in the 5 minutes after administration of a single bolus of rapacuronium 1 mg/kg but increased transiently after a 2 or 3 mg/kg dose. Similar to other NMBAs, rapacuronium tended to decrease blood pressure (by 0 to 30% from baseline) and increase heart rate (by 10 to 24% from baseline) in the first few minutes after administration; these changes generally resolved within 15 minutes. These effects of rapacuronium were not correlated with plasma histamine levels in a dose-ranging trial.
Heart rate increased more in patients who received rapacuronium than in those who received suxamethonium chloride and the difference was significant in 2 of 3 trials. The extent of the decrease in blood pressure with rapacuronium was similar to that with mivacurium chloride or vecuronium bromide and was variable relative to that with suxamethonium chloride.
Pharmacokinetic Properties
Data collected in studies of the pharmacokinetic properties of rapacuronium were analysed by traditional or population approaches, and were analysed using 2- or 3-compartmental models in different trials. After administration of a single intravenous bolus of 0.5 to 2.5 mg/kg or a short infusion of 1 mg/kg of rapacuronium, the plasma concentration declined rapidly over time. The apparent volume of distribution at steady state (Vss) was 0.316 to 0.457 L/kg with a single bolus of rapacuronium 1.5 mg/kg. The first-order rate constant (ke0) for equilibration of the drug between the central compartment (plasma) and the effect compartment (neuromuscular junction) was 0.38 to 0.42 per minute, and tended to be higher than that reported for rocuronium bromide or vecuronium bromide. This suggests that rapacuronium reaches the neuromuscular junction more rapidly than these other nondepolarising NMBAs, consistent with its more rapid onset of action.
The major metabolite of rapacuronium, ORG-9488, is formed by hydrolysis at the 3-position of the steroid nucleus. The plasma concentration of this metabolite is approximately 10% of that of the parent drug shortly after administration of a bolus of rapacuronium 1.1 mg/kg.
Clearance of rapacuronium from plasma is rapid (0.422 to 0.666 L/h/kg) and clearance from blood is not consistently related to age or haemoglobin level. Plasma clearance of ORG-9488 is markedly slower than that of the parent drug (0.077 or 0.066 vs 0.437 L/h/kg). Although plasma clearance of rapacuronium was slower in patients with renal dysfunction than in those with normal renal function, the fraction of the administered dose recovered in urine from patients with normal renal function as parent compound and metabolites was low (6.2 to 22%). It was suggested that excretion of the drug is both renal and hepatic. The terminal elimination half-life was approximately 1 to 3 hours and was not affected by renal function.
Clinical Efficacy
Intubating conditions were clinically acceptable in 68 to 89% of adult patients at about 1 minute after administration of a single bolus of rapacuronium 1.5 mg/kg. Intubating conditions did not vary with bodyweight in adults or between adult and elderly patients, and appeared to be similar in the general adult population and in pregnant women undergoing Caesarean section. Clinically acceptable in-tubating conditions were provided by the recommended dose of rapacuronium 2 mg/kg in 100% of infants (aged 2 to 11 months) and children (aged 1 to 12 years) in 2 different studies.
Intubating conditions at about 1 minute after administration were clinically acceptable in 86 to 100% of patients who received rapacuronium 1.3 to 2.5 mg/kg versus in 88 to 97% of those who received suxamethonium chloride 1 or 1.5 mg/kg in 4 clinical trials. In the largest of these trials, intubating conditions were clinically acceptable significantly less often with rapacuronium 1.5 mg/kg than with suxamethonium chloride 1 mg/kg (n = 316; 89 vs 97% of patients).
Tolerability
The overall incidence of treatment-related adverse events with rapacuronium 0.3 to 3 mg/kg was 8% in clinical trials in a total of 1893 adult, elderly and paediatric patients, according to an unpublished summary of clinical trials of rapacuronium. Serious adverse events occurred in 0.3% of these patients.
The most common adverse events in 1300 adult rapacuronium recipients were bronchospasm (3.4% of patients), tachycardia (1.6%), injection site reaction (1.1%), hypotension (0.9%), increased airway pressure (0.6%) and erythematous rash (0.5%). Hypertension, fever, nausea and vomiting each occurred in <0.1% of patients. Bronchospasm was considered a serious adverse event in 2 and tachycardia, hypotension and upper airway obstruction each in 1 patient who received rapacuronium. There was no relationship between histamine levels and the incidence of adverse events which have been associated with histamine release induced with other NMBAs (e.g. hypotension, erythematous rash and bronchospasm).
In comparison with other nondepolarising NMBAs, the overall incidence of adverse events with rapacuronium 0.3 to 3 mg/kg (8%, n = 1893) appeared to be similar to that with mivacurium chloride 0.2 or 0.25 mg/kg (11%, n = 55) but may have been higher than that with vecuronium bromide 0.07 or 0.1 mg/kg (1%, n = 68). Additional data comparing rapacuronium and other nondepolarising NMBAs are limited.
The overall incidence of adverse events was similar with rapacuronium 1.5 or 2.5 mg/kg (8%, n = 630) or suxamethonium chloride 1 mg/kg (6%, n = 572) in adult patients. In patients who received rapacuronium, the incidence of bronchospasm (3.2 vs 1% of patients), tachycardia (2.5 vs 0%) and injection site reaction (2.2 vs 0.5%) tended to be higher, that of erythematous rash (1.4 vs 2.1%) or myalgia (0 vs 0.7%) tended to be lower, and that of hypotension (2.5 vs 2.1%) similar compared with in patients who received suxamethonium chloride.
The types of adverse events were generally similar in the general adult population and in elderly (n = 209) and paediatric (total of 168 infants and 177 children) patients who received rapacuronium. The most common adverse event was hypotension (5.3% of patients) in the older patients and tachycardia in infants (4.8%) and children (7.9%).
Dosage and Administration
Rapacuronium is indicated for endotracheal intubation and for maintenance of skeletal muscle relaxation in patients who are undergoing surgical procedures of short duration. Rapacuronium must be administered in conjunction with general anaesthesia and neuromuscular function should be continuously monitored during its use. Administration of rapacuronium by continuous infusion or to provide long term skeletal muscle relaxation is not recommended.
In adult patients, rapacuronium 1.5 mg/kg administered as a rapid intravenous bolus after anaesthetic induction is recommended to facilitate endotracheal intubation at about 1 minute after administration. Neostigmine 0.05 mg/kg can be used after rapacuronium to reduce the duration of action of rapacuronium, provided that ventilatory support is continued until the patient resumes normal res-piration.
No dosage adjustments are recommended in elderly patients or in adult patients with obesity or renal or hepatic dysfunction. The recommended dose in patients undergoing Caesarean section is an intravenous bolus of rapacuronium 2.5 mg/kg after anaesthetic induction with thiopental sodium. In paediatric patients (aged 1 month to 12 years), an intravenous bolus of rapacuronium 2 mg/kg in conjunction with halothane anaesthesia is recommended for endotracheal intubation.
In patients aged 13 to 17 years, the dose of rapacuronium should be individualised. Rapacuronium is not currently recommended for infants aged <1 month.
In adult patients, neuromuscular block is effectively maintained by ≤3 successive intravenous boluses of rapacuronium 0.5 mg/kg following an intravenous bolus of rapacuronium 1.5 mg/kg for endotracheal intubation. Additional boluses should not be administered until there is some recovery from neuromuscular block. There is evidence that rapacuronium can accumulate, causing a slower recovery, when multiple boluses are administered. This use of rapacuronium is not currently recommended in elderly or paediatric patients or in patients who receive an intubating dose of rapacuronium >1.5 mg/kg.
Similar content being viewed by others
References
Wiklund RA, Rosenbaum SH. Anesthesiology: First of two parts. N Engl J Med 1997 Oct 16; 337: 1132–41
Scott JM, Hunter JM. Use of the new neuromuscular blocking drugs in critically ill patients. Br J Intens Care 1996; 6(5): 163–4, 166–8
Goulden MR, Hunter JM. Rapacuronium (Org 9487): do we have a replacement for succinylcholine? [editorial I]. Br J Anaesth 1999 Apr; 82(4): 489–91
Booij LHDJ. Neuromuscular transmission and its pharmacological blockade Part 1: neuromuscular transmission and general aspects of its blockade. Pharm World Sci 1997 Feb; 19: 1–12
Fisher DM. Clinical pharmacology of neuromuscular blocking. Am J Health System Pharm 1998; 56 Suppl. 1: S1–S13
Sparr HJ. Rapid-sequence intubation with non-depolarizing muscle relaxants. Acta Anaesthesiol Scand 1997; 41 Suppl. 11: 111–3
Bevan DR. Neuromuscular blocking drugs: Onset and intubation. J Clin Anesth 1997; 9(6) Suppl.: 36S–9S
Savarese JJ. Some considerations on the new muscle relaxants. Anesth Analg 1998 Mar; 86 Suppl.: 119–27
Savarese JJ, Kitz RJ. The quest for a short-acting nondepolarizing neuromuscular blocking agent. Acta Anaesthesiol Scand 1973 Suppl. 53: 43–58
Bedford RE From the FDA [letter]. Anesthesiology 1995 Jan; 82(1): 33A
Booij LHDJ. Neuromuscular transmission and its pharmacological blockade. Part 3: continuous infusion of relaxants and reversal and monitoring of relaxation. Pharm World Sci 1997 Feb; 19: 35–44
Fu W, Klein KW, Sun R, et al. Effect of neostigmine on reversal of residual neuromuscular blockade after an infusion of ORG 9487 [abstract]. Anesth Analg 1998 Feb; 86 Suppl.: S445
Dempsey GA, Dods IM, Hunter JM. Pharmacodynamics of Org 9487 after a bolus dose followed by a continuous infusion in healthy patients [abstract no. 49]. Eur J Anaesthesiol 1997 Sep; 14 Suppl. 16: 30
van den Broek L, Wierda JM, Smeulers NJ, et al. Pharmacodynamics and pharmacokinetics of an infusion of Org 9487, a new short-acting steroidal neuromuscular blocking agent. Br J Anaesth 1994 Sep; 73: 331–5
Wierda JMKH, Beaufort AM, Kleef UW, et al. Preliminary investigations of the clinical pharmacology of three short-acting non-depolarizing neuromuscular blocking agents, Org 9453, Org 9489 and Org 9487. Can J Anaesth 1994 Mar; 41: 213–20
Wierda JMKH, van den Broek L, Proost JH, et al. Time course of action and endotracheal intubating conditions of Org 9487, a new short-acting steroidal muscle relaxant; a comparison with succinylcholine. Anesth Analg 1993 Sep; 77: 579–84
Reynolds LM, Infosino A, Brown R, et al. Intramuscular rapacuronium in infants and children. Anesthesiology 1999 Nov; 91(5): 1–12
Sparr HJ, Mellinghoff H, Blobner M, et al. Comparison of intubating conditions after rapacuronium (Org 9487) and succinylcholine following rapid sequence induction in adult patients. Br J Anaesth 1999 Apr; 82: 537–41
Abboud TK, Bikhazi G, Mroz L, et al. ORG 9487 vs succinylcholine in rapid sequence induction for cesarean section patients: maternal and neonatal effects [abstract]. Anesthesiology 1997 Sep; 87 Suppl: A906
Motsch J, Meakin G, Meretoja OA, et al. A dose-ranging study of ORG 9487 on endotracheal intubating conditions in infants and children [abstract]. Anesthesiology 1996 Sep; 85 Suppl: 1084
Viby-Mogensen J, Engbaek J, Eriksson LI, et al. Good clinical research practice (GCRP) in pharmacodynamic studies of neuromuscular blocking agents. Acta Anaesthesiol Scandinavica 1996; 40: 59–74
Wierda JMKH, Proost JH. Structure-pharmacodynamic-pharmacokinetic relationships of steroidal neuromuscular blocking agents. Eur J Anaesthesiol, Supplement 1995; 12(11): 45–54
Schiere S, Proost JH, Wierda JMKH. Pharmacokinetics and pharmacokinetic/-dynamic (PK/PD) relationship of ORG 9488, the 3-desacetyl metabolite of ORG 9487 [abstract no. A377]. Anesthesiology 1997; 87 (3A)
Meretoja OA, Taivainen T, Jalkanen L, et al. Afast-onset shortacting non-depolarizing neuromuscular blocker, ORG 9487, in infants and children [abstract]. Br J Anaesth 1996 Jun; 76 Suppl. 2: 95
Schiere S, van den Broek L, Proost JH, et al. Comparison of vecuronium with ORG 9487 and their interaction. Can J Anaesth 1997 Nov; 44: 1138–43
Schiere S, Proost JH, Schuringa M, et al. Pharmacokinetics and pharmacokinetic-dynamic relationship between rapacuronium (Org 9487) and its 3-desacetyl metabolite (Org 9488). Anesth Analg 1999; 88: 640–7
Curran MJ, Donati F, Bevan DR. Onset and recovery of atracurium and suxamethonium-induced neuromuscular blockade with simultaneous train-of-four and single twitch stimulation. Br J Anaesth 1987; 59: 989–94
Meistelman C. Effects on laryngeal muscles and intubating conditions with new generation muscle relaxants. Acta Anaesthesiol Belg 1997; 48: 11–4
Wright PMC, Brown R, Lau M, et al. A pharmacodynamic explanation for the rapid onset/offset of rapacuronium bromide. Anesthesiology 1999 Jan; 90: 16–23
Debaene B, Lieutaud T, Billard V, et al. ORG 9487 neuromuscular block at the adductor pollicis and the laryngeal adductor muscles in humans. Anesthesiology 1997 Jun; 86: 1300–5
Organon Teknika. Data on file. 1999
Kahwaji R, Bevan DR, Bikhazi G, et al. Dose-ranging study in younger adult and elderly patients of ORG 9487, a new, rapid-onset, short-duration muscle relaxant. Anesth Analg 1997 May; 84: 1011–8
Lichtor JL, Korttila K, Lane B, et al. Onset time, peak effect, and cardiovascular effects in adult patients after three different doses of ORG 9487 [abstract]. Anesthesiology 1996 Sep; 85 Suppl.: 805
Witkowski T, Barfkowski R, Huffnagle S. Onset and recovery of rapacuronium: a comparison with rocuronium [abstract]. Anesthesiology 1998; 89(3A): A978
Miguel R, Bartkowski R, Foldes FF, et al. Comparison of the neuromuscular effects of ORG9487, mivacurium and succinylcholine [abstract]. Anesth Analg 1998 Feb; 86 Suppl.: 482
Bowman WC, Rodger IW, Houston J, et al. Structure: action relationships among some desacetoxy analogues of pancuronium and vecuronium in the anesthetized cat. Anesthesiology 1988; 69: 57–62
Kopman AF. Pancuronium, gallamine and i/-tubocurarine compared: is speed of onset inversely related to drug potency? Anesthesiology 1989; 70: 915–20
Seheller MS, Zornow MH, Saidman LJ. Trachéal intubation without the use of muscle relaxants: a technique using propofol and varying doses of alfentanil. Anesth Analg 1992; 75: 788–93
Mahajan RP. Is suxamethonium now obsolete? Curr Anaesth Crit Care 1996; 7(6): 289–94
Connolly FM, Mirakhur RK, Loan PB, et al. Time course of action of Org 9487 with or without reversal: comparison with suxamethonium [abstract]. Br J Anaesth 1995 Apr; 74: 473P
Purdy R, Bevan DR, Donati F, et al. Early reversal of rapacuronium with neostigmine. Anesthesiology 1999 Jul; 91(1): 51–7
Hayes A, Reid J, Bresline D, et al. Comparison of recovery following suxamethonium and Org 9487 (rapacuronium) with and without neostigmine [abstract no. A.416]. Br J Anaesth 1999 Jun; 82 Suppl. 1: 125–6
Bevan DR. Monitoring and reversal of neuromuscular block. Am J Health System Pharm 1998; 56 Suppl. 1: Sl–9
Szenohradszky J, Caldwell JE, Wright PCM, et al. Influence of renal failure on the pharmacokinetics and neuromuscular effects of a single dose of rapacuronium bromide. Anesthesiology 1999 Jan; 90: 24–35
Duvaldestin P, Slavov V, Rimaniol J-M. ORG 9487 pharmacodynamics in patients with cirrhosis [abstract]. Anesthesiology 1997 Sep; 87 Suppl.: A864
Kaplan RF, Fletcher JE, Hannallah R, et al. The ED50 of ORG 9487 in infants and children [abstract]. Anesthesiology 1996 Sep; 85 Suppl.: 1059
Kaplan RF, Hannallah R, Darrow E, et al. Potency of ORG 9487 in neonates [abstract]. Anesth Analg 1997 Feb; 84 Suppl.: S437
Brandom BW, Bikhazi G, Ginsberg B, et al. Org 9487 in neonates and infants anaesthetized with nitrous oxide-halothane [abstract no.56]. Eur J Anaesthesiol 1997; 14 Suppl. 16: 33–4
Kenaan CA, Brandom BW, Bikhazi GB, et al. Neuromuscular effects of ORG9487 compared with 0.2 mg/kg of mivacurium in pediatric patients anesthetized with halothane [abstract]. Anesthesiology 1997 Sep; 87 Suppl.: A1047
Mills KG, Scott JM, Parker CJR, et al. Reversal of single and incremental doses of Org 9487 [abstract no. 50]. Eur J Anaesthesiol 1997 Sep; 14 Suppl. 16: 30–1
Danjoux GR, Mills K, Hunter JM, et al. Can antagonism of rapacuronium speed its offset sufficiently to emulate suxamethonium: neostigmine or edrophonium? [abstract]. Anaesth Intensive Care 1999 Feb; 27: 78–9
McCourt KC, Mirakhur RK, Lowry DW, et al. Spontaneous or neostigmine-induced recovery after maintenance of neuromuscular block with Org 9487 (rapacuronium) or rocuronium following an initial dose of Org 9487. Br J Anaesth 1999 May; 82: 755–6
Osmer C, Wulf K, Vögele C, et al. Cardiovascular effects of Org 9487 under isoflurane anaesthesia in man. Eur J Anaesthesiol 1998 Sep; 15: 585–9
Witkowski TA, Bartkowski RR, Huffnagle S, et al. Hemodynamic effects of bolus injection of ORG 9487: a comparison with mivacurium and succinylcholine [abstract]. Anesthesiology 1997 Sep; 87 Suppl.: A865
Levy JH, Pitts M, Thanopoulos A, et al. The effects of rapacuronium on histamine release and hemodynamics in adult patients undergoing general anesthesia. Anesth Analg 1999; 89: 290–5
Bikhazi GB, Deepika KD, Fonseca J, et al. Cardiovascular effects of ORG 9487 under nitrous oxide barbiturate, fentanyl anesthesia [abstract]. Anesth Analg 1996 Feb; 82 Suppl.: S29
Miguel R, Bartkowski R, Foldes FF, et al. The effect of two doses of ORG9487, succinylcholine and mivacurium on heart rate and blood pressure [abstract]. Anesthesiology 1997 Sep; 87 Suppl.: A847
Whitford AM, Godschalkx A, Robertson EN, et al. A clinical comparison of some cardiovascular and intraocular effects of ORG9487 vecuronium and succinylcholine [abstract]. Anesthesiology 1997 Sep; 87 Suppl.: A848
Muir AW, Sleigh T, Marshall RJ, et al. Neuromuscular blocking and cardiovascular effects of Org 9487, a new short-acting aminosteroidal blocking agent, in anaesthetized animals and in isolated muscle preparations. Eur J Anaesthesiol 1998 Jul; 15: 467–79
Yamaguchi K, Huraux C, Szlam F, et al. Vascular effects of ORG9487 in human mammary arteries, a new short acting muscle relaxant [abstract]. Anesth Analg 1998 Apr; 86: SCA109
Fisher DM, Kahwaji R, Bevan D, et al. Factors affecting the pharmacokinetic characteristics of rapacuronium. Anesthesiology 1999 Apr; 90: 993–1000
Lemmens HJM, Drover DR, White PF, et al. The population pharmacokinetics of rapacuronium [abstract]. Clin Pharmacol Ther 1999 Feb; 65: 178
Donati F, Varin F, Ducharme J, et al. Pharmacokinetics and pharmacodynamics of atracurium obtained with arterial and venous blood samples. Clin Pharmacol Ther 1991; 49: 515–22
Atherton DPL, Hunter JM. Clinical pharmacokinetics of the newer neuromuscular blocking drugs. Clin Pharmacokinet 1999 Mar; 36: 169–89
Sheiner LB, Stanski DR, Vozeh S, et al. Simultaneous modeling of pharmacokinetics and pharmacodynamics: application to d-turbocurarine. Clin Pharmacol Ther 1979 Mar; 25(3): 358–71
Plaud B, Proost JH, Wierda JMKH, et al. Pharmacokinetics and pharmacodynamics of rocuronium at the vocal cords and the adductor pollicis in humans. Clin Pharmacol Ther 1995; 58(2): 185–91
Fisher DM, Wright PMC. Are plasma concentration values necessary for pharmacodynamic modeling of muscle relaxants? Anesthesiology 1997; 86: 567–75
Proost JH, Roggeveld J, Wierda JMKH, et al. Relationship between chemical structure and physicochemical properties of series of bulky organic cations and their hepatic uptake and biliary excretion rates. J Pharmacol Exp Ther 1997; 282(2): 715–26
Szenohradszky J, Caldwell JE, Sharma ML, et al. Interaction of rocuronium (ORG 9426) and phenytoin in a patient undergoing cadaver renal transplantation: a possible pharmacokinetic mechanism? Anesthesiology 1994; 80: 1167–70
Meistelman C, Rowan C, Lacroix O, et al. Comparison of intubating conditions after administration of Org 9487 and succinylcholine [abstract]. Br J Anaesth 1999 Jun; 82 Suppl. 1: 147
Goldberg ME, Larijani GE, Azad SS, et al. Comparison of tracheal intubating conditions and neuromuscular blocking profiles after intubating doses of mivacurium chloride or succinylcholine in surgical outpatients. Anesth Analg 1989; 69: 93–9
Organon Inc. Org 9487 for injection: integrated summary of safety information. Data on file, 1997 Oct
Naguib M, Samarkandi AH, Bakhamees HS, et al. Histamine-release haemodynamic changes produced by rocuronium, vecuronium, mivacurium, atracurium and tubocurarine. Br J Anaesth 1995; 75: 588–92
Organon Inc. Raplon™ (rapacuronium bromide) prescribing information. West Orange, New Jersey, USA, 1999
Øberg B, Poulsen TD. Obesity: an anaesthetic challenge. Acta Anaesthesiol Scand 1996; 40: 191–200
Bartkowski RR. Recent advances in neuromuscular blocking agents. Am J Health System Pharm 1999 Jun 1; 56 Suppl. 1: S14–17
Author information
Authors and Affiliations
Corresponding author
Additional information
Various sections of the manuscript reviewed by: D.P.L. Atherton, Department of Anaesthesia, University of Liverpool, Liverpool, England; D.R. Bevan, Department of Anaesthesia, Vancouver Hospital, Vancouver, British Columbia, Canada; J.E. Caldwell, Departments of Anesthesia and Perioperative Care, University of California, San Francisco, California, USA; D.M. Fisher, Department of Anesthesia, University of California, San Francisco, California, USA; M.E. Goldberg, Department of Anesthesiology, University of Medicine and Dentistry of New Jersey, Camden, New Jersey, USA; A.F. Kopman, Department of Anesthesiology, St Vincents Hospital and Medical Center, New York, New York, USA; G.E. Larijani, Department of Anesthesiology, University of Medicine and Dentistry of New Jersey, Camden, New Jersey, USA; C. Meistelman, Department of Anaesthesia and Intensive Care Medicine, Centre Hospitalier Régional de Nancy, Vandoevre, France; J.J. Savarese, Department of Anesthesiology, Weill Medical College of Cornell University, New York, New York, USA; H.J. Sparr, Department of Anaesthesia and Intensive Care Medicine, University of Innsbruck, Innsbruck, Austria.
Data Selection
Sources: Medical literature published in any language since 1966 on rapacuronium bromide, identified using AdisBase (a proprietary database of Adis International, Auckland, New Zealand), Medline and EMBASE. Additional references were identified from the reference lists of published articles. Bibliographical information, including contributory unpublished data, was also requested from the company developing the drug.
Search strategy: AdisBase search terms were ‘rapacuronium-bromide’ or ‘ORG-9487’. Medline search terms were ‘rapacuronium-bromide’ or ‘ORG 9487’. EMBASE search terms were ‘rapacuronium-bromide’ or ‘ORG 9487’. Searches were last updated 15 October 1999.
Selection: Studies in patients undergoing endotracheal intubation who received rapacuronium bromide. Inclusion of studies was based mainly on the methods section of the trials. When available, large, well controlled trials with appropriate statistical methodology were preferred. Relevant pharmacodynamic and pharmacokinetic data are also included.
Index terms: Rapacuronium bromide, intubation, neuromuscular blocking agent, pharmacodynamics, pharmacokinetics, therapeutic use, adverse events.
Rights and permissions
About this article
Cite this article
Onrust, S.V., Foster, R.H. Rapacuronium Bromide. Drugs 58, 887–918 (1999). https://doi.org/10.2165/00003495-199958050-00011
Published:
Issue Date:
DOI: https://doi.org/10.2165/00003495-199958050-00011