Summary
Synopsis
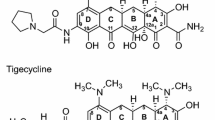
Ciprofloxacin is one of a new generation of fluorinated quinolones structurally related to nalidixic acid. The primary mechanism of action of ciprofloxacin is inhibition of bacterial DNA gyrase. It is a broad spectrum antibacterial drug to which most Gram-negative bacteria are highly susceptible in vitro and many Gram-positive bacteria are susceptible or moderately susceptible. Unlike most broad spectrum antibacterial drugs, ciprofloxacin is effective after oral or intravenous administration.
Ciprofloxacin has been most extensively studied following oral administration. It attains concentrations in most tissues and body fluids which are at least equivalent to the minimum inhibitory concentration designated as the breakpoint for bacterial susceptibility in vitro. The results of clinical trials with orally and intravenously administered ciprofloxacin have confirmed the potential for its use in a wide range of infections, which was suggested by its in vitro antibacterial and pharmacokinetic profiles. It has proven an effective treatment for many types of systemic infections as well as for both acute and chronic infections of the urinary tract.
Ciprofloxacin generally appeared to be at least as effective as alternative orally administered antibacterial drugs in the indications in which they were compared, and in some indications, to parenterally administered antibacterial therapy. However, further studies are needed to fully clarify the comparative efficacy of ciprofloxacin and standard antibacterial therapies.
Bacterial resistance to ciprofloxacin develops infrequently, both in vitro and clinically, except in the setting of pseudomonal respiratory tract infections in cystic fibrosis patients. The drug is also well tolerated. Thus, as an orally active, broad spectrum and potent antibacterial drug, ciprofloxacin offers a valuable alternative to broad spectrum parenterally administered antibacterial drugs for use in a wide range of clinical infections, including difficult infections due to multiresistant pathogens.
Antibacterial Activity
Ciprofloxacin is a fluorinated quinolone, with the most potent in vitro antibacterial activity against most bacterial species of all the newer quinolones marketed to date. The primary mechanism of action of ciprofloxacin and other quinolones involves inhibition of bacterial DNA gyrase. Ciprofloxacin has an MIC90 of ⩽ 1 mg/L (indicating susceptibility) against all species of Enterobacteriaceae, except some species of Providencia. Acinetobacter species, Neisseria gonorrhoeae, Neisseria meningitidis, Branhamella catarrhalis and Haemophilus species (including β-lactamase negative and positive strains) were also highly susceptible to ciprofloxacin. Pseudomonas aeruginosa was susceptible (MIC90 range 0.12–1 mg/L), but ciprofloxacin was less active against other Pseudomonas species (MIC90 range 0.25–16 mg/L). Other Gram-negative organisms susceptible to ciprofloxacin include Campylobacter jejuni, Vibrio species and Legionella species, while Gardnerella vaginalis was only moderately susceptible. In general, against Gram-negative aerobes in vitro, ciprofloxacin has equivalent activity, or was more potent by 1 or 2 dilutions than ofloxacin, and was consistently more potent than other quinolones such as norfloxacin, enoxacin or pefloxacin.
Staphylococcus species, such as S. epidermidis, S. saprophyticus and S. aureus (ineluding penicillin-resistant and methicillin-resistant strains) were susceptible to ciprofloxacin (MIC90 range 0.12–1 mg/L). Streptococcus species, including penicillin-resistant strains of S. pneumoniae, were moderately susceptible to ciprofloxacin (MIC90 range 0.5–6.3 mg/L). Among the marketed quinolones only ofloxacin has similar activity to ciprofloxacin in vitro against Gram-positive organisms. Among the non-quinolones reviewed only cefotaxime and mezlocillin show greater activity against non-enterococcal streptococci and only imipenem shows greater activity against S. aureus.
Mycobacterium tuberculosis, Mycobacterium fortuitum, Mycobacterium intracellulare and Listeria monocytogenes were susceptible or moderately susceptible to ciprofloxacin, but other Mycobacterium species and Nocardia asteroides tended to be resistant (MIC90 range ⩾ 4 mg/L).
Ciprofloxacin has a broad range of reported MIC90 values against Bacteroides species (0.06–32 mg/L); B. oralis and B. ureolyticus tended to be susceptible while B. fragilis tended to be resistant. Peptococcus species were moderately susceptible to ciprofloxacin, but Peptostreptococcus species and Clostridium species were resistant. Chlamydia trachomatis proved moderately susceptible (MIC range 0.5–2 mg/L).
The antibacterial activity of ciprofloxacin is influenced little, if at all, by inoculum size, growth medium or the presence of serum. However, both bacteriostatic and bactericidal activities (which are achieved at similar concentrations for ciprofloxacin) are reduced by magnesium ions and acidity, which may account for the drug’s reduced activity in urine.
Mutants having reduced susceptibility to ciprofloxacin emerge at a relatively low incidence in vitro. Moreover, strains which become less susceptible to ciprofloxacin rarely become resistant (i.e. MIC values generally remain < 4 mg/L). Cross-resistance with nalidixic acid or other quinolones occurs, but it is rare with non-quinolone antibacterial drugs. The mechanisms of resistance to quinolones are unclear. Plasmid-mediated resistance does not occur, but chromosomal mutation influencing DNA gyrase and/or the cell membrane may confer resistance.
Pharmacological Effects
Ciprofloxacin has little, if any, effect on chemotaxis of — and may increase phagocytosis and killing by — polymorphonuclear leucocytes. At concentrations up to 125 mg/L it has no effect on human mitogen-stimulated mononuclear cell proliferation.
In the gastrointestinal tract ciprofloxacin markedly reduces or eradicates Enterobacteriaceae, with a less dramatic effect against staphylococci and enterococci and little effect on the anaerobic microflora. There is little evidence of overgrowth or superinfection.
Preclinical toxicology studies, including ophthalmological examination, in various animal species reveal no significant evidence of toxicity. In young rats and dogs ciprofloxacin does cause articular damage, but the clinical implications, if any, are unknown.
Pharmacokinetics
After oral administration of single doses (50 to l000mg) of ciprofloxacin, peak serum concentrations of 0.28 to 5.92 mg/L were reached within 0.5 to 2 hours. Mean peak concentrations increased in proportion to the dose within the normal therapeutic range. Multiple dose administration for up to 8 days in healthy volunteers, either orally (500mg bid) or intravenously (200mg bid), did not produce significant drug accumulation. Food had no significant effect on the pharmacokinetics of ciprofloxacin, except to delay absorption, but simultaneous administration of antacids containing magnesium hydroxide and/or aluminium hydroxide with ciprofloxacin reduced the bioavailability of the latter. Following intravenous administration, the plasma concentration profile of ciprofloxacin is best characterised by a 3-compartment open model. The absolute bioavailability of oral ciprofloxacin averages between 69 and 85%.
The apparent volume of distribution of ciprofloxacin was calculated to be approximately 2 to 3 L/kg. The volume of the central compartment was between 0.16 and 0.63 L/kg, which approximately represents the total volume of extracellular water. The tissue concentrations achieved are at least as high as the serum concentrations for most tissues. Ciprofloxacin was approximately 16 to 40% bound to plasma proteins.
After administration of a single oral dose (259mg) of 14C-labelled ciprofloxacin to healthy volunteers, approximately 94% of the dose was recovered in urine and faeces over 5 days, with most radioactivity being recovered in the urine (55.4%). This study demonstrates that unchanged ciprofloxacin is the major moiety in both urine (45%) and faeces (25%). After a single intravenous dose (107mg) of 14C-labelled ciprofloxacin to healthy volunteers, approximately 89% of the dose was recovered in urine and faeces over 5 days with about 75% of radioactivity being recovered in the urine. As with oral dosage, unchanged ciprofloxacin is also the major moiety in urine (62%) and faeces (15%). Small amounts of 4 metabolites are present in urine and faeces, all with some antibacterial activity, but less than that of ciprofloxacin.
Total serum clearance of ciprofloxacin in healthy volunteers ranged from 23 to 43 L/h/1.73m2. Renal clearance accounts for approximately 60 to 70% of total serum clearance, and was approximately 3 times higher than creatinine clearance. Active tubular secretion of ciprofloxacin is confirmed by the observation that coadministration of probenecid decreases the ciprofloxacin renal clearance.
The elimination half-life of ciprofloxacin after single and multiple doses ranged from 3.4 to 6.9 hours following oral administration (50 to 1000mg) and from 3 to 4.4 hours following intravenous administration (50 to 200mg).
The pharmacokinetics of ciprofloxacin are altered in patients with renal dysfunction. After single doses, peak serum concentration, area under the serum concentration-time curve (AUC) and elimination half-life are substantially increased depending on the degree of renal impairment. Thus, dosage adjustment may be required in such subjects. Ciprofloxacin is poorly removed from the body by haemodialysis. The pharmacokinetics of ciprofloxacin are generally not affected to a clinically significant extent by age or the presence of cystic fibrosis. However, serum concentrations tend to be higher in elderly subjects, possibly due to diminished renal function or changes in volume of distribution.
Therapeutic Trials
With its broad spectrum of antibacterial activity and widespread distribution to most tissues and body fluids, ciprofloxacin should have potential therapeutic application in many types of infection. Cumulated European and US clinical trial data revealed that ciprofloxacin (in most cases administered orally in a daily dosage of 500 to 1500mg divided into two 12-hourly doses, for 7 to 14 days) was clinically effective in greater than 88% of patients with infections of the urinary tract, respiratory tract, skin and skin structure, bones or joints, gastrointestinal tract, blood and gynaecological organs. In Japanese patients (most of whom received 200mg of oral ciprofloxacin 3 times daily) cumulated clinical trial data revealed clinical efficacy rates of greater than 80% in most infection types and of approximately 75% in lower respiratory tract infections, and ear, nose and throat infections. High rates of clinical efficacy were achieved in infections due to most Gram-positive and Gram-negative pathogens, including multiresistant but ciprofloxacinsusceptible nosocomial pathogens. However, only 43.2% of patients in Japan with infections of various sites due to P. aeruginosa responded versus approximately 75% of non-Japanese patients, a difference which may be a consequence of the lower dosages used in Japan as compared with the rest of the world. Bacterial eradication rates for most species of pathogens reported in data cumulated worldwide are generally 75% or greater, with the majority being 85% or greater. P. aeruginosa is again an exception in the Japanese data, being eradicated from only 22.7% of infections.
As with many broad spectrum antibacterial drugs, superinfection due to Candida species or bacterial pathogens occurs with ciprofloxacin, in some cases requiring additional antimicrobial therapy. Development of resistance or reduced susceptibility to ciprofloxacin generally occurs infrequently. However, transitory, or in a few cases persistent, resistance to P. aeruginosa is commonly encountered among cystic fibrosis patients. In addition, among debilitated patients or in those suffering chronic and/or complicated infections, emergence of reisistance to P. aeruginosa or other bacteria occurs occasionally and has resulted in clinical treatment failures. Cross-resistance has been reported rarely in Pseudomonas species between ciprofloxacin and aminoglycosides, ureidopenicillins and cephalosporins, and cross-resistance has also been reported between ciprofloxacin and aminoglycosides in S. aureus.
Several small randomised studies have compared the clinical efficacy of ciprofloxacin and alternative antibacterial drugs in the treatment of urinary tract infections (UTI). While none of these trials provided statistical analyses of the results, oral ciprofloxacin appeared to be similar in clinical and bacteriological efficacy to orally administered cotrimoxazole (trimethoprim/sulphamethoxazole) [complicated and uncomplicated infections], trimethoprim (uncomplicated infections), norfloxacin (complicated infections) and cinoxacin (uncomplicated infections). Intravenous ciprofloxacin appeared to be similar in clinical and bacteriological efficacy to intravenous mezlocillin (complicated infections). In addition, in a large Japanese study, oral ciprofloxacin 200mg 3 times daily was reported to be statistically superior to oral norfloxacin 200mg 4 times daily in both clinical efficacy and bacterial eradication rates in the treatment of complicated UTI. Of note, in the above studies the incidence of side effects was lower with ciprofloxacin than with co-trimoxazole.
Results of several comparative and non-comparative studies indicated that single oral doses of ciprofloxacin 100 to 2000mg (usually 100 to 500mg) produced 100% bacteriological cure rates in gonococcal urethritis. Comparative rates for single doses of ampicillin 2 to 3.5g plus probenecid 1g were 90 to 92%. Ciprofloxacin was consistently effective against penicillinase-producing strains of N. gonorrhoeae, and was often effective in curing oropharyngeal or rectal infections. In contrast, ciprofloxacin lacks a reliable degree of clinical efficacy in non-gonococcal urethritis due to Chlamydia trachomatis or Ureaplasma urealyticum.
Ciprofloxacin appears to be similar to or, in the studies which analysed the results statistically, was not significantly different in clinical efficacy from doxycycline, cephalexin, amoxycillin, bacampicillin or co-trimoxazole in various lower respiratory tract infections. Randomised comparative studies showed oral ciprofloxacin to be statistically (p < 0.001) superior to cefaclor in clinical efficacy in the treatment of infectious exacerbations of chronic bronchitis and other chronic lung diseases, and statistically (p < 0.05) superior to ampicillin in clinical efficacy in outpatients with acute bronchitis.
Several randomised comparative studies documented the efficacy of oral ciprofloxacin in young adult patients with cystic fibrosis who were suffering from lower respiratory tract infections due, in most instances, to colonising P. aeruginosa. Statistical analyses in 2 separate studies demonstrated that ciprofloxacin 500 or 750mg twice daily was generally no different in clinical efficacy to the combination of intravenous azlocillin plus an aminoglycoside, although in one of these two studies oral ciprofloxacin produced a superior improvement in 2 parameters of lung function (p < 0.05). Two crossover studies showed no statistically significant difference in clinical efficacy between twice daily oral administration of ciprofloxacin (500 or 750mg) and ofloxacin (400mg). Because of the potential for the development of resistant P. aeruginosa, ciprofloxacin is not recommended for long term prophylaxis or multiple sequential courses of treatment in recurrent lung infections in cystic fibrosis patients.
Three double-blind randomised studies revealed oral ciprofloxacin 750mg twice daily to be not statistically different in clinical efficacy from intravenous cefotaxime 2g 3 times daily in skin and soft tissue infections. A fourth study, involving mild to moderate infections, reported significantly (p < 0.05) more failures among the cefotaxime-treated patients (21% vs 3%).
Several case studies reported the successful treatment with ciprofloxacin of systemic Salmonella infections in immunocompromised patients. Encouraging preliminary results were also noted in other immunocompromised patients with fever or documented infection. Prophylaxis of remission induction therapy with oral ciprofloxacin 500mg twice daily resulted in a significantly (p < 0.05) lower infection rate (18%) than prophylaxis with the combination of co-trimoxazole 160/800mg plus colistin 200mg orally 3 times daily (50%). However, results of both prophylaxis and treatment in immunocompromised patients suggest that streptococci and staphylococci may not be adequately inhibited by ciprofloxacin alone.
Treatment with ciprofloxacin eliminates nasopharyngeal carriage of Neisseria meningitidis and gastrointestinal carriage of Salmonella species and nosocomial Klebsiella species.
Side Effects
Significant adverse effects associated with ciprofloxacin therapy are uncommon. The overall worldwide incidence of side effects in patients treated with the drug was reported to be from 5 to 10%, and therapy had to be discontinued in less than 2% of patients. Gastrointestinal symptoms, mainly nausea, vomiting, abdominal pain, diarrhoea, and anorexia, were reported most frequently (in up to 10% of patients receiving higher oral dosages), followed by central nervous system events such as anxiety, nervousness, insommia, euphoria, tremor and, very rarely, seizures and hallucinations (1 to 4%), and hypersensitivity reactions of a dermatological nature (1%). Other untoward effects that have been reported rarely (incidence less than 1%) include eye disorders and chest pain. Mild, transient alterations in laboratory values were sometimes observed [eosinophilia, elevated serum creatinine, blood urea nitrogen, AST (SGOT) and ALT (SGPT)], although their clinical significance is unknown. Isolated cases of haematuria, interstitial nephritis and arthropathy have also been reported.
Dosage and Administration
Ciprofloxacin is usually administered orally as a twice daily regimen in a total daily dosage of 500 to 1500mg depending on the nature and severity of the infection. For mild to moderate urinary tract infections a total daily dosage of 500mg is usually appropriate, while 1000mg daily is recommended for severe or complicated urinary tract infections, and mild to moderate respiratory tract, bone and joint, or skin and skin structure infections. For severe or complicated respiratory tract infections a dosage of 1500mg daily is recommended. In Japan the standard recommended oral dosage is 200mg 3 times daily.
The recommended dosage of ciprofloxacin administered intravenously is 100mg twice daily in urinary tract infections and 200mg twice daily in other infections. In patients with pseudomonal or staphylococcal infections, or in immunocompromised patients, a dosage of 300mg twice daily may be used.
Dosage adjustments for altered renal function are usually not required except in patients with severe renal impairment (creatinine clearance ⩽ 20 ml/min) in whom the total daily dose may be reduced by one-half.
Elevated plasma concentrations of theophylline and a prolongation of its elimination half-life may result from the concurrent administration of ciprofloxacin with theophylline. If concomitant use cannot be avoided, plasma concentrations of theophylline should be monitored and dosage adjustments made as appropriate.
Antacids containing magnesium and/or aluminium hydroxide interfere with the absorption of ciprofloxacin, resulting in subtherapeutic serum and urine concentrations. Thus, concurrent administration of these antacids with ciprofloxacin should be avoided.
Similar content being viewed by others
References
Aigner KR, Dalhoff A. Penetration activities of ciprofloxacin into muscle, skin and fat following oral administration. Journal of Antimicrobial Chemotherapy 18: 644–645, 1986
Aldridge KE, Janney A, Sanders CV. Comparison of the activities of coumermycin, ciprofloxacin, teicoplanin, and other non β-lactam-antibiotics against clinical isolates of methicillin-resistant Staphylococcus aureus from various geographical locations. Antimicrobial Agents and Chemotherapy 28: 634–638, 1985a
Aldridge KE, Schiro DD, Tsai L, Janney A, Sanders CV, et al. Ciprofloxacin (Bay o 9867): an in vitro comparison with other broad spectrum antibiotics. Current Therapeutic Research 37: 754–762, 1985b
Alfaham M, Holt ME, Goodchild MC. Arthropathy in a patient with cystic fibrosis taking ciprofloxacin. British Medical Journal 295: 699, 1987
Aoki FY, Conly JM, Hoban D, McLeod J, Chubb H, et al. Pharmacokinetics of ciprofloxacin and effect of ciprofloxacin on the fecal flora in volunteers on a vitamin K1-deficient diet. Proceedings of the 24th Interscience Conference on Antimicrobial Agents and Chemotherapy, abstract no. 765, Washington D.C., USA, 1984
Appelbaum PC, Spangler SK, Sollenberger L. Susceptibility of non-fermentative Gram-negative bacteria to ciprofloxacin, norfloxacin, amifloxacin, pefloxacin and cefpirome. Journal of Antimicrobial Chemotherapy 18: 675–679, 1986
Arcieri G, August R, Becker N, Doyle C, Griffith E, et al. Clinical experience with ciprofloxacin in the USA. European Journal of Clinical Microbiology 5: 220–225, 1986
Arcieri G, et al. Ciprofloxacin: an update on clinical experience. American Journal of Medicine 82(Suppl. 4A): 381–386, 1987
Aronoff GE, Kenner CH, Sloan RS, Pottratz ST. Multiple-dose ciprofloxacin kinetics in normal subjects. Clinical Pharmacology and Therapeutics 36: 384–388, 1984
Arya OP, Hobson D, Hart CA, Bartzokas C, Pratt BC. Evaluation of ciprofloxacin 500mg twice daily for one week in treating uncomplicated gonococcal, chlamydial, and non-specific urethritis in men. Genitourinary Medicine 62: 170–174, 1986
Auckenthaler R, Michéa-Hamzehpour M, Pechère JC. In-vitro activity of newer quinolones against aerobic bacteria. Journal of Antimicrobial Chemotherapy 17(Suppl. B): 29–39, 1986
Azadian BS, Bendig JWA, Samson DM. Emergence of ciprofloxacin-resistant Pseudomonas aeruginosa after combined therapy with ciprofloxacin and amikacin. Journal of Antimicrobial Chemotherapy 18: 771, 1986
Aznar J, Prados R, Rodriguez Pichardo A, Hernandez I, De Miguel C, et al. Comparative clinical efficacy of two different single-dose ciprofloxacin treatments for uncomplicated gonorrhea. Sexually Transmitted Diseases 13: 169–171, 1986
Aznar J, Caballero MC, Lozano MC, de Miguel C, Palomares JC, et al. Activities of new quinolone derivatives against genital pathogens. Antimicrobial Agents and Chemotherapy 27: 76–78, 1985
Baba S. Clinical evaluation of ciprofloxacin in the fields of surgery, obstetrics and gynecology, dermatology, otorhinolaryngology and ophthalmology. Proceedings of the 14th International Congress of Chemotherapy, Kyoto, Japan, Jun, 1985
Baba S, Kinoshita H, Mori Y, Suzuki K, Shimada J, et al. Comparative study of ciprofloxacin (Bay o 9867) and norfloxacin in the treatment of acute lacunar tonsillitis. JIBI (Ear and Nose) 33: 312–336, 1987
Ball AP, Fox C, Ball ME, Brown IRF, Willis JV. Pharmacokinetics of oral ciprofloxacin, 100mg single dose, in volunteers and elderly patients. Journal of Antimicrobial Chemotherapy 17: 629–635, 1986
Ball AP. Ciprofloxacin: an overview of adverse experiences. Journal of Antimicrobial Chemotherapy 18(Suppl. D): 187–193, 1986
Bamberger DM, Peterson LR, Gerding DN, Moody JA, Fasching CE. Ciprofloxacin, azlocillin, ceftizoxime and amikacin alone and in combination against Gram-negative bacilli in an infected chamber model. Journal of Antimicrobial Chemotherapy 18: 51–63, 1986
Banerjee DK. Ciprofloxacin (4-quinolone) and Mycobacterium leprae. Leprosy Reviews 57: 159–162, 1986
Bantz P-M, Grote J, Peters-Haertel W, Stahmann J, Timm J, et al. Low-dose ciprofloxacin in respiratory tract infections. A randomized comparison with doxycycline in general practice. American Journal of Medicine 82(Suppl. 4A): 208–210, 1987
Barry AL, Jones RN. Cross-resistance among cinoxacin, ciprofloxacin, DJ-6783, enoxacin, nalidixic acid, norfloxacin, and oxolinic acid after in vitro selection of resistant populations. Antimicrobial Agents and Chemotherapy 25: 775–777, 1984
Barry AL, Jones RN, Thornsberry C, Ayers LW, Gerlach EH, et al. Antibacterial activities of ciprofloxacin, norfloxacin, oxolinic acid, cinoxacin, and nalidixic acid. Antimicrobial Agents and Chemotherapy 25: 633–637, 1984
Bayer AS, Blomquist IK, Kim KS. Ciprofloxacin in experimental aortic valve endocarditis due to Pseudomonas aeruginosa. Journal of Antimicrobial Chemotherapy 17: 641–649, 1986a
Bayer AS, Kim KS. In vivo efficacy of azlocillin and amikacin versus ciprofloxacin with and without amikacin in experimental right-sided endocarditis due to Pseudomonas aeruginosa. Chemotherapy 32: 364–373, 1986
Bayer AS, Lindsay P, Yih J, Hirano L, Lee D, Blomquist IK. Efficacy of ciprofloxacin in experimental aortic valve endocarditis caused by a multiply-β-lactam-resistant variant of Pseudomonas aeruginosa stably derepressed for β-lactamase production. Antimicrobial Agents and Chemotherapy 30: 528–531, 1986b
Bayer AS, Norman DC, Blomquist IK. Comparative efficacy of ciprofloxacin and ceftriaxone in experimental arthritis caused by Escherichia coli. Antimicrobial Agents and Chemotherapy 30: 184–186, 1986c
Bayer AS, Norman D, Anderson D. Efficacy of ciprofloxacin in experimental arthritis caused by Escherichia coli — in vitro and in vivo correlations. Journal of Infectious Diseases 152: 811–816, 1985
Bayer A, Gajewska A, Stephens M, Marshal-Stark J, Pathy J. Pharmacokinetics of ciprofloxacin in the elderly. Respiration 51: 292–295, 1987
Beermann D, Wingender W, Horstmann R. Intravenous infusion regimen for rapidly achieving steady-state levels of ciprofloxacin. American Journal of Medicine 82(Suppl. 4A): 360–362, 1987
Beermann D, Scholl H, Wingender W, Förster D, Beubler E, et al. Metabolism of ciprofloxacin in man. In Neu HC & Weuta H (Eds) 1st International Ciprofloxacin Workshop, Leverkusen 1985, pp. 141–146, Excerpta Medica, Amsterdam, 1986
Behrens-Baumann W, Martell J. Ciprofloxacin concentrations in human aqueous humor following intravenous administration. Chemotherapy (Basel) 33: 328–330, 1987
Bender SW, Dalhoff A, Shah PM, Strehl R, Posselt HG. Ciprofloxacin pharmacokinetics in patients with cystic fibrosis. Infection 14: 17–21, 1986
Bendig JWA, Kyle PW, Giangrande PLF, Samson DM, Azadian BS. Two neutropenic patients with multiple resistant Pseudomonas aeruginosa septicaemia treated with ciprofloxacin. Journal of the Royal Society of Medicine 80: 316–317, 1987
Bergan T, Delin C, Johansen S, Kolstad IM, Nord CE, et al. Pharmacokinetics of ciprofloxacin and effect of repeated dosage on salivary and fecal microflora. Antimicrobial Agents and Chemotherapy 29: 298–302, 1986a
Bergan T, Engeset A, Olszewski W, Østby N, Solberg R. Pharmacokinetics of ciprofloxacin in peripheral lymph and skin blisters. European Journal of Clinical Microbiology 5: 458–461, 1986b
Bergan T, Thorsteinsson SB, Kolstaad IM, Johansen S. Pharmacokinetics of ciprofloxacin and increasing oral doses. European Journal of Clinical Microbiology 5: 187–192, 1986c
Bergan T, Thorsteinsson SB, Solberg R, Bjornskou L, Kolstad IM, et al. Pharmacokinetics of ciprofloxacin: intravenous and increasing oral doses. American Journal of Medicine 82(Suppl. 4A): 97–102, 1987
Bergogne-Bérézin E, Berthelot G, Even P, Stern M, Reynaud P. Penetration of ciprofloxacin into bronchial secretions. European Journal of Clinical Microbiology 5: 197–200, 1986
Blaser J, Dudley MN, Gilbert D, Zinner SH. Influence of medium and method on the in vitro susceptibility of Pseudomonas aeruginosa and other bacteria to ciprofloxacin and enoxacin. Antimicrobial Agents and Chemotherapy 29: 927–929, 1986
Boelaert J, Valcke Y, Schurgers M, Daneels R, Rosseneu M, et al. The pharmacokinetics of ciprofloxacin in patients with impaired renal function. Journal of Antimicrobial Chemotherapy 16: 87–93, 1985
Boerema JBJ, Dalhoff A, Debruyne FMY. Ciprofloxacin distribution in prostatic tissue and fluid following oral administration. Chemotherapy 31: 13–18, 1985a
Boerema J, Boll B, Muytjens H, Branolte J. Efficacy and safety of ciprofloxacin (Bay 0 9867) in the treatment of patients with complicated urinary tract infections. Journal of Antimicrobial Chemotherapy 16: 211–217, 1985b
Borner K, Lode H, Höffken G. Renal elimination of sulpho-ciprofloxacin, a new metabolite of ciprofloxacin. European Journal of Clinical Microbiology 5: 476, 1986
Borobio MV, Perea EJ. Effect of inoculum, pH, and medium on the activity of ciprofloxacin against anaerobic bacteria. Antimicrobial Agents and Chemotherapy 25: 342–343, 1984
Bosch J, Linares J, López de Goicoechea MJ, Ariza J, Cisnal MC, et al. In-vitro activity of ciprofloxacin, ceftriaxone and five other antimicrobial agents against 95 strains of Bruceila melitensis. Journal of Antimicrobial Chemotherapy 17: 459–461, 1986
Bosso JA, Black PG. Efficacy of ciprofloxacin in adults with cystic fibrosis (Abstract No. 30). Drug Intelligence and Clinical Pharmacy 21: 8A, 1987
Bosso JA, Black PG, Matsen JM. Ciprofloxacin versus tobramycin plus azlocillin in pulmonary exacerbations in adult patients with cystic fibrosis. American Journal of Medicine 82(Suppl. 4A): 180–184, 1987
Brittain DC, Scully BE, McElrath MJ, Steinman R, Labthavikul P, et al. The pharmacokinetics and serum and urine bactericidal activity of ciprofloxacin. Journal of Clinical Pharmacology 25: 82–88, 1985
Brown EM, Morris R, Stephenson TP. Efficacy and safety of ciprofloxacin in the treatment of chronic Pseudomonas aeruginosa urinary tract infection. Journal of Antimicrobial Chemotherapy 18(Suppl. D): 123–127, 1986
Brumfitt W, Franklin I, Grady D, Hamilton-Miller JMT, Iliffe A. Changes in the pharmacokinetics of ciprofloxacin and fecal flora during administration of a 7-day course to human volunteers. Antimicrobial Agents and Chemotherapy 26: 757–761, 1984
Brunner H, Zeiler H-J, Luckhaus G. Efficacy of ciprofloxacin in experimental Mycoplasma pneumoniae infection of hamsters. Abstract no. 272 of the 24th Interscience Conference on Antimicrobial Agents and Chemotherapy, Washington D.C., USA, 1984
Bruns BJ, Wallace MR. Treatment of Salmonella typhimurium infection in a renal transplant patient with ciprofloxacin. New Zealand Medical Journal 100: 190, 1987
Bryant RE, Harstein AI. Oral ciprofloxacin in refractory gram-negative bacillary infections. International Journal of Clinical Pharmacology Research 7: 187–194, 1987
Carmona O, Hernandez-Gonzalez S, Kobelt R. Ciprofloxacin in the treatment of nonspecific vaginitis. American Journal of Medicine 82(Suppl. 4A): 321–323, 1987
Carpenter TC, Hackbarth CJ, Chambers HF, Sande MA. Efficacy of ciprofloxacin for experimental endocarditis caused by methicillin-susceptible or -resistant strains of Staphylococcus aureus. Antimicrobial Agents and Chemotherapy 30: 382–384, 1986
Casal M, Rodriguez F, Villalba R, Benavente MC, Gonzalez AI. In vitro susceptibility of Mycobacterium fortuitum, Mycobacterium chelonae and Mycobacterium avium against some quinolones. Chemioterapia 6: 431–433, 1987
Chapman ST, Speller DCE, Reeves DS. Resistance to ciprofloxacin. Lancet 2: 39, 1985
Chau PY, Leung YK, Ng WS. Comparative in vitro antibacterial activity of ofloxacin and ciprofloxacin against some selected Gram-positive and Gram-negative isolates. Infection 14(Suppl. 4): 237–239, 1986
Chin NX, Jules K, Neu HC. Synergy of ciprofloxacin and azlocillin in vitro and in a neutropenic mouse model of infection. European Journal of Clinical Microbiology 5: 23–28, 1986
Chin N-X, Neu HC. Ciprofloxacin, a quinolone carboxylic acid compound active against aerobic and anaerobic bacteria. Antimicrobial Agents and Chemotherapy 25: 319–326, 1984
Chin N-X, Neu HC. Post-antibiotic suppressive effect of ciprofloxacin against Gram-positive and Gram-negative bacteria. American Journal of Medicine 82: 58–62, 1987a
Chin N-X, Neu HC. Synergy of imipenem — a novel carbapenem, and rifampin and ciprofloxacin against Pseudomonas aeruginosa, Serratia marcescens and Enterobacter species. Chemotherapy 33: 183–188, 1987b
Chow AW, Cheng N, Bartlett KH. In vitro susceptibility of Clostridium difficile to new β-lactam and quinolone antibiotics. Antimicrobial Agents and Chemotherapy 28: 842–844, 1985
Cohen J, McConnell JS. Antibiotic-induced endotoxin release. Lancet 2: 1069–1070, 1985
Cohen J, McConnell JS. Release of endotoxin from bacteria exposed to ciprofloxacin and its prevention with polymyxin B. European Journal of Clinical Microbiology 5: 13–17, 1986
Collins CH, Uttley HC. In-vitro susceptibility of mycobacteria to ciprofloxacin. Journal of Antimicrobial Chemotherapy 16: 575–580, 1985
Collins MS, Hector RF, Roby RE, Edwards AA, Ladehoff DK, Dorsey JH. Prophylaxis of gram-negative and gram-positive infections in rodents with 3 intravenous immunoglobulins and therapy of experimental polymicrobial burn wound sepsis with pseudomonas immunoglobulin and ciprofloxacin. Infection 15(Suppl. 2): 51–59, 1987
Connolly MJ, Snow MH, Ingham HR. Ciprofloxacin treatment of recurrent Salmonella typhimurium septicaemia in a patient with acquired immune deficiency syndrome. Journal of Antimicrobial Chemotherapy 18: 647–648, 1986
Cornaglia G, Pompei R, Dainelli B, Satta G. In vitro activity of ciprofloxacin against aerobic bacterial isolated in a Southern European hospital. Antimicrobial Agents and Chemotherapy 31: 1651–1655, 1987
Courvalin P, Derlot E, Chabbert YA. Cross resistance to quinolone derivatives of Enterobacteriaceae and Pseudomonas mutants selected on pefloxacin and ciprofloxacin. Abstract 401 presented at the 24th Interscience Conference on Antimicrobial Agents and Chemotherapy, Washington, USA, 1984
Cox CE. Comparative study of three dosage regimens of ciprofloxacin in the treatment of urinary tract infections. In Neu HC & Weuta H (Eds) 1st International Ciprofloxacin Workshop, Leverkusen, 1985, pp. 291–296, Excerpta Medica, Amsterdam, 1986
Cox C. Brief report: ciprofloxacin in the treatment of urinary tract infections caused by Pseudomonas species and organisms resistant to trimethoprim/sulfamethoxazole. American Journal of Medicine 82(Suppl. 4A): 228–229, 1987
Crook SM, Selkon JB, McLardy Smith PD. Clinical resistance to long-term oral ciprofloxacin. Lancet 1: 1275, 1985
Cullmann W, Stieglitz M, Baars B, Opferkuch W. Comparative evaluation of recently developed quinolone compounds — with a note on the frequency of resistant mutants. Chemotherapy 31: 19–28, 1985
Dan M, Verbin N, Gorea A, Nagar H, Berger SA. Concentrations of ciprofloxacin in human liver, gallbladder and bile after oral administration. European Journal of Clinical Pharmacology 32: 217–218, 1987
Daschner FD, Westenfelder M, Dalhoff A. Penetration of ciprofloxacin into kidney, fat, muscle and skin tissue. European Journal of Clinical Microbiology 5: 212–213, 1986
Davies BI, Maesen FPV. Respiratory infections: clinical experiences with the new quinolones. Pharmaceutisch Weekblad Scientific Edition 9 (Suppl.): 53–57, 1987
Davies GSR, Cohen J. In-vitro study of the activity of ciprofloxacin alone and in combination against strains of Pseudomonas aeruginosa with multiple antibiotic resistance. Journal of Antimicrobial Chemotherapy 16: 713–717, 1985
Davies S, Sparham PD, Spencer RC. Comparative in-vitro activity of five fluoroquinolones against mycobacteria. Journal of Antimicrobial Chemotherapy 19: 605–609, 1987
Davis RL, Koup JR, Williams-Warren J, Weber A, Heggen L, et al. Pharmacokinetics of ciprofloxacin in cystic fibrosis. Antimicrobial Agents and Chemotherapy 31: 915–919, 1987
De Lalla F, Rizzardini G, Angelucci B. Oral ciprofloxacin in the treatment of uncomplicated gonococcal urethritis in men. Chemioterapia 6: 50–51, 1987
Dekker AW, Rozenberg-Arska M, Verhoeff J. Infection prophylaxis in acute leukemia: a comparison of ciprofloxacin with trimethoprim-sulfamethoxazole and colistin. Annals of Internal Medicine 106: 7–12, 1987
Delfino D, Bonina L, Berlinghieri MC, Mastroeni P. Effects of a new quinolone derivative, ciprofloxacin, on some professional phagocytic cell functions. Chemioterapia 4: 463–466, 1985
Delmee M, Avesani V. Comparative in vitro activity of seven quinolones against 100 clinical isolates of Clostridium difficile. Antimicrobial Agents and Chemotherapy 29: 374–375, 1986
Dennig D, Fülle H, Hellriegel KP. Chemoprophylaxis of bacterial infections in granulocytopenic patients with ciprofloxacin. Onkologie 10: 57–58, 1987
De Vries-Hospers HG, Welling GW, Van der Waaij D. Influence of quinolones on throat- and faecal flora of healthy volunteers. Pharmaceutisch Weekblad Scientific Edition 9 (Suppl.): 41–44, 1987
De Witte T, Novakova I, Branolte J, Muytjens H, De Pauw B. Long-term oral ciprofloxacin for infection prophylaxis in allogenic bone marrow transplantation. Pharmaceutisch Weekblad Scientific Edition 9 (Suppl.): 48–50, 1987
Digranes A, Dibb WL, Benonisen E. In vitro activities of ciprofloxacin, ofloxacin, norfloxacin and rosoxacin compared with cinoxacin and trimethoprim. Chemotherapy 31: 466–471, 1985
Digranes A. In vitro activity of amifloxacin (WIN 49 375) compared with those of ciprofloxacin and ofloxacin. Acta Pathologica, Microbiologica et Immunologica Scandinavica section B 95: 29–32, 1987
Diridl G, Pichler H, Wolf D. Treatment of chronic salmonella carriers with ciprofloxacin. European Journal of Clinical Microbiology 5: 260–261, 1986
Dirksen MSC, Vree TB. Pharmacokinetics of intravenously administered ciprofloxacin in intensive care patients with acute renal failure. Pharmaceutisch Weekblad — Scientific Edition 8: 35–39, 1986
Domagala JM, Hanna LD, Heifetz CL, Hutt MP, Mich TF, et al. New structure-activity relationships of the quinolone antibacterials using the target enzyme: the development and application of a DNA gyrase assay. Journal of Medicinal Chemistry 29: 394–404, 1986
Drusano GL. An overview of the pharmacology of intravenously administered ciprofloxacin. American Journal of Medicine 82(Suppl. 4A): 339–345, 1987
Drusano GL, Plaisance KI, Forrest A, Standiford HC. Dose ranging study and constant infusion evaluation of ciprofloxacin. Antimicrobial Agents and Chemotherapy 30: 440–443, 1986a
Drusano GL, Standiford HC, Plaisance K, Forrest A, Leslie J, et al. Absolute oral bioavailability of ciprofloxacin. Antimicrobial Agents and Chemotherapy 30: 444–446, 1986b
Drusano GL, Weir M, Forrest A, Plaisance K, Emm T, et al. Pharmacokinetics of intravenously administered ciprofloxacin in patients with various degrees of renal function. Antimicrobial Agents and Chemotherapy 31: 860–864, 1987
Dudley MN, Ericson J, Zinner SH. Effect of dose on serum pharmacokinetics of intravenous ciprofloxcin with identification and characterization of extravascular compartments using noncompartmental and compartmental pharmacokinetic models. Antimicrobial Agents and Chemotherapy 31: 1782–1786, 1987
Duncker D, Ullmann U. Influence of various antimicrobial agents on the chemiluminescence of phagocytosing human granulocytes. Chemotherapy 32: 18–24, 1986
Easmon CSF, Blowers A. Ciprofloxacin treatment of systemic infection in sensitive and resistant mice. Journal of Antimicrobial Chemotherapy 16: 615–519, 1985
Easmon CSF, Crane JP, Blowers A. Effect of ciprofloxacin on intracellular organisms: in-vitro and in-vivo studies. Journal of Antimicrobial Chemotherapy 18(Suppl. D): 43–48, 1986
Easmon CSF, Crane JP. Uptake of ciprofloxacin by human neutrophils. Journal of Antimicrobial Chemotherapy 16: 67–73, 1985
Easmon CSF. Protective effects of ciprofloxacin in a murine model of salmonella infection. American Journal of Medicine 82(Suppl. 4A): 71–72, 1987
Edlund C, Nord EC. Comparative in vitro activities of ciprofloxacin, enoxacin, norfloxacin, ofloxacin and pefloxacin against Bacteroides fragilis and Clostridium difficile. Scandinavian Journal of Infectious Diseases 18: 149–151, 1986
Efstratiou E, Sahin A, Giamarellou H. In vitro studies with BAY o 9867 a nalidixic acid analogue. Proceedings of the 13th International Congress of Chemotherapy, Vienna, part 112, pp. 9–12, 1983
Eliopoulos GM, Gardella A, Moellering RC. In vitro activity of ciprofloxacin, a new carboxyquinolone antimicrobial agent. Antimicrobial Agents and Chemotherapy 25: 331–335, 1984
Ericsson CD, Johnson PC, Dupont HL, Morgan DR, Bittsra JAM, et al. Ciprofloxacin or trimethoprim-sulphamethoxazole, as initial therapy for travelers’ diarrhea. Annals of Internal Medicine 106: 216–220, 1987
Eron LJ, Harvey L, Hixon DL, Poretz DM. Ciprofloxacin therapy of infections caused by Pseudomonas aeruginosa and other resistant bacteria. Antimicrobial Agents and Chemotherapy 27: 308–310, 1985
Escalante A, Aznar J, De Miguel C, Perea EJ. Activity of nine antimicrobial agents against Mycoplasma hominis and Urea-plasma urealyticum. European Journal of Sexually Transmitted Diseases 2: 85–87, 1985
Esposito S, Galante D, Barba D, D’errico G, Mazzone A, et al. Ciprofloxacin concentrations in human fluids and tissues following a single oral dose. International Journal of Pharmaceutical Research V11: 181–186, 1987a
Esposito S, Gupta A, Thadepalli H. In vitro synergy of ciprofloxacin and three other antibiotics against Bacteroides fragilis. Drugs Under Experimental and Clinical Research 8: 489–492, 1987b
Eykyn SJ, Williams H. Treatment of multiresistant Salmonella typhi with oral ciprofloxacin. Lancet 2: 1407–1408, 1987
Fass RJ. Efficacy and safety of oral ciprofloxacin for treatment of serious urinary tract infections. Antimicrobial Agents and Chemotherapy 31: 148–150, 1987a
Fass RJ. Efficacy and safety of oral ciprofloxacin in the treatment of serious respiratory infections. American Journal of Medicine 82(Suppl. 4A): 202–207, 1987b
Fass RJ. Treatment of skin and soft tissue infections with oral ciprofloxacin. Journal of Antimicrobial Chemotherapy 18(Suppl. D): 153–157, 1986
Fass RJ. In vitro activity of ciprofloxacin (Bay o 9867). Antimicrobial Agents and Chemotherapy 24: 568–574, 1983
Feist H, Vetter N, Drlicek M, Otupa I, Weuta H. Comparative study of ciprofloxacin and cefalexin in the treatment of patients with lower respiratory tract infections. In Neu HC & Weuta H (Eds) Proceedings of the 1st International Ciprofloxacin Workshop, Leverkusen, 1985, pp. 265–267, Excerpta Medica, Amsterdam 1986
Felmingham D, O’Hare MD, Robbins MJ, Wall RA, Williams AH, et al. Comparative in vitro studies with 4-quinolone antimicrobials. Drugs in Experimental Clinical Research 11: 317–329, 1985
Fenlon CH, Cynamon MH. Comparative in vitro activities of ciprofloxacin and other 4-quinolones against Mycobacterium tuberculosis and Mycobacterium intracellulare. Antimicrobial Agents and Chemotherapy 29: 386–388, 1986
Fern AI, Sweeney G, Doig M, Lindsay G. Penetration of ciprofloxacin into aqueous humor. Transactions of the Ophthalmological societies of the United Kingdom 105: 650–652, 1986
Fernandez-Guerrero ML, Rouse MS, Henry NK, Wilson WR. Ciprofloxacin treatment of methicillin-sensitive or methicillin-resistant Staphylococcus aureus experimental endocarditis. 14th International Congress of Chemotherapy, abstract no. 32–39, Kyoto, Japan, 1985
Fernández-Roblas R, Prieto S, Santamaría M, Ponte C, Soriano F. Activity of nine antimicrobial agents against Corynebacterium Group D2 strains isolated from clinical specimens and skin. Antimicrobial Agents and Chemotherapy 31: 821–822, 1987
Fietta A, Sacchi F, Bersani C, Grassi F, Mangiarotti P, et al. Effect of β-lactam antibiotics on migration and bactericidal activity of human phagocytes. Antimicrobial Agents and Chemotherapy 23: 930–931, 1983
Fitzgeorge RB, Gibson DH, Jepras R, Baskerville A. Studies on ciprofloxacin therapy of experimental Legionnaires’ disease. Journal of Infection 10: 194–203, 1985
Fleming LW, Moreland TA, Scott AC, Stewart WK, White LO. Ciprofloxacin in plasma and peritoneal dialysate after oral therapy in patients on continuous ambulatory peritoneal dialysis. Journal of Antimicrobial Chemotherapy 19: 493–503, 1987
Fliegelman RM, Petrak RM, Goodman LJ, Segreti J, Trenholme GM, et al. Comparative in vitro activities of twelve antimicrobial agents against Campylobacter species. Antimicrobial Agents and Chemotherapy 27: 429–430, 1985
Floyd-Reising SA, Kelley SG, Hindier JA, Young LS. In vitro activity of CI-934 compared with ciprofloxacin, enoxacin, norfloxacin, and vancomycin. Diagnostic Microbiology and Infectious Disease 6: 301–306, 1987
Follath F, Bindschedler M, Wenk M, Frei R, Stalder H, et al. Use of ciprofloxacin in the treatment of Pseudomonas aeruginosa infections. European Journal of Clinical Microbiology 5: 236–240, 1986
Fong IG, Ledbetter WH, Van den broucke C, Simbul M, Rahm V. Ciprofloxacin concentrations in bone and muscle after oral dosing. Antimicrobial Agents and Chemotherapy 29: 405–408, 1986
Fong IW, Linton W, Simbul M, Thorup R, McLaughlin B, et al. Treatment of nongonococcal urethritis with ciprofloxacin. American Journal of Medicine 82(Suppl. 4A): 311–316, 1987
Forsgren A, Bergkvist PI. Effect of ciprofloxacin on phagocytosis. European Journal of Clinical Microbiology 4: 575–578, 1985
Forsgren A, Bredberg A, Pardee AB, Schlossman SF, Tedder TF. Effects of ciprofloxacin on eucaryotic pyrimidine nucleotide biosynthesis and cell growth. Antimicrobial Agents and Chemotherapy 31: 774–779, 1987a
Forsgren A. Comparative in vitro activity of three new quinolone antibiotics against recent clinical isolates. Scandinavian Journal of Infectious Diseases 17: 91–94, 1985
Forsgren A, Schlossman SF, Tedder TF. 4-quinolone drugs affect cell cycle progression and function of human lymphocytes in vitro. Antimicrobial Agents and Chemotherapy 31: 768–773, 1987b
Forsgren A, Schmeling D, Quie PG. Effect of tetracycline on the phagocytic function of human leucocytes. Journal of Infectious Diseases 130: 412–415, 1974
Fu KP, Vince T, Bloom R, Gregory FJ, Hung PP. Therapeutic efficacy and pharmacokinetic properties of ciprofloxacin in intra-abdominal abscesses caused by Bacteroides fragilis and Escherichia coli. Drugs Under Experimental and Clinical Research 8: 493–496, 1987
Fuursted K. Post-antibiotic effect and killing activity of ciprofloxacin against Staphylococcus aureus. Acta Pathologica Microbiologica et Immunologica Scandinavica Section B — Microbiology 95: 199–202, 1987
Garlando F, Rietiker S, Täuber MG, Flepp M, Meier B, et al. Single-dose ciprofloxacin at 100 versus 250mg for treatment of uncomplicated urinary tract infections in women. Antimicrobial Agents and Chemotherapy 31: 354–356, 1987
Garlando F, Täuber MG, Joos B, Oelz O, Liithy R. Ciprofloxacin-induced hematuria. Infection 13: 177–178, 1985
Gasser TC, Ebert SC, Graversen PH, Madsen PO. Ciprofloxacin pharmacokinetics with normal and impaired renal function. Antimicrobial Agents and Chemotherapy 31: 709–712, 1987a
Gasser TC, Graversen PH, Madsen PO. Treatment of complicated urinary tract infections with ciprofloxacin. American Journal of Medicine 82(Suppl. 4A): 278–279, 1987b
Gau W, Kurz J, Petersen U, Ploschke HJ, Wuensche C. Isolation and structural elucidation of urinary metabolites of ciprofloxacin. Arzneimittel-Forschung 36: 1545–1549, 1986
Gay JD, DeYoung DR, Roberts GD. In vitro activities of norfloxacin and ciprofloxacin against Mycobacterium tuberculosis, M. avium complex, M. chelonei, M. fortuitum, and M. ransasii. Antimicrobial Agents and Chemotherapy 26: 94–96, 1984
Gellermann H-J. Therapy of lower respiratory tract infections with ciprofloxacin [Therapie von unteren atemwegsinfektionen mit ciprofloxacin]. Medizinische Welt 38: 69–72, 1987
Giamarellou H, Daphnis E, Galanakis N, Dendrinos Ch, Petrikkos G, et al. Ciprofloxacin in the treatment of Gram-negative infections including Pseudomonas aeruginosa. Proceedings of the 14th International Congress of Chemotherapy Kyoto, Japan, Jun, 1985
Giamarellou H, Galanakis N. Use of intravenous ciprofloxacin in difficult-to-treat infections. American Journal of Medicine 82(Suppl. 4A): 346–351, 1987
Giamarellou H, Galanakis N, Dendrinos C, Stefanou J, Daphnis E, et al. Evaluation of ciprofloxacin in the treatment of Pseudomonas aeruginosa infections. European Journal of Clinical Microbiology 5: 232–235, 1986
Giamarellou H, Petrikkos G. Ciprofloxacin interactions with imipenem and amikacin against multiresistant Pseudomonas aeruginosa. Antimicrobial Agents and Chemotherapy 31: 959–961, 1987
Gilbert DN, Tice AD, Marsh PK, Craven PC, Preheim LC. Oral ciprofloxacin therapy for chronic contiguous osteomyelitis caused by aerobic Gram-negative bacilli. American Journal of Medicine 82(Suppl. 4A): 254–258, 1987
Gleadhill IC, Ferguson WP, Lowry RC. Efficacy and safety of ciprofloxacin in patients with respiratory tract infections in comparison with amoxycillin. Journal of Antimicrobial Chemotherapy 18(Suppl. D): 133–138, 1986
Gobernado M, Cantón E, Santos M. In vitro activity of ciprofloxacin against Bruceila melitensis. European Journal of Clinical Microbiology 3: 371, 1984
Goldfarb J, Stern RC, Reed MD, Yamashita TS, Myers CM, et al. Ciprofloxacin monotherapy for acute pulmonary exacerbations of cystic fibrosis. American Journal of Medicine 82(Suppl. 4A): 174–179, 1987
Goldfarb J, Wormser GP, Inchiosa MA, Guideri G, Diaz M, et al. Single dose pharmacokinetics of oral ciprofloxacin in patients with cystic fibrosis. Journal of Clinical Pharmacology 26: 222–226, 1986
Goldstein EJC, Kahn RM, Alpert ML, Ginsberg BP, Greenway FI, et al. Ciprofloxacin versus cinoxacin in therapy of urinary tract infections. American Journal of Medicine 82(Suppl. 4A): 284–287, 1987
Gollapudi SVS, Prabhala RH, Thadepalli H. Effect of ciprofloxacin on mitogen-stimulated lymphocyte proliferation. Antimicrobial Agents and Chemotherapy 29: 337–338, 1986
Golper TA, Hortsfein AI, Morthland VH, Christensen JM. Effects of antacids and dialysate dwell times on multiple dose pharmacokinetics of oral ciprofloxacin in patients on continuous ambulatory peritoneal dialysis. Antimicrobial Agents and Chemotherapy 31: 1787–1790, 1987
Gombert ME, Aulicino TM. Comparison of agar dilution, microtitre broth dilution and tube macrodilution susceptibility testing of ciprofloxacin against several pathogens at two different inocula. Journal of Antimicrobial Chemotherapy 16: 709–712, 1985
Gombert ME, Aulicino TM. Susceptibility of multiply antibiotic-resistant pneumococci to the new quinolone antibiotics, nalidixic acid, coumermycin, and novobiocin. Antimicrobial Agents and Chemotherapy 26: 933–934, 1984
Gonzalez MA, Moranchel AH, Duran S, Pichardo A, Magana JL, et al. Multiple dose ciprofloxacin dose ranging and kinetics. Clinical Pharmacology and Therapeutics 37: 633–637, 1985a
Gonzalez MA, Moranchel AH, Duran S, Pichardo A, Magana JL. Multiple dose pharmacokinetics of ciprofloxacin administered intravenously to normal volunteers. Antimicrobial Agents and Chemotherapy 28: 235–239, 1985b
Goormans E, Dalhoff A, Kazzaz B, Branolte J. Penetration of ciprofloxacin into gynecological tissues following oral and intravenous administration. Chemotherapy 32: 7–77, 1986
Goosens H, De Mol P, Coignau H, Levy J, Grados O, et al. Comparative in vitro activities of aztreonam, ciprofloxacin, norfloxacin, ofloxacin, HR 810 (a new cephalosporin), RU 28965 (a new macrolide), and other agents against enteropathogens. Antimicrobial Agents and Chemotherapy 27: 388–392, 1985
Gordin PM, Hackbarth CJ, Scott KG, Sande MA. Activities of pefloxacin and ciprofloxacin in experimentally induced Pseudomonas pneumonia in neutropenic guinea-pigs. Antimicrobial Agents and Chemotherapy 27: 452–454, 1985
Grabe M, Forsgren A, Björk T, Hellsen S. Controlled trial of a short and a prolonged course with ciprofloxacin in patients undergoing transurethral prostatic surgery. European Journal of Clinical Microbiology 6: 11–17, 1987
Graeff H, Loos W, Hugo RV, Machka K, Fischbach F. Ciprofloxacin in the treatment of patients with symptomatic and asymptomatic urinary tract infections: a comparative study of single dose application versus three days’ treatment concerning efficacy and safety (Abstract S-50-9) Proceedings of the 14th International Congress of Chemotherapy, Kyoto, Japan, Jun, 1985
Greenberg RN, Kennedy DJ, Reilly PM, Luppen KL, Weinandt WJ, et al. Treatment of bone, joint, and soft-tissue infections with oral ciprofloxacin. Antimicrobial Agents and Chemotherapy 31: 151–155, 1987a
Greenberg RN, Tice AD, Marsh PK, Craven PC, Reilly PM, et al. Randomized trial of ciprofloxacin compared with other antimicrobial therapy in the treatment of osteomyelitis. American Journal of Medicine 82(Suppl. 4A): 266–269, 1987b
Guay DRP, Awni WM, Peterson PK, Obaid S, Breitenbucher R, et al. Pharmacokinetics of ciprofloxacin in acutely ill and convalescent elderly patients. American Journal of Medicine 82(Suppl. 14A): 124–129, 1987
Guay D, Klicker R, Pence T, Peterson P. In vitro antistaphylococcal activity of teicoplanin and ciprofloxacin in peritoneal dialysis effluent. European Journal of Clinical Microbiology 5: 661–663, 1986
Guelpa-Lauras C-C, Perani EG, Giroir A-M, Grosset JH. Activities of pefloxacin and ciprofloxacin against Mycobacterium leprae in the mouse. International Journal of Leprosy 55: 70–77, 1987
Hackbarth CJ, Chambers HF, Stella F, Shibl AM, Sande MA. Ciprofloxacin in experimental Pseudomonas aeruginosa meningitis in rabbits. Journal of Antimicrobial Chemotherapy 18(Suppl. D): 65–69, 1986
Haller I. Comprehensive evaluation of ciprofloxacin — aminoglycoside combinations against Enterobacteriaceae and Pseudomonas aeruginosa strains. Antimicrobial Agents and Chemotherapy 28: 663–666, 1985
Hara H, Saito A, Yamaguchi K, Suzuyama Y, Shigeno Y, Kohno S, et al. Comparative study of Bay 09867 (ciprofloxacin) and bacampicillin on bacterial pneumonia by double blind method. Chemotherapy (Tokyo) 34: 629–653, 1986
Hart CA, How SJ, Hobson D. Activity of ciprofloxacin against genital tract pathogens. British Journal of Venereal Diseases 60: 316–318, 1984
Haverkorn MJ. Ciprofloxacin for respiratory tract infection with Pseudomonas aeruginosa. Pharmaceutisch Weekblad Scientific Edition 9 (Suppl.): 64–67, 1987
Heise-Reinecker E, Ruschmeyer J, Rosenfeld M. Clinical efficacy of ciprofloxacin in Salmonella carriers. In Neu HC & Weuta H (Eds) 1st International Ciprofloxacin Workshop, Leverkusen, 1985, pp. 373–377, Excerpta Medica, Amsterdam, 1986
Henry NK, Rouse MS, Whitesell AL, McConnell ME, Wilson WR. Treatment of methicillin-resistant staphylococcus aureus experimental osteomyelitis with ciprofloxacin or vancomycin alone or in combination with rifampin. American Journal of Medicine 82: 73–75, 1987
Henry NK, Schultz HJ, Grubbs NC, Muller SM, Ilstup DM, et al. Comparison of ciprofloxacin and co-trimoxazole in the treatment of uncomplicated urinary tract infection in women. Journal of Antimicrobial Chemotherapy 18(Suppl. D): 103–106, 1986
Hodson ME, Roberts CM, Butland RJA, Smith MJ, Batten JC. Oral ciprofloxacin compared with conventional intravenous treatment for Pseudomonas aeruginosa infection in adults with cystic fibrosis. Lancet 1: 235–237, 1987
Hof H, Pfannemüller B, Christen A. Therapeutic activities of ciprofloxacin on infection of mice with Listeria monocytogenes, Salmonella typhimurium, Escherichia coli and Pseudomonas aeruginosa. 2nd European Congress of Clinical Microbiology, abstract no. 22/17, Brighton, England, 1985
Höffken G, Borner K, Glatzel PD, Koeppe P, Lode H. Reduced enterai absorption of ciprofloxacin in the presence of antacids. European Journal of Clinical Microbiology 4: 345, 1985a
Höffken G, Lode H, Prinzing C, Borner K, Koeppe P. Pharmacokinetics of ciprofloxacin after oral and parenteral administration. Antimicrobial Agents and Chemotherapy 27: 375–379, 1985b
Höffken G, Lode H, Willey PD. Pharmacokinetics and interaction in the bioavailability of new quinolones. Abstract from Proceedings of the International Symposium on the New Quinolones, Geneva, 1986
Höffler U. In-vitro sensitivity of Bacteroidaceae, clostridia and propionibacteria to newer antimicrobial agents. Journal of Antimicrobial Chemotherapy 18(Suppl. E): 41–46, 1986
Hoiby N. Clinical use of nalidixic acid analogues: the fluoroquinolones. European Journal of Clinical Microbiology 5: 138–140, 1986
Holmes B, Brogden RN, Richards DM. Norfloxacin: a review of its antibacterial activity, pharmacokinetic properties and therapeutic use. Drugs 30: 482–513, 1985
Holt HA, Lewis DA, White LO, Bastable SY, Reeves DS. Effect of oral ciprofloxacin on the faecal flora of healthy volunteers. European Journal of Clinical Microbiology 5: 201–205, 1986
Honeybourne D, Wise R, Andrews JM. Ciprofloxacin penetration into lungs. Lancet 2031: 1040, 1987
Hoogkamp-Korstanje JAA. Comparative in vitro activity of five quinolone derivatives and five other antimicrobial agents used in oral therapy. European Journal of Clinical Microbiology 3: 333–338, 1984
Hoogkamp-Korstanje JAA. Treatment of chronic postsurgical osteomyelitis with ciprofloxacin. Pharmaceutisch Weekblad Scientific Edition 9 (Suppl.): 90–92, 1987
Hooper DC, Wolfson JS, Ng EY, Swartz MN. Mechanisms of action of and resistance to ciprofloxacin. American Journal of Medicine 82(Suppl. 4A): 12–20, 1987
Houwen RHJ, Bijleveld CMA, DeVries-Hospers HG. Ciprofloxacin for cholangitis after hepatic portoenterostomy. Lancet 1: 1367, 1987
Hudson SJ, Ingham HR, Snow MH. Treatment of Salmonella typhi carrier state with ciprofloxacin. Lancet 1: 1047, 1985
Humphreys H, Mulvihill E. Ciprofloxacin-resistant Staphylococcus aureus: Lancet 1: 383, 1985
Iannello D, Delfino D, Carbone M, Fera M, Curo TF. In vitro effects of cephalosporin and ampicillin on some human leukocyte functions. Drugs in Experimental and Clinical Research 9: 67–71, 1983
Isaacs D, Slack MPE, Wilkinson AR, Westwood AW. Successful treatment of pseudomonal ventriculitis with ciprofloxacin. Journal of Antimicrobial Chemotherapy 17: 535–538, 1986
Janknegt R. Fluorinated quinolones: a review of their mode of action, antimicrobial activity, pharmacokinetics and clinical efficacy. Pharmaceutisch Weekblad — Scientific Edition 8: 1–21, 1986
Jensen T, Pedersen SS, Neilsen CH, Høiby N, Koch C. Efficacy and safety of ciprofloxacin and ofloxacin in chronic Pseudomonas aeruginosa infection in cystic fibrosis. Journal of Antimicrobial Chemotherapy 20: 585–594, 1987
Joly-Guillou ML, Bergogne-Berezin E. In vitro activity of antimicrobial agents against Acinetobacter calcoaceticus. Drugs in Experimental Clinical Research 12: 949–952, 1986
Joos B, Ledergerber B, Flepp M, Betex JD, Liithy R, et al. Comparison of high liquid chromatography and bioassay for determination of ciprofloxacin in serum and urine. Antimicrobial Agents and Chemotherapy 27: 353–356, 1985
Jules K, Neu HC. The efficacy of fluorinated carboxyquinolones in protecting neutropenic mice from Pseudomonas aeruginosa. 24th Interscience Conference on Antimicrobial Agents and Chemotherapy, p. 94, Washington D.C., USA, 1984
Kaatz GW, Barriere SL, Schaberg DR, Fekety R. Emergence of resistance to ciprofloxacin during experimental Staphylococcus aureus endocarditis. Journal of Antimicrobial Chemotherapy 20: 753–758, 1987b
Kaatz GW, Barriere SL, Schaberg DR, Fekety R. Ciprofloxacin versus vancomycin in the therapy of experimental methicillin-resistant Staphylococcus aureus endocarditis. Antimicrobial Agents and Chemotherapy 31: 527–530, 1987a
Kamidono S, Arakawa S. Brief report: ciprofloxacin treatment of complicated urinary tract infections. American Journal of Medicine 82(Suppl. 4A): 301–302, 1987
Kawamura S, Itabashi T, Watanabe H, Fujimaki Y, Horikawa H, et al. Comparative study of ciprofloxacin (Bay o 9867) and pipemidic acid in the treatment of suppurative otitis media. JIBI. (Ear and Nose) 33: 100–125, 1987
Kayser FM. The quinolones: mode of action and mechanism of resistance. Research and Clinical Forums 7: 17–27, 1985
Kelley SG, Bertram MA, Young LS. Activity of ciprofloxacin against resistant clinical isolates. Journal of Antimicrobial Chemotherapy 17: 281–286, 1986
Kemmerich B, Borner K, Pennington JE. Comparative efficacies of ciprofloxacin, ampicillin and chloramphenicol in treatment of experimental Haemophilus influenzae pneumonia. Journal of Antimicrobial Chemotherapy 20: 77–83, 1987
Kemmerich B, Small GJ, Pennington JE. Comparative evaluation of ciprofloxacin, enoxacin and ofloxacin in experimental Pseudomonas aeruginosa pneumonia. Antimicrobial Agents and Chemotherapy 29: 395–399, 1986
Kiess W, Haas R, Marget W. Chloramphenicol-resistant Salmonella tennesse osteomyelitis. Correspondence. Infection 12: 359, 1984
King A, Phillips I. The comparative in vitro activity of eight newer quinolones and nalidixic acid. Journal of Antimicrobial Chemotherapy 18(Suppl. D): 1–20, 1986
Klein E, Trautmann M, Hoffmann H-G. Ciprofloxacin in Salmonella infection and abdominal typhoid. Deutsche Medizinische Wochenschrift 111: 1599–1602, 1986
Klietmann W, Focht J, Nösner K. Comparative in vitro activity of ciprofloxacin against aerobic and anaerobic bacteria from clinical isolates. Arzneimittel-Forschung 37: 661–666, 1987
Knoche H, Glogau U, Enzensberger R, Schäfer V, Kipp JP, et al. Effect of oral ofloxacin on bowel flora in human volunteers. (Abstract S 2/2) 2nd European Congress of Clinical Microbiology, Brighton, 1985
Kobayashi H. Clinical efficacy of ciprofloxacin in the treatment of patients with respiratory tract infections in Japan. American Journal of Medicine 82: 169–173, 1987
Kobayashi H. Summary of clinical studies on ciprofloxacin: efficacy and adverse reactions. Proceedings of the 14th International Congress of Chemotherapy, Kyoto, Japan, Jun, 1985
Kobayashi H, Takamura H, Takeda H, Kono K, Saito A, et al. Comparative clinical study of ciprofloxacin and cefaclor in the treatment of respiratory tract infections. Chemotherapy (Tokyo) 34: 1011–1037, 1986
Kosmidis J, Macrygiannis E, Aboudabash B. Ciprofloxacin in urinary tract infections: its efficacy as compared with that of co-trimoxazole. In Neu HC & Weuta H (Eds) 1st International Ciprofloxacin Workshop, Leverkusen, 1985, pp. 310–313, Excerpta Medica, Amsterdam, 1986
Krol GJ, Noe AJ, Beerman D. Liquid Chromatographic analysis of ciprofloxacin and ciprofloxacin metabolites in body fluids. Journal of Liquid Chromatography 9: 2897–2919, 1986
Kumazawa J. Clinical evaluation of the use of ciprofloxacin in urological infections. Presented at the 14th International Congress of Chemotherapy, Kyoto, 1985
Kumazawa J, Matsumoto T, Tsuchida S, Niijima T, Machida T, et al. Comparative clinical study of ciprofloxacin (Bay o 9867) and norfloxacin in the treatment of complicated urinary tract infections. Nishinihon Journal of Urology 49: 1620–1622, 1987
Kurz CC, Marget W, Harms K, Bertele RM. Crossover study on the efficacy of oral ofloxacin and ciprofloxacin. Infection 14(Suppl. 1): S82–S86, 1986
Lagast H, Husson M, Klastersky J. Bactericidal activity of ciprofloxacin in serum and urine against Escherichia coli, Pseudomonas aeruginosa, Klebsiella pneumoniae, Staphylococcus aureus and Streptococcus faecalis. Journal of Antimicrobial Chemotherapy 16: 341–347, 1985
LeBel M, Barbeau G, Bergeron MG, Roy D, Vallée F. Pharmacokinetics of ciprofloxacin in elderly subjects. Pharmacotherapy 6: 87–91, 1986a
LeBel M, Bergeron MG, Vallée F, Fiset C, Chassé G, et al. Pharmacokinetics and pharmacodynamics of ciprofloxacin in cystic fibrosis patients. Antimicrobial Agents and Chemotherapy 30: 260–266, 1986c
LeBel M, Vallée F, Bergeron MG. Tissue penetration of ciprofloxacin after single and multiple doses. Antimicrobial Agents and Chemotherapy 29: 501–505, 1986b
Ledergerber B, Bettex JD, Joos B, Flepp M, Luthy R. Effect of standard breakfast on drug absorption and multiple-dose pharmacokinetics of ciprofloxacin. Antimicrobial Agents and Chemotherapy 27: 350–352, 1985
Lefrock JL, Smith BR, Bihl-Donato J. Ciprofloxacin: a comparative study of in vitro antimicrobial activity. Current Therapeutic Research 39: 789–797, 1986
Leigh DA, Emmanuel FXS, Petch VJ. Ciprofloxacin therapy in complicated urinary tract infections caused by Pseudomonas aeruginosa and other resistant bacteria. Journal of Antimicrobial Chemotherapy 18(Suppl. D): 117–121, 1986
Lesse AJ, Freer C, Salata RA, Francis JB, Scheid WM. Oral ciprofloxacin therapy for Gram-negative bacillary osteomyelitis. American Journal of Medicine 82(Suppl. 4A): 247–253, 1987
Levison ME, Pitsakis PG, Rosenberg AF. Comparison of the efficacy of ciprofloxacin, BMY-28142 and ceftazidime in therapy of experimental Pseudomonas aeruginosa endocarditis in the rat. 14th International Congress on Chemotherapy, abstract no. S-32-8, Kyoto, Japan, 1985
Lewin CS, Smith JT. Detection of a third bacterial mechanism of ciprofloxacin and ofloxacin. Journal of Pharmacy and Pharmacology 38 (Suppl.): 44P, 1986
Licitra CM, Brooks RG, Siegler BE. Clinical efficacy and levels of ciprofloxacin in tissue in patients with soft tissue infection. Antimicrobial Agents and Chemotherapy 31: 805–807, 1987
Liebowitz LD, Saunders J, Fehler G, Ballard RC, Koornhof HJ. In vitro activity of A-56619 (difloxacin), A-56620, and other new quinolone antimicrobial agents against genital pathogens. Antimicrobial Agents and Chemotherapy 30: 948–950, 1986
Limson BM. Efficacy and safety of ciprofloxacin in uncomplicated typhoid fever. In Neu HC & Weuta H (Eds) 1st International Ciprofloxacin Workshop, Leverkusen 1985, pp. 362–364, Excerpta Medica, Amsterdam, 1986
Lode H, Wiley R, Höffken G, Wagner J, Borner K. Prospective randomized controlled study of ciprofloxacin versus imipenem-cilastatin in severe clinical infections. Antimicrobial Agents and Chemotherapy 31: 1491–1496, 1987
Lonka L, Pedersen RS. Ciprofloxacin for cholangitis. Lancet 2: 212, 1987
Loo PS, Ridgway GL, Oriel JD. Single dose ciprofloxacin for treating gonococcal infections in men. Genitourinary Medicine 61: 302–305, 1985
Luthy R, Joos B, Gassmann F. Penetration of ciprofloxacin into the human eye. In Neu HC & Weuta H (Eds) 1st International Ciprofloxacin Workshop, Leverkusen 1985, pp. 192–195, Excerpta Medica, Amsterdam 1986
Machka K, Milatovic D. Serum bactericidal activity of ciprofloxacin and ofloxacin in volunteers. European Journal of Clinical Microbiology 6: 59–62, 1987
Magnani C, Fregni S, Valli G, Cosentina R, Bisetti A. Comparative clinical study of ciprofloxacin and co-trimoxazole in respiratory tract infections. In Neu HC & Weuta H (Eds) 1st International Ciprofloxacin Workshop, Leverkusen, 1985, pp. 260–264, Excerpta Medica, Amsterdam, 1986
Manning M, Edison A, Gadebusch M. Inhibition of DNA gyrase by norfloxacin and ten other quinolone carboxylic acids. Abstract no. 979 presented at the 24th Interscience Conference on Antimicrobial Agents and Chemotherapy, Washington, USA, 8–10 Oct, 1984
Marinis E, Legakis NJ. In vitro activity of ciprofloxacin against clinical isolates of mycobacteria resistant to antimycobacterial drugs. Journal of Antimicrobial Chemotherapy 16: 527–530, 1985
McConnell JS, Cohen J. Release of endotoxin from Escherichia coli by quinolones. Journal of Antimicrobial Chemotherapy 18: 765–773, 1986
McCormick EM, Echols RM. Effect of peritoneal dialysis fluid and pH on bactericidal activity of ciprofloxacin. Antimicrobial Agents and Chemotherapy 31: 657–659, 1987
McNulty CAM, Dent J, Wise R. Susceptibility of clinical isolates of Campylobacter pyloridis to 11 antimicrobial agents. Antimicrobial Agents and Chemotherapy 28: 837–838, 1985
Mehtar S, Blakemore PH, Ellis K. Brief report: In vivo curing of plasmids from multi-drug-resistant Serratia marcescens by ciprofloxacin. American Journal of Medicine 82(Suppl. 4A): 55–57, 1987
Mehtar S, Drabu Y, Blakemore P. Ciprofloxacin in the treatment of infections caused by gentamicin-resistant Gram-negative bacteria. European Journal of Clinical Microbiology 5: 248–251, 1986
Michalsen H, Stiris T, Bergan T. Peroral ciprofloxacin in the treatment of infections with Pseudomonas aeruginosa in patients with CF. Abstract. Proceedings of the 13th Annual Meeting of the European Working Group for Cystic Fibrosis, Jerusalem, 3–8 Nov, 1985
Michéa-Hamzepour M, Auckenthaler R, Regamey P, Pechère J-C. Resistance occurring after fluoroquinolone therapy of experimental Pseudomonas aeruginosa peritonitis. Antimicrobial Agents and Chemotherapy 31: 1803–1808, 1987
Michel-Briand Y, Uccelli V, Laporte J-M, Plesiat P. Elimination of plasmids from Enterobacteriaceae by 4-quinolone derivatives. Journal of Antimicrobial Chemotherapy 18: 667–674, 1986
Millar MR, Bransby-Zachary MA, Tompkins DS, Hawkey PM, Gibson RM. Ciprofloxacin for Pseudomonas aeruginosa meningitis. Lancet 1: 1325, 1986
Monk JP, Campoli-Richards DM. Ofloxacin: a review of its antibacterial activity, pharmacokinetic properties and therapeutic use. Drugs 33: 346–391, 1987
Moody JA, Gerding DN, Peterson LR. Evaluation of ciprofloxacin’s synergism with other agents by multiple in vitro methods. American Journal of Medicine 82(Suppl. 4A): 44–54, 1987
Moorhouse EC, Mulvihill TE, Jones L, Mooney D, Falkiner FR, et al. The in-vitro activity of some antimicrobial agents against methicillin-resistant Staphylococcus aureus. Journal of Antimicrobial Chemotherapy 15: 291–295, 1985
Motohiro T, Aramaki M, Kawakami A, Tanaka K, Koga T, et al. Effect of BAY 0 9867 (Ciprofloxacin), a new quinolone antibacterial agent, on human fecal flora. Chemotherapy 33(S7): 100–139, 1985
Mulligan ME, Ruane PJ, Johnston L, Wong P, Wheelock JP, et al. Ciprofloxacin for eradication of methicillin-resistant Staphylococcus aureus colonization. American Journal of Medicine 82(Suppl. 4A): 215–219, 1987
Murdoch DA, Badenoch DF. Oral ciprofloxacin as prophylaxis for optical urethrectomy. British Journal of Urology 60: 352–354, 1987
Murdoch DA, Badenoch DF, Gatchalian ER. Oral ciprofloxacin prophylaxis in transurethral resection of the prostate. British Journal of Urology 60: 153–156, 1987
Murphy PG, Ferguson WP. Corynebacterium jeikeium (Group JK) resistance to ciprofloxacin emerging during therapy. Journal of Antimicrobial Chemotherapy 20: 922–923, 1987
Muszynski MJ, Scribner RK, Lewis TD, Marks MI. Activity of ciprofloxacin in combination with azlocillin against Pseudomonas aeruginosa. Abstract no. 1091 from the 25th Interscience Conference on Antimicrobial Agents and Chemotherapy, Minneapolis, USA, Sep 29–Oct 2, 1985a
Muszynski MJ, Scribner RK, Marks MI. In vitro activity of ciprofloxacin, in combination with other antimicrobials, against Pseudomonas aeruginosa isolates from patients with cystic fibrosis. Abstract no. A19 from American Society for Microbiology 85th Annual Meeting, Las Vegas, USA, March 3–7, 1985b
Muytjens HL, van der Ros-van de Repe J, van Veldhuizen G. Comparative activities of ciprofloxacin (Bay o 9867), norfloxacin, pipemidic acid, and nalidixic acid. Antimicrobial Agents and Chemotherapy 24: 302–304, 1983
Naamara W, Plummer FA, Greenblatt RM, D’Costa LJ, Ndinya-Achola LJ, et al. Treatment of chancroid with ciprofloxacin. American Journal of Medicine 82(Suppl. 4A): 317–320, 1987
Naber KG, Bartosik-Wich B. Ciprofloxacin versus norfloxacin in the treatment of complicated urinary tract infections: in vitro activity, serum and urine concentrations, safety and therapeutic efficacy. In Neu HC & Weuta H (Eds) 1st International Ciprofloxacin Workshop, Leverkusen 1985, pp. 314–317, Excerpta Medica, Amsterdam, 1986
NCCLS. Thornsberry C, et al. (Eds) Methods for dilution antimicrobial susceptibility tests for bacteria that grow aerobically: approved standard. National Committee for Clinical Laboratory Standards publication M7-A, Villanova Pa., NCCLS, 1985
Neu HC. Ciprofloxacin: an overview and prospective appraisal. American Journal of Medicine 82(Suppl. 4A): 395–404, 1987
Neu HC, Kumada T, Chin N-X, Mandell W. The post-antibiotic suppressive effect of quinolone agents. Drugs in Experimental Clinical Research 13: 63–67, 1987
Newsom SWB, Murphy P, Matthews J. A comparative study of ciprofloxacin and trimethoprim in the treatment of urinary tract infections in geriatric patients. Journal of Antimicrobial Chemotherapy 18(Suppl. D): 111–115, 1986
Nilsson-Ehle I. Assay for ciprofloxacin and norfloxacin in serum and urine by high performance liquid chromatography. Journal of Chromatography 416: 207–211, 1987
Nix DE, DeVito JM, Whitbread MA, Schentag JJ. Effect of multiple dose oral ciprofloxacin on the pharmacokinetics of theophylline and in docyanine green. Journal of Clinical Pharmacology 26: 545, 1986
Nix DE, Sands MF, Peloquin CA, Vari AJ, Cumbo TJ, et al. Dual individualization of intravenous ciprofloxacin in patients with nosocomial lower respiratory tract infections. American Journal of Medicine 82(Suppl. 4A): 352–356, 1987
Nord CE, Delin C, Bergan T, Johansen S, Kolstad IM, et al. The effect of ciprofloxacin on oropharyngeal and colon microflora. Research and Clinical Forum 7: 89–95, 1985
Norden CW, Shinners E. Ciprofloxacin as therapy for experimental osteomyelitis caused by Pseudomonas aeruginosa. Journal of Infectious Diseases 151: 291–294, 1985
Norden CW, Shinners E. Ciprofloxacin is effective therapy in Pseudomonas aeruginosa experimental osteomyelitis. 24th Interscience Conference on Antimicrobial Agents and Chemotherapy, abstract no. 273, Washington D.C., USA, 1984
Ogawa K, Tabuchi E, Hirota J, Haraguchi K, Ohyama M. Efficacy of ofloxacin and ciprofloxacin, new antimicrobial agents of pyridone carboxylic acid derivative, on experimental sinusitis. 14th International Congress on Chemotherapy, abstract no. S-48-11, Kyoto, Japan, 1985
Ooishi M, Sakaue F, Oomomo A, Yoneyama K. Fundamental and clinical studies on Bay 09867 in ophthalmology. Chemotherapy (Tokyo) 33: 1014–1021, 1985
Overbeek BP, Rozenberg-Arska M, Verhoef J. Interaction between ciprofloxacin and tobramycin or azlocillin against multi-resistant strains of Acinetobacter anitratum in vitro. European Journal of Clinical Microbiology 4: 140–141, 1985
Pankey GA, Valainis GT, Katner HP, Cortez LM, Dalovisio JR. Pseudomonas aeruginosa infections treated with ciprofloxacin. Abstract P-38-92 of the 14th International Congress of Chemotherapy, Kyoto, Japan, Jun, 1985
Parish LC, Asper R. Systemic treatment of cutaneous infections: a comparative study of ciprofloxacin and cefotaxime. American Journal of Medicine 82(Suppl. 4A): 227–229, 1987
Parras F, Ezpeleta C, Erice Al, Loza E, Martinez-Beltran J, et al. Evaluation of ciprofloxacin in the treatment of severe infections in non-neutropenic patients. Abstract P-38-93 of the 14th International Congress of Chemotherapy, Kyoto, Japan, Jun, 1985
Parry MF, Folta D, Nossek H, Anderson M, Azzarello L, et al. Comparative activity of ciprofloxacin and other new agents against 1454 clinical isolates at a community hospital. Current Therapeutic Research 38: 755–761, 1985
Parry MF. The in vitro activity and clinical role of ciprofloxacin: observations during treatment of patients with systemic and urinary tract infections due to Gram-negative bacilli. Abstract no. S-50-11 presented at the International Congress of Chemotherapy, Kyoto, Japan, Jun, 1985
Patton WN, Smith GM, Leyland MJ, Geddes AM. Multiply resistant Salmonella typhimurium septicaemia in an immunocompromised patient successfully treated with ciprofloxacin. Journal of Antimicrobial Chemotherapy 16: 667–669, 1985
Pedersen SS, Jensen T, Hvidberg EF. Comparative pharmacokinetics of ciprofloxacin and ofloxacin in cystic fibrosis patients. Journal of Antimicrobial Chemotherapy 20: 575–583, 1987
Peerbooms PGM, MacLaren DM. Comparative activities of five antimicrobial agents in experimental Proteus pyelonephritis in mice. Pharmaceutisch Weekblad Scientific Edition 9 (Suppl.): 30–32, 1987
Peeters M, Van Dyck E, Piot P. In vitro activities of the spectinomycin analog U-63366 and four quinolone derivatives against Neisseria gonorrhoeae. Antimicrobial Agents and Chemotherapy 26: 608–609, 1984
Perrone CM, Malinverni R, Glauser MP. Treatment of Staphylococcus aureus endocarditis in rats with coumermycin A1 and ciprofloxacin, alone or in combination. Antimicrobial Agents and Chemotherapy 31: 539–543, 1987
Peters HJ. Comparison of intravenous ciprofloxacin and mezlocillin in treatment of complicated urinary tract infection. European Journal of Clinical Microbiology 5: 253–255, 1986
Piccolomini R, Ravagnan G. Comparative in vitro activity of ciprofloxacin (Bay o 9867) and other antimicrobial agents against urinary bacterial isolates. Chemioterapia 5: 249–256, 1986
Pichler HET, Diridl G, Stickler K, Wolf D. Clinical efficacy of ciprofloxacin compared with placebo in bacterial diarrhoea. American Journal of Medicine 82(Suppl. 4A): 329–332, 1987
Piddock LJV, Diver JM, Wise R. Cross-resistance of nalidixic acid resistant Enterobacteriaeceae to new quinolones and other antimicrobials. European Journal of Microbiology 5: 411–415, 1986
Piddock LJV, Wijnands WJA, Wise R. Quinolone/ureidopenicillin cross-resistance. Lancet 2: 907, 1987
Pien FD, Yamane KK. Ciprofloxacin treatment of soft tissue and respiratory infections in a community outpatient practice. American Journal of Medicine 82(Suppl. 4A): 236–238, 1987
Plaisance KI, Drusano GL, Forrest A, Bustamante CI, Standiford HC. Effect of dose size on bioavailability of ciprofloxacin. Antimicrobial Agents and Chemotherapy 31: 956–958, 1987
Prabhala RH, Rao B, Marshall R, Bansal MB, Thadepalli H. In vitro susceptibility of anaerobic bacteria to ciprofloxacin (Bay o 9867). Antimicrobial Agents and Chemotherapy 26: 785–786, 1984
Preheim LC, Cuevas TA, Roccaforte JS, Mellencamp MA, Bittner MJ. Ciprofloxacin and antacids. Lancet 2: 48, 1986
Preheim LC, Cuevas TA, Roccaforte JS, Mellencamp MA, Bittner MJ. Oral ciprofloxacin in the treatment of elderly patients with complicated urinary tract infections due to trimethoprim/sulfamethoxazole-resistant bacteria. American Journal of Medicine 82(Suppl. 4A): 295–300, 1987
Pugsley MP, Dworzack DL, Horowitz EA, Cuevas TA, Sanders Jr WE, et al. Efficacy of ciprofloxacin in the treatment of nasopharyngeal carriers of Neisseria meningitidis. Journal of Infectious Diseases 156: 211–213, 1987
Pérez-Ruvalcaba JA, Quintero-Pérez NP, Morales-Reyes JJ, Huitrón-Ramirez JA, Rodriguez-Chagollan J, et al. Double-blind comparison of ciprofloxacin and cefotaxime in the treatment of skin and skin structure infections. American Journal of Medicine 82(Suppl. 4A): 242–246, 1987
Raeburn JA, Govan JRW, McCrae WM, Greening AP, Collier PS, et al. Ciprofloxacin therapy in cystic fibrosis. Journal of Antimicrobial Chemotherapy 20: 295–296, 1987
Ramirez CA, Bran JL, Mejia CR, Garcia JF. Clinical efficacy of ciprofloxacin in typhoid fever. In Neu HC & Weuta H (Eds) 1st International Ciprofloxacin Workshop, Leverkusen, 1985, pp. 365–369, Excerpta Medica, Amsterdam, 1986
Ramirez-Ronda CH, Saavedra S, Rivera-Vázques CR. Comparative, double-blind study of oral ciprofloxacin and intravenous cefotaxime in skin and skin structure infections. American Journal of Medicine 82(Suppl. 4A): 220–223, 1987
Raoof S, Wollschager C, Khan FA. Ciprofloxacin increases serum levels of theophylline. American Journal of Medicine 84(Suppl. 4A): 115–118, 1987
Raoult D, Gallais H, De Micco P, Casanova P. Ciprofloxacin therapy for mediterranean spotted fever. Antimicrobial Agents and Chemotherapy 30: 606–607, 1986
Ratcliffe NT, Smith JT. Ciprofloxacin and ofloxacin exhibit a rifampicin-resistant bactericidal mechanism not detectable in other 4-quinolone antibacterial agents. Journal of Pharmacy and Pharmacology 36 (Suppl.): 59P, 1984a
Ratcliffe NT, Smith JT. Effects of magnesium on the activity of 4-quinolone antibacterial agents. Journal of Pharmacy and Pharmacology 35 (Suppl.): 61P, 1983
Ratcliffe NT, Smith JT. The mechanism of reduced activity of 4-quinolone agents in urine. Fortschritte der Antimikrobiellen und Antineoplastischen Chemotherapie (Band 3–5): 563–569, 1984b
Reeves DS, Bywater MJ, Holt HA, White LO. In-vitro studies with ciprofloxacin, a new 4-quinolone compound. Journal of Antimicrobial Chemotherapy 13: 333–346, 1984
Reinhardt JF, George WL. Comparative in vitro activities of selected antimicrobial agents against Aeromonas species and Plesiomonas shigelloides. Antimicrobial Agents and Chemotherapy 27: 643–645, 1985
Renkonen O-V, Sivonen A, Visakorpi R. Effect of ciprofloxacin on carrier rate of Neisseria meningitidis in army recruits in Finland. Antimicrobial Agents and Chemotherapy 31: 962–963, 1987
Ridgway GL, Mumtaz G, Gabriel FG, Oriel JD. The activity of ciprofloxacin and other 4-quinolones against Chlamydia trachomatis and Mycoplasmas in vitro. European Journal of Clinical Microbiology 3: 344–346, 1984
Righter J. Ciprofloxacin treatment of Staphylococcus aureus infections. Journal of Antimicrobial Chemotherapy 20: 595–597, 1987
Righter J. In vitro activity of ciprofloxacin, azthreonam and ceftazidime against Serratia marcescens and Pseudomonas aeruginosa. European Journal of Clinical Microbiology 3: 368–369, 1984
Roberts CM, Batten J, Hodson ME. Ciprofloxacin-resistant Pseudomonas. Lancet 1: 1442, 1985
Robson HG. Ciprofloxacin comparative efficacy against Pseudomonas aeruginosa bacteremia in a neutropenic rat model. Proceedings of the 14th International Congress of Chemotherapy, abstract no. S-32-11, Kyoto, Japan, 1985
Roddy RE, Handsfield HH, Hook EW. Comparative trial of single-dose ciprofloxacin and ampicillin plus probenecid for treatment of gonococcal urethritis in men. Antimicrobial Agents and Chemotherapy 30: 267–269, 1986
Rohwedder RW, Bergan T. Non-renal elimination of ciprofloxacin. Proceedings of the Congress on Bacterial and Parasitic Drug Resistance, Bangkok, 10–13 Dec, 1986
Rolin O, Huet Y, Bouanchand DH. Comparative efficacy of pefloxacin and six other antimicrobial agents on Staphylococcus aureus experimental abscesses. Journal of Antimicrobial Chemotherapy 17(Suppl. B): 49–52, 1986
Ronconi P, Carosi M, Cosentina R, Pittiruti M, Castiglioni GC. Clinical efficacy of ciprofloxacin in surgical infections. 1st International Ciprofloxacin Workshop, Leverkusen, Nov. 6–8, 1985, Current Clinical Practice Series 34, pp. 390–392, Excerpta Medica, Amsterdam, 1986
Ronnlund RD, Chartrand SA, Gaubatz JW. Inhibition of ATP dependent DNA gyrase supercoiling activity by quinolone antibiotics. Abstract A26 presented at the 85th Annual Meeting of the American Society for Microbiology, Las Vegas, USA, 1985
Roosendaal R, Bakker-Woudenberg IAJM, Van den Berghe-Van Raffe M, Vink-Van den Berg, JC, Michel MF. Comparative activities of ciprofloxacin and ceftazidime against Klebsiella pneumoniae in vitro and in experimental pneumonia in leukopenic rats. Antimicrobial Agents and Chemotherapy 31: 1809–1815, 1987
Roszkowski W, Ciborowski P, Ko HL, Schumacher-Pertreau F, Roszkowski K, et al. The effect of subinhibitory concentrations of selected antibiotics on bacteria-phagocyte interaction. In Adam et al. (Eds) The influence of antibiotics on the host parasite relationship, pp. 179–187, Springer Verlag, Berlin, 1985
Roy C, Foz A, Segura C, Tirado M, Teixell M, et al. Activity of ciprofloxacin (BAY o 9867) against Pseudomonas aeruginosa and ampicillin-resistant Enterobacteriaceae. Infection 11: 326–328, 1983
Rozenberg-Arska M, Dekker AW, Verhoef J. Ciprofloxacin for selective decontamination of the alimentary tract in patients with acute leukemia during remission induction treatment: the effect on fecal flora. Journal of Infectious Diseases 152: 104–107, 1985
Rubinstein E, Mark Z, Samra Y, Alkan M, Berger S. In vitro activity of ciprofloxacin compared with other agents against recent hospital isolates. Chemioterapia 5: 75–82, 1986
Rubio T. Oral ciprofloxacin in the treatment of P. aeruginosa infection in children with cystic fibrosis. Pediatric Pulmonology 1 (Suppl.): 128–129, 1987
Ruckdeschel G, Ehret W, Ahl A. Susceptibility of Legionella spp. to quinolone derivatives and related organic acids. European Journal of Clinical Microbiology 3: 373, 1984
Rudin JE, Norden CW, Shinners EM. In vitro activity of ciprofloxacin against aerobic Gram-negative bacteria. Antimicrobial Agents and Chemotherapy 26: 597–598, 1984
Rudrik JT, Cavalieri SJ, Britt EM. Proposed quality control and interpretive criteria for disk diffusion susceptibility testing with enoxacin. Journal of Clinical Microbiology 21: 332–334, 1985
Ryan JL, Berenson CS, Greco TP, Mangi RJ, Sims M, et al. Oral ciprofloxacin in resistant urinary tract infections. American Journal of Medicine 82(Suppl. 4A): 303–306, 1987
Saavedra S, Ramírez-Ronda CH, Nevárez M. Ciprofloxacin in the treatment of urinary tract infections caused by Pseudomonas aeruginosa and multiresistant bacteria. European Journal of Clinical Microbiology 5: 255–257, 1986
Saito A, Koga H, Shigeno H, Watanabe K, Mori K, et al. The antimicrobial activity of ciprofloxacin against Legionella species and the treatment of experimental Legionella pneumonia in guinea pigs. Journal of Antimicrobial Chemotherapy 18: 251–260, 1986
Saito I, Terada Y, Yokozawa M, Ono K, Yamaguchi K, et al. Clinical study on Bay 0 9867 in gonococcal urethritis. Chemotherapy (Tokyo) 33(Suppl. 7): 621–631, 1985
Salh B, Webb AK. Ciprofloxacin resistance. Lancet 1: 749–750, 1987
Samonis G, Ho DH, Gooch GF, Rolston KVI, Bodey GP. In vitro susceptibility of Citrobacter species to various antimicrobial agents. Antimicrobial Agents and Chemotherapy 31: 829–830, 1987
Samsom JP. Influence of haemodialysis on the pharmacokinetics of ciprofloxacin. Pharmaceutisch Weekblad Scientific Edition 9 (Suppl.): 23–25, 1987
Sanders CC, Sanders WE, Goering RV. Overview of preclinical studies with ciprofloxacin. American Journal of Medicine 82(Suppl. 4A): 2–11, 1987
Sanders CC, Sanders WE, Goering RV, Werner V. Selection of multiple antibiotic resistance by quinolones, β-lactams, and aminoglycosides with special reference to cross-resistance between unrelated drug classes. Antimicrobial Agents and Chemotherapy 26: 797–801, 1984
Sanson-Le Pors M-J, Casin IM, Thebault M-C, Arlet G, Perol Y. In vitro activities of U-63366, a spectinomycin analog; roxithromycin (RU 28965), a new macrolide antibiotic; and five quinolone derivatives against Haemophilus ducreyi. Antimicrobial Agents and Chemotherapy 30: 512–513, 1986
Sato K, Inoue Y, Yamashita S, Inoue M, Mitsuhashi S. Inhibitory effect of ofloxacin and other new pyridonecarboxylic acids on the activities of DNA gyrase isolated from Escherichia coli, Pseudomonas aeruginosa and Bacteroides fragilis. In Mitsuhashi & Daikos (Eds) Ofloxacin: a new quinolone antibacterial agent. Proceedings of a Workshop held at the 14th International Congress of Chemotherapy, Kyoto, Japan, 1985, pp. 21–25, University of Tokyo Press, Tokyo, 1985
Sauerwein D, Bauernfeind A, Petermüller C. Clinical and bacteriological evaluation of ciprofloxacin in treatment of UTIs of para- and tetraplegic patients. 14th International Congress of Chemotherapy, Kyoto, Japan, Jun, 1985
Schacht P, Arcieri G, Branolte J, Bruck H, Chysky V, et al. Worldwide clinical data on efficacy and safety of ciprofloxacin. In Neu HC (Ed.) Ciprofloxacin: clinical monograph, pp. 69–79, ADIS Press International Ltd, Manchester, 1988
Schacht P, Bruck H, Chysky V, Hullmann R, Weuta H, et al. Overall clinical results with ciprofloxacin. Proceedings of the 14th International Congress of Chemotherapy, Kyoto, Japan, Jun, 1985
Schacht P, Arcieri G, Branolte J, Bruck H, Chysky V, et al. Worldwide clinical data on efficacy and safety of ciprofloxacin. In Neu HC (Ed.) Ciprofloxacin: clinical monograph, pp. 69–79, ADIS Press International Ltd, Manchester, 1988
Schacht P, Hullmann R. Development of resistance during phase II and III clinical trials with ciprofloxacin. Proceedings of the Congress on Bacterial and Parasitic Drug Resistance, Bangkok, 10–13 Dec, 1986
Schacht P, Hullmann R. Changes of susceptibility of infecting organisms to ciprofloxacin during treatment. Abstract No. 15. Proceedings of the Biennial Conference on Chemotherapy of Infectious Diseases and Malignancies, Munich, 26–29 April, 1987
Schentag JJ, Domagala JM. Structure-activity relationship with the quinolone antibiotics. Research and Clinical Forums 7: 9–15, 1985
Schiff JB, Small GJ, Pennington JE. Comparative activities of ciprofloxacin, ticarcillin, and tobramycin against experimental Pseudomonas aeruginosa pneumonia. Antimicrobial Agents and Chemotherapy 26: 1–4, 1984
Schlenkoff D, Dalhoff A, Knopf J, Opferkuch W. Penetration of ciprofloxacin into human lung tissue following intravenous injection. Infection 14: 299–300, 1986
Schlüter G. Ciprofloxacin: review of potential toxicologic effects. American Journal of Medicine 82(Suppl. 4A): 91–93, 1987
Schlüter G. Toxicology of ciprofloxacin. In Neu HC, Weuta H (Eds) 1st International Ciprofloxacin Workshop, Leverkusen 1985, pp. 291–296, Excerpta Medica, Amsterdam, 1986
Schmicker R, Naumann G. Efficacy of ciprofloxacin in urinary tract infections in geriatric patients. In Neu HC & Weuta H (Eds) 1st International Ciprofloxacin Workshop, Leverkusen, 1985, pp. 305–309, Excerpta Medica, Amsterdam, 1986
Scholl H, Schmidt K, Weber B. Sensitive and selective determination of picogram amounts of ciprofloxacin and its metabolites in biological samples using high-performance liquid chromatography and photothermal post-column derivatization. Journal of Chromatography 416: 321–330, 1987
Scott AC, Fleming LW, Stewart WK. Efficacy of ciprofloxacin in treatment of CAPD. European Journal of Clinical Microbiology 6: 599, 1987
Scott GR, McMillan A, Young H. Ciprofloxacin versus ampicillin and probenecid in the treatment of uncomplicated gonorrhoea in men. Journal of Antimicrobial Chemotherapy 20: 117–121, 1987
Scribner RK, Muszynski MJ, Marks MI. In vitro activity of antimicrobials, alone and in combination, against Pseudomonas cepacia. Abstract 394, 24th Interscience Conference on Antimicrobial Agents and Chemotherapy, Washington DC, 1984
Scully BE, Jules K, Chin N-X, Neu HC. Effect of ciprofloxacin on fecal flora of patients with cystic fibrosis and other patients treated with oral ciprofloxacin. American Journal of Medicine 82(Suppl. 4A): 336–338, 1987a
Scully BE, Nakatomi M, Ores C, Davidson S, Neu HC. Ciprofloxacin therapy in cystic fibrosis. American Journal of Medicine 82(Suppl. 4A): 196–201, 1987b
Scully BE, Neu HC. Oral ciprofloxacin therapy of infection caused by multiply resistant bacteria other than Pseudomonas aeruginosa. Journal of Antimicrobial Chemotherapy 18(Suppl. D): 179–185, 1986
Scully BE, Neu HC. Treatment of serious infections with intravenous ciprofloxacin. American Journal of Medicine 82(Suppl. 4A): 369–375, 1987
Scully BE, Parry MF, Neu HC, Mandell W. Oral ciprofloxacin therapy of infections due to Pseudomonas aeruginosa. Lancet 1: 819–822, 1986
Segev S, Rubinstein E, Shick J, Rabinovitch O, Dolitsky M. Penetration of ciprofloxacin into female pelvic tissues. European Journal of Clinical Microbiology 5: 207–209, 1986
Self PL, Zeluff BA, Sollo D, Gentry LO. Use of ciprofloxacin in the treatment of serious skin and skin structure infections. American Journal of Medicine 82(Suppl. 4A): 239–241, 1987
Selwyn S, Bakhtiar M. Comparative in-vitro studies on a new azaquinolone, enoxacin. Drugs in Experimental Clinical Research 10: 653–668, 1984
Shah PM, Enzenberger R, Glogau O, Knothe H. Influence of oral ciprofloxacin or ofloxacin on the fecal flora of healthy volunteers. American Journal of Medicine 82(Suppl. 4A): 333–335, 1987a
Shah PM, Just G, Staszewski S, Helm EB, Brodt R, et al. Ciprofloxacin und Imipenem bei Nocardiose. Deutsche Medizinische Wochenschrift 112: 1101, 1987b
Shahmanesh M, Shukla SR, Phillips I, Westwood A, Thin RN. Ciprofloxacin for treating urethral gonorrhoea in men. Genitourinary Medicine 62: 86–87, 1986
Shalit I, Greenwood RB, Marks MI, Pederson JA, Frederick DL. Pharmacokinetics of single-dose oral ciprofloxacin in patients undergoing chronic ambulatory peritoneal dialysis. Antimicrobial Agents and Chemotherapy 30: 152–156, 1986
Shalit I, Stutman HR, Marks MI, Chartrand SA, Hilman BC. Randomized study of two dosage regimens of ciprofloxacin for treating chronic bronchopulmonary infection in patients with cystic fibrosis. American Journal of Medicine 82(Suppl. 4A): 189–195, 1987
Shalit I, Welch DF, San Joaquin VH, Marker MI. In vitro antibacterial activities of antibiotics against Pseudomonas aeruginosa in peritoneal dialysis fluid. Antimicrobial Agents and Chemotherapy 27: 908–911, 1985
Shwachman H, Kulcyzcki LL. Long-term study of one hundred five patients with cystic fibrosis. American Journal of Diseases of Children 96: 6–15, 1958
Simberkoff MS, Rahal JJ. Bactericidal activity of ciprofloxacin against amikacin- and cefotaxime-resistant Gram-negative bacilli and methicillin-resistant staphylococci. Antimicrobial Agents and Chemotherapy 29: 1098–1100, 1986
Singlas E, Taburet AM, Landru I, Albin H, Ryckelinck JP. Pharmacokinetics of ciprofloxacin tablets in renal failure: influence of haemodialysis 31: 589–593, 1987
Slama TG, Misinski J, Sklar S. Oral ciprofloxacin therapy for osteomyelitis caused by aerobic Gram-negative bacilli. American Journal of Medicine 82(Suppl. 4A): 259–261, 1987
Smith CR. The adverse effects of fluoroquinolones. Journal of Antimicrobial Chemotherapy 19: 709–712, 1987
Smith GM, Cashmore C, Leyland MJ. Ciprofloxacin-resistant staphylococci. Lancet 2: 949, 1985
Smith GM, Leyland MJ, Farrell ID, Geddes AM. Preliminary evaluation of ciprofloxacin, a new 4-quinolone antibiotic in the treatment of febrile neutropenic patients. Journal of Antimicrobial Chemotherapy 18(Suppl. D): 165–174, 1986a
Smith JT. Awakening the slumbering potential of the 4-quinolone antibacterials. Pharmaceutical Journal 233: 299–305, 1984a
Smith JT. Chemistry and mode of action of 4-quinolone agents. Fortschritte der Antimikrobiellen und Antineoplastischen Chemotherapie 3: 493–508, 1984b
Smith JT. Mutational resistance to 4-quinolone antibacterial agents. European Journal of Clinical Microbiology 3: 347–350, 1984c
Smith JT. The mode of action of 4-quinolones and possible mechanisms of resistance. Journal of Antimicrobial Chemotherapy 18(Suppl. D): 21–29, 1986a
Smith MJ, Hodson ME, Barten JC. Ciprofloxacin in cystic fibrosis. Correspondence. Lancet 1: 1103, 1986b
Smith SM, Eng RHK. Activity of ciprofloxacin against methicillin-resistant Staphylococcus aureus. Antimicrobial Agents and Chemotherapy 27: 688–691, 1985
Smith SM, Eng RHK, Berman E. The effect of ciprofloxacin on methicillin-resistant Staphylococcus aureus. Journal of Antimicrobial Chemotherapy 17: 287–295, 1986c
Smith SM. In vitro comparison of A-56619, A-56620, amifloxacin, ciprofloxacin, enoxacin, norfloxacin, and ofloxacin against methicillin resistant Staphylococcus aureus. Antimicrobial Agents and Chemotherapy 29: 325–326, 1986b
Sobieski MW, Scheid WM. Comparative activity of ciprofloxacin and ofloxacin in experimental H. influenzae meningitis. Proceedings of the 25th Interscience Conference on Antimicrobial Agents and Chemotherapy, abstract no. 216, Minneapolis, USA, 1985
Staib AH, Harder S, Mieke S, Beer C, Stille W, et al. Gyraseinhibitors impair caffeine elimination in man. Methods and Findings in Experimental and Clinical Pharmacology 9: 193–198, 1987
Standiford HC, Drusano GL, Forrest A, Tatern B, Plaisance K. Bactericidal activity of ciprofloxacin compared with that of cefotaxime in normal volunteers. Antimicrobial Agents and Chemotherapy 31: 1172–1182, 1987
Stille W, Schäfer-Lotz G, Puppel H. Activity of β-lactam-antibiotics against Yersinia enterocolitica. Presented at the 13th International Congress of Chemotherapy, Vienna, 1983
Stolz E, Wagenvoort JHT, Van der Willigen AH. Quinolones in the treatment of gonorrhoea and Chlamydia trachomatis infection. Pharmaceutisch Weekblad Scientific Edition 9 (Suppl.) 82–85, 1987
Stratton CW, Lin C, Weeks LS. Activity of LY 146032 compared with that of methicillin, cefazolin, cefamandole, cefuroxime, ciprofloxacin, and vancomycin against Staphylococci as determined by kill-kinetic studies. Antimicrobial Agents and Chemotherapy 31: 1210–1215, 1987
Strunk RW, Gratz JC, Maserati R, Scheid WM. Comparison of ciprofloxacin with azlocillin plus tobramycin in the therapy of experimental Pseudomonas aeruginosa endocarditis. Antimicrobial Agents and Chemotherapy 28: 428–432, 1985
Stutman HR, Shalit I, Marks MI, Greenwood R, Chartrand SA, et al. Pharmacokinetics of two dosage regimens of ciprofloxacin during a two-week therapeutic trial in patients with cystic fibrosis. American Journal of Medicine 82(Suppl. 4A): 142–145, 1987
Stutman HR. Summary of a workshop on ciprofloxacin use in patients with cystic fibrosis. Pediatric Infectious Diseases Journal 6: 932–935, 1987
Stuyck J, Verbist L, Mulier JC. Treatment of chronic osteomyelitis with ciprofloxacin. Pharmaceutisch Weekblad Scientific Edition 9 (Suppl): 93–95, 1987
Suerbaum S, Leying H, Kroll H-P, Gmeiner J, Opferkuch W. Influence of β-lactam antibiotics and ciprofloxacin on cell envelope of Escherichia coli. Antimicrobial Agents and Chemotherapy 31: 1106–1110, 1987
Sutter VL, Kwok Y-Y, Bulkacz J. Comparative activity of ciprofloxacin against anaerobic bacteria. Antimicrobial Agents and Chemotherapy 27: 427–428, 1985
Swenson JM, Wallace RJ, Silcox VA, Thornsberry C. Antimicrobial susceptibility of five subgroups of Mycobacterium fortuitum and Mycobacterium chelonae. Antimicrobial Agents and Chemotherapy 28: 807–811, 1985
Szaff M, Høiby N, Flensborg EW. Frequent antibiotic therapy improves survival in cystic fibrosis patients with chronic Pseudomonas aeruginosa infection. Acta Paediatrica Scandinavica 72: 651–657, 1983
Szarmach H, Weuta H, Skazynski J, Wronski A. Ciprofloxacin in acute male gonorrhea. Arzneimittel-Forschung 36: 1840–1842, 1986
Tanimura H, Tominaga S, Rai F, Matsumoto H. Transfer of ciprofloxacin to bile and determination of biliary metabolites in humans. Arzneimittel-Forschung 36: 1417–1420, 1986
Tartaglione TA, Raffalovich AC, Poynor WJ, Espinel-Ingroff A, Kerkering TM. Pharmacokinetics and tolerance of ciprofloxacin after sequential increasing oral doses. Antimicrobial Agents and Chemotherapy 29: 62–66, 1986
Taylor DN, Echeverria P, Hanchalay S, Pitarangsi C, Slootmans L, et al. Antimicrobial susceptibility and characterization of outer membrane proteins of Haemophilus ducreyi isolated in Thailand. Journal of Clinical Microbiology 21: 442–444, 1985
Tegelberg-Stassen MJAM, van der Hoek JCS, Mooi L, Wagenvoort JHT, van Joost T, et al. Treatment of uncomplicated gonococcal urethritis in men with two dosages of ciprofloxacin. European Journal of Clinical Microbiology 5: 244–246, 1986
Thadepalli H, Prabhala R, Bansal M. Evaluation of ciprofloxacin and cefotaxime in treatment of experimental subcutaneous abscess in mice. 14th International Congress of Chemotherapy, abstract no. 32–14, Kyoto, Japan, 1985
Thorsteinsson SB, Bergan T, Johannesson G, Thorsteinsson HS, Rohwedder R. Tolerance of ciprofloxacin at injection site, systemic safety and effect on electroencephalogram. Chemotherapy 33: 448–451, 1987
Thorsteinsson SB, Bergan T, Oddsdottir S, Rohwedder R, Holm R. Crystalluria and ciprofloxacin, influence of urinary pH and hydration. Chemotherapy 32: 408–417, 1986
Tietgen K, Schulz E, Boness J, Marre R. Ciprofloxacin und Cefotaxim: pharmakokinetik und therapeutische Effektivität bei der E. coli-Pyelonephritis der Ratte. Immunologie und Infektion 14: 152–155, 1986
Tolkoff-Rubin N, Rubin RH. New approaches to the treatment of urinary tract infection. American Journal of Medicine 82(Suppl. 4A): 270–277, 1987
Trautmann M, Krause B, Birnbaum D, Wagner J, Lenk K. Serum bactericidal activity of two newer quinolones against Salmonella typhi compared with standard therapeutic regimens. European Journal of Microbiology 5: 297–302, 1986
Trexler Hessen M, Ingerman MJ, Kaufman DH, Weiner P, Santoro J, et al. Clinical efficacy of ciprofloxacin therapy for Gram-negative bacillary osteomyelitis. American Journal of Medicine 82(Suppl. 4A): 262–265, 1987
Turgeon PL, Gaudreau CL, Mantha R. Comparative in vitro activity of four quinolones and four other agents against enteropathogens. Current Therapeutic Research 41: 584–588, 1987
Ullmann U, Giebel W, Dalhoff A, Koeppe P. Single and multiple dose pharmacokinetics of ciprofloxacin. European Journal of Clinical Microbiology 5: 193–196, 1984
Ulrich E, Tautmann M, Weinke T, Hahn H. Treatment of experimental Pseudomonas septicemia with ciprofloxacin and other antipseudomonal drugs. Proceedings of the International Symposium on New Quinolones, abstract no. 112, Geneva, 1986
Valainis GT, Pankey GA, Katner HP, Cortez LM, Dalovisio JR. Ciprofloxacin in the treatment of bacterial skin infections. American Journal of Medicine 82(Suppl. 4A): 230–232, 1987
Valainis G, Thomas D, Pankey G. Penetration of ciprofloxacin into cerebrospinal fluid. European Journal of Clinical Microbiology 5: 207–209, 1986
Vallée F, Lebel M, Bergeron MG. Determination of ciprofloxacin in biological samples by reversed-phase high performance liquid chromatography. Therapeutic Drug Monitoring 8: 340–345, 1986
Van Caekenberghe DL, Pattyn SR. In vitro activity of ciprofloxacin compared with those of other new fluorinated piperazinyl-substituted quinolone derivatives. Antimicrobial Agents and Chemotherapy 25: 518–521, 1984
Van de Heyning PH, Pattyn SR, Valcke HD. Ciprofloxacin in oral treatment of ear infections. Pharmaceutisch Weekblad — Scientific Edition 8: 63–66, 1986
Van de Heyning PH, Pattyn SR, Valcke HD, Van Caekenberghe DL, Claes J. The use of fluoroquinolones in chronic otitis suppurativa. Pharmaceutisch Weekblad Scientific Edition 9 (Suppl.): 87–89, 1987
Van der Auwera P, Klastersky J. Bactericidal activity and killing rate of serum in volunteers receiving ciprofloxacin alone or in combination with vancomycin. Antimicrobial Agents and Chemotherapy 30: 892–895, 1986
Van der Auwera P, Scorneaux B. In vitro susceptibility of Campylobacter jejuni to 27 antimicrobial agents and various combinations of β-lactams with clavulanic acid and sulbactam. Antimicrobial Agents and Chemotherapy 28: 37–40, 1985
Van Poppel H, Wegge M, Dammekens H, Chysky V. Oral treatment of Pseudomonas-induced urinary tract infections with ciprofloxacin. Chemotherapy 32: 83–87, 1986b
Van Poppel H, Wegge M, Dammekens H, Chysky V. Ciprofloxacin in the treatment of urinary tract infection in patients with multiple sclerosis. European Journal of Clinical Microbiology 5: 251–253, 1986a
Vanhoof R, Hubrechts JM, Roebben E, Nyssen HJ, Nulens E, et al. The comparative activity of pefloxacin, enoxacin, ciprofloxacin and 13 other antimicrobial agents against enteropathogenic microorganisms. Infection 14: 294–298, 1986
Van der Waaij D. Colonisation resistance of the digestive tract: clinical consequences and implications. Journal of Antimicrobial Chemotherapy 10: 263–270, 1982
Van Saene JJM, van Saene HKF, Geitz JN, Jarko-Smit WJP, Lerk CF. Quinolones and colonisation resistance in human volunteers. Pharmaceutisch Weekblad — Scientific Edition 8: 67–71, 1986
Venezio FR, Tatarowicz W, DiVincenzo CA, O’Keefe JP. Activity of ciprofloxacin against multiply resistant strains of Pseudomonas aeruginosa, Staphylococcus epidermidis, and Group JK corynebacteria. Antimicrobial Agents and Chemotherapy 30: 940–941, 1986
Verbist L. Comparative in vitro activity of the new quinolone CI-934. European Journal of Clinical Microbiology 5: 343–345, 1986
Wall RA, Mabey DCW, Bello CSS, Felmingham D. The comparative in-vitro activity of twelve 4-quinolone antimicrobials against Haemophilus ducreyi. Journal of Antimicrobial Chemotherapy 16: 165–168, 1985
Warren RE, Newsom SWB. Ciprofloxacin vs nalidixic acid gut decontamination to stop spread of gentamicin-resistant Klebsiellas. Abstract No. 932 of 24th Interscience Conference on Antimicrobial Agents and Chemotherapy, 8–10 Oct, 1984
Watanabe K, Aoki M, Kobayashi T, Sawa K, Ueno K. Effect of BAY o 9867 on human fecal flora. Chemotherapy 33(Suppl. 7): 88–99, 1985
Watt B, Brown FV. Is ciprofloxacin active against clinically important anaerobes? Journal of Antimicrobial Chemotherapy 17: 605–613, 1986
Weber AH, Scribner RK, Marks MI. In vitro activity of ciprofloxacin against pediatric pathogens. Chemotherapy (Basel) 31: 456–465, 1985
Weidner W, Schiefer HG, Dalhoff A. Treatment of chronic bacterial prostatitis with ciprofloxacin: results of a one-year follow-up study. American Journal of Medicine 82(Suppl. 4A): 280–283, 1987
Weinstein RA, Nathan G, Delzell D, Kabins SA. In vitro susceptibility of nosocomial Pseudomonas aeruginosa, Enterobacteriaceae, and staphylococci to ciprofloxacin and ten other broad-spectrum antibiotics. Chemioterapia 6: 315–318, 1987
Weiss D, Trautmann M, Wagner J, Borner K, Hahn H. Ciprofloxacin: a comparative evaluation of its bactericidal activity in human serum against four enterobacterial species. Drugs in Experimental Clinical Research 12: 889–894, 1986
Weissauer-Condon C, Engels I, Daschner FD. In vitro activity of four new quinolones in Mueller-Hinton broth and peritoneal dialysis fluid. European Journal of Clinical Microbiology 6: 324–326, 1987
Weisser J, Wiedemann B. Brief report: effect of ciprofloxacin on plasmids. American Journal of Medicine 82: 21–22, 1987
Whitby M, Edwards P, Holliday A, Finch RG. Ciprofloxacin: A clinical evaluation and assessment of its effect on faecal flora. 14th International Congress on Chemotherapy, p. 400, Kyoto, Japan, 1985
Whiting JL, Cheng N, Chow AW. Interactions of ciprofloxacin with clindamycin, metronidazole, cefoxitin, cefotaxime, and mezlocillin against Gram-positive and Gram-negative anaerobic bacteria. Antimicrobial Agents and Chemotherapy 31: 1379–1382, 1987
Wijnands WJA, Vree TB, Baars AM, Van Herwaarden CLA. Steady-state kinetics of the quinolone derivatives ofloxacin, enoxacin, ciprofloxacin and pefloxacin during maintenance treatment with theophylline. Drugs 34(Suppl. 1): 159–169, 1987
Wijnands WJA, Vree TB, Van Herwaarden CLA. The influence of quinolone derivatives on theophylline clearance. British Journal of Clinical Pharmacology 22: 677–683, 1986
Wiley R, Lode H, Höffken G, Wagner J, Borner K. Ciprofloxacin versus imipenem/cilastatin: a prospective randomized study in 60 patients with severe infections. Abstract S-51-5 of the 14th International Congress of Chemotherapy, Kyoto, Japan, Jun, 1985
Williams AH, Grüneberg RN. Ciprofloxacin and co-trimoxazole in urinary tract infections. Journal of Antimicrobial Chemotherapy 18(Suppl. D): 107–110, 1986
Williams P. Sub-MIC’s of cefuroxime and ciprofloxacin influence interaction of complement and immunoglobulins with Klebsiella pneumoniae. Antimicrobial Agents and Chemotherapy 31: 758–762, 1987
Wingender W, Beerman D, Foerster D, Graefe K-H, Schacht P, et al. Mechanism of renal excretion of ciprofloxacin (Bay o 9867), a new quinolone carboxylic acid derivative, in humans. Abstract 621 of the 4th Mediterranean Congress of Chemotherapy, Rhodes, 1984a
Wingender W, Foerster D, Beerman D, Rohwedder R, Graefe KH, et al. Effect of gastric emptying time on rate and extent of systemic availability of ciprofloxacin. Abstract no. P-37-91 of the 14th International Congress of Chemotherapy, Kyoto, Japan, 1985
Wingender W, Graefe K-H, Gau W, Förster D, Beerman D, et al. Pharmacokinetics of ciprofloxacin after oral and intravenous administration in healthy volunteers. European Journal of Clinical Microbiology 3: 355–359, 1984b
Wise R, Andrews JM, Edwards LJ. In vitro activity of Bay O 9867, a new quinolone derivative, compared with those of other antimicrobial agents. Antimicrobial Agents and Chemotherapy 23: 559–564, 1983
Wise R, Donovan IA. Tissue penetration and metabolism of ciprofloxacin. American Journal of Medicine 82(Suppl. 4A): 103–107, 1987
Wise R, Lockley RM, Webberly M, Dent J. Pharmacokinetics of intravenously administered ciprofloxacin. Antimicrobial Agents and Chemotherapy 26: 208–210, 1984
Wittmann DH, Teichmann W, Huebner A, Fock R, Bauernfeind A. Penetration of ciprofloxacin into inorganic and organic bone compartments. Abstract S-40-7, International Congress of Chemotherapy, Kyoto, Japan, 1985
Wolff M, Boutron L, Singlas E, Clair B, Decazes JM, et al. Penetration of ciprofloxacin into cerebrospinal fluid of patients with bacterial meningitis. Antimicrobial Agents and Chemotherapy 31: 899–902, 1987
Wollschlager CM, Raoof S, Khan FA, Guarneri J, LaBombardi V, et al. Controlled, comparative study of ciprofloxacin versus ampicillin in treatment of bacterial respiratory tract infections. American Journal of Medicine 82: 164–168, 1987
Wood ME, Newland AC. Intravenous ciprofloxacin in the treatment of infection in immunocompromised patients. Journal of Antimicrobial Chemotherapy 18(Suppl. D): 175–178, 1986
Wood MJ, Logan MN. Ciprofloxacin for soft tissue infections. Journal of Antimicrobial Chemotherapy 18(Suppl. D): 159–164, 1986
Yamaguchi K, Hara K. Clinical evaluation of ciprofloxacin in the field of internal medicine in Japan. Proceedings of the 14th International Congress of Chemotherapy, Kyoto, Japan, Jun, 1985
Yu VL, Stoehr G, Rubin J, Matador A, Kamarer D. Efficacy of oral ciprofloxacin plus rifampin for therapy of malignant otitis externa. Abstract no. 188. Proceedings of the 27th Interscience Conference of Antimicrobial Agents and Chemotherapy, New York, Oct 4–7, 1987
Zeiler H-J. Influence of pH and human urine on the antibacterial activity of ciprofloxacin, norfloxacin and ofloxacin. Drugs in Experimental Clinical Research 11: 335–338, 1985
Zeiler H-J, Voigt WH. Efficacy of ciprofloxacin on stationary-phase bacteria in vivo. American Journal of Medicine 82(Suppl. 4A): 87–91, 1987
Zeiler H-J, Petersen U, Gau W, Ploschke HJ. Antibacterial activity of the metabolites of ciprofloxacin and its significance in the bioassay. Arzneimittel-Forschung 37: 131–134, 1987
Zweerink MM, Edison A. Inhibition of Micrococcus luteus DNA gyrase by norfloxacin and 10 other quinolone carboxylic acids. Antimicrobial Agents and Chemotherapy 29: 598–601, 1986
Author information
Authors and Affiliations
Additional information
Various sections of the manuscript reviewed by: A.P. Ball, Infectious Disease Unit, Cameron Hospital, Fife, Scotland; A.L. Barry, Clinical Microbiology Institute, Tualatin, Oregon, USA; T. Bergan, Department of Microbiology, Institute of Pharmacy, University of Oslo, Oslo, Norway; A. Digrams, Department of Microbiology and Immunology, The Gade Institute, Haukeland Hospital, Bergen, Norway; G.L. Drusano, Department of Medicine, University of Maryland School of Medicine, Baltimore, Maryland, USA; R. Janknegt, Klinische Pharmacie, Hospital Sittard, Sittard, The Netherlands; J. Kumazawa, Department of Urology, Faculty of Medicine, Kyushu University, Fukuoka, Japan; M. LeBel, Université Laval and Service d’Infectiologie, Centre Hospitalier de L’Université Laval, Québec, Canada; L.A. Mandell, McMaster University, Henderson General Hospital, Hamilton, Ontario, Canada; S.W. Newsom, Hospital Infection Society, Papworth Hospital, Cambridge, England; S.R. Norrby, Department of Infectious Diseases, University of Umea, Umea University Hospital, Umea, Sweden; D. Pastel, Cedars-Sinai Medical Center, Department of Pharmacy, Los Angeles, California, USA; S.M. Smith, Microbiology Section, Veterans Administration Medical Center, East Orange, New Jersey, USA; D.J. Winston, Los Angeles, California, USA; J.S. Wolfson, Infectious Disease Unit, Massachusetts General Hospital, Boston, Massachusetts, USA.
Rights and permissions
About this article
Cite this article
Campoli-Richards, D.M., Monk, J.P., Price, A. et al. Ciprofloxacin. Drugs 35, 373–447 (1988). https://doi.org/10.2165/00003495-198835040-00003
Published:
Issue Date:
DOI: https://doi.org/10.2165/00003495-198835040-00003