Summary
Several clinical studies have shown oral morphine and methadone to be effective in the treatment of intractable pain in patients with malignant disease. Recent pharmacokinetic studies have confirmed the rationale for regular administration of oral morphine and methadone but have revealed marked interindividual differences in the kinetics and metabolism which must be considered when titrating the oral dose according to the individual patient’s need.
Oral absorption of morphine in patients with malignant diseases is rapid, with peak plasma concentrations occurring at 20 to 90 minutes. Predose steady-state concentrations bear a constant relationship to dose, but vary considerably between individuals. The oral bioavailability is approximately 40% with marked patient-to-patient variations as a result of differences in presystemic elimination. The reported values for the volume of distribution range from 1.0 to 4.7 L/kg. Plasma protein binding is about 30%. The elimination half-life varies between 0.7 and 7.8 hours. Plasma clearance is approximately 19 ml/min/kg (5 to 34 ml/min/kg) and mostly accounted for by metabolic clearance. Studies in a few patients with malignant diseases treated regularly with daily doses of oral morphine ranging from 20 to 750mg indicate a linear relationship between the dose and trough concentration of morphine. Long term treatment with 10- to 20-fold increase of the oral dose over a period of 6 to 8 months does not seem to change the kinetics of oral morphine.
The plasma concentrations of the main metabolite, morphine-3-glucuronide (M3G), exceed those of the parent drug by approximately 10-fold after intravenous administration and by 20-fold after oral administration. The relationship between the area under the plasma concentration-time curve (AUC) of morphine and the AUC of morphine-3-glucuronide remains constant during the development of tolerance upon long term treatment with increasing doses.
Renal disease causes a significant increase in the mean plasma concentrations of morphine for 15 minutes after its administration, while mean values of terminal half-life and total body clearance are within the normal range. However, the glucuronidated polar metabolite morphine-3-glucuronide rises rapidly to high concentrations which persist for several days. Chronic liver disease causes an increase in the bioavailability of oral morphine but no, or only a slight reduction in the intravenous clearance. The elimination half-life and volume of distribution are within the normal range. In the elderly, there is a reduction in the volume of distribution and the total plasma clearance, while the elimination phase is shorter compared with younger patients. Increased sensitivity has been reported in the elderly, in patients with liver disease, and patients with renal dysfunction. Consequently cautious dosing is needed in these groups of patients.
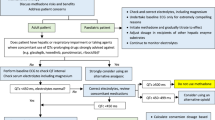
The initial dose of oral morphine is mainly determined by the patient’s previous medication. Most opiate-naive patients experience pain relief with initial oral doses of morphine of 5 to 30mg every 4 to 6 hours. The dose and/or the dose interval are adjusted according to therapeutic response evaluated at steady-state, i.e. after 4 to 5 half-lives. Continuous re-evaluation of the dosage regimen is necessary during long term treatment. Dose adjustments are recommended to be in the order of 25 to 30% of the previous dose. When switching from oral to parenteral therapy the morphine dose should be reduced by 75% and thereafter adjusted according to the individual patient’s needs.
The pharmacokinetics of oral methadone have, almost exclusively, been studied in former opiate addicts. Single-dose studies have shown methadone to be equivalent to morphine in both its potency and duration of analgesia while during repeated dosing, as a consequence of its kinetics, the duration of action will increase beyond 4 to 6 hours. Methadone is rapidly absorbed from the gastrointestinal tract and has a high oral bioavailability of about 90%. The peak plasma concentrations after administration of tablets occurred at 1 to 5 hours. The volume of distribution is approximately 4 L/kg and the plasma clearance is about 95 ml/min (5.7 L/h). The protein binding is 60 to 90% and α1-acid glycoprotein is the main binding protein and hence the determinant of the free fraction in plasma. Lower free fractions of methadone have been shown in cancer patients compared with healthy volunteers. Plasma methadone concentrations decline in a biexponential manner with an elimination half-life of 15 to 60 hours. Biotransformation as well as renal and faecal excretion are important determinants of the disposition of methadone. Studies, although non-conclusive, have indicated decreased steady-state plasma concentrations during methadone maintenance treatment. Similar to morphine, there are marked interindividual differences in the kinetics of methadone which must be taken into account in the clinical use of the drug. Although the long elimination half-life of methadone is an obvious advantage, it is difficult to titrate the minimum effective safe dose for the individual patient. In order to shorten the time to reach an analgesic effect, a loading dose regimen with dosage intervals of 4 to 6 hours has been suggested during the first 2 days of therapy. The dosage interval should thereafter be increased to 8 or 24 hours.
When switching from oral to parenteral therapy, the methadone dose should be reduced by 50% and thereafter if necessary further dose adjustment can be performed according to the individual patient’s need.
Similar content being viewed by others
References
Abramson F. Methadone plasma protein binding: alterations in cancer and displacement from α1-acid glycoprotein. Clinical Pharmacology and Therapeutics 32: 652–658, 1982
Aherne GW, Piall EM, Twycross RG. Serum morphine concentration after oral administration of diamorphine hydrochloride and morphine sulphate. British Journal of Clinical Pharmacology 8: 577–580, 1979
Aherne GW. The specificity of morphine radioimmunoassays. Royal Society Medicine Internal Congress Symposium Series 58: 21–26, 1983
Aitkenhead AR, Vater M, Achola K, Cooper CHS, Smith G. Pharmacokinetics of single-dose iv morphine in normal volunteers and patients with end-stage renal failure. British Journal of Clinical Pharmacology 56: 813–819, 1984
Änggård E, Gunne LM, Holmstrand J, McMahon RE, Sandberg CG et al. Disposition of methadone in methadone maintenance. Clinical Pharmacology and Therapeutics 17: 258–266, 1975
Axelrod J. Possible mechanism of tolerance to narcotic drugs. Science 124: 263–264, 1956
Ball M, McQuay HJ, Moore RA, Allen MC, Fisher A, et al. Renal failure and the use of morphine in intensive care. Lancet 784–786, 1985
Bell MDD, Mishra P, Weldon BD, Murray GR, Calvey TN, et al. Buccal morphine — a new route for analgesia? Lancet 1: 71–73, 1985
Baker WP, Woods LA. A study in the dog of the renal clearance of morphine and the effect of morphine on p-amino-hippurate clearance. Journal of Pharmacology and Experimental Therapeutics 120: 371–374, 1957
Baselt RC, Casarett LJ. Urinary excretion of methadone in man. Clinical Pharmacology and Therapeutics 13: 64–70, 1972
Beaver WT, Wallenstein SL, Houde RW, Rogers AA. Comparison of the analgesic effects of pentazocine and morphine in cancer patients. Clinical Pharmacology and Therapeutics 7: 740–751, 1966
Beaver WT, Wallenstein SL, Houde RW, Rogers A. A clinical comparison of the analgesic effects of methadone and morphine administered intramuscularly, and of orally and parenterally administered methadone. Clinical Pharmacology and Therapeutics 8: 415–426, 1967
Beckett AH, Taylor JF, Casy AF, Hassan MMA. The biotransformation of methadone in man: synthesis and identification of a major metabolite. Journal of Pharmacy and Pharmacology 20: 754–762, 1968
Beecher HK, Keats AS, Mosteller F, Lasagna L. The effectiveness of oral analgesics (morphine, codeine, acetylsalicylic acid) and the problem of placebo ‘reactors’ and ‘non-reactors’. Journal of Pharmacology 109: 393–400, 1953
Bellville JW, Forrest WH, Miller E. Influence of age on pain relief from analgesics. Journal of the American Medical Association 217: 1835–1841, 1971
Bennett WM, Singer I, Coggins CJ. A guide to drug therapy in renal failure. Journal of the American Medical Association 230: 1544–1553, 1974
Berkowitz BA, Ngai SH, Yang JC, Hempstead J, Spector S. The disposition of morphine in surgical patients. Clinical Pharmacology and Therapeutics 17: 629–635, 1975
Berkowitz BA. Research review: the relationship of pharmacokinetics to pharmacological activity: morphine, methadone and naloxone. Clinical Pharmacokinetics 1: 219–230, 1976
Blom Y, Bondesson U, Änggård E. Determination of morphine in biological samples by gas chromatography-mass spectrometry. Journal of Chromatography 309: 73–80, 1984
Boerner U, Abbott S, Roe R. The metabolism of morphine and heroin in man. Drug Metabolism Reviews 4: 39–73, 1975
Brunk SF, Delle M. Morphine metabolism in man. Clinical Pharmacology and Therapeutics 16: 51–57, 1974
Bullingham RES, McQuay HJ, Porter EJB, Thomas, D, Allen MC, et al. Acute iv methadone kinetics in man. Relationship to chronic studies. British Journal of Anaesthesia 54: 1271–1276, 1982
Dahlström B, Paalzow L. Quantitative determination of morphine in biological samples by gas-liquid chromatography and electron-capture detection. Journal of Pharmaceutical Pharmacology 27: 172–176, 1975
Dahlström B, Paalzow L, Segre G, Ågren AJ. Relation between morphine pharmacokinetics and analgesia. Journal of Pharmacokinetics and Biopharmaceutics 6: 41–53, 1978
Dahlström B, Tamsen A, Paalzow L, Hartvig P. Patient-controlled analgesic therapy. IV. Pharmacokinetics and analgesic plasma concentrations of morphine. Clinical Pharmacokinetics 7: 266–279, 1982
Dole VP, Kreek MJ. Methadone plasma level: sustained by a reservoir of drug in the tissue. Proceedings of the National Academy of Sciences of the United States of America 70: 10, 1973
Don HF, Dieppa RA, Taylor P. Narcotic analgesics in anuric patients. Anesthesiology 42: 745–747, 1975
Drost RH, Van Oijen RD. Determination of morphine in serum and cerebrospinal fluid by gas chromatography and selected ion monitoring after reversed-phase column extraction. Journal of Chromatography 310: 193–198, 1984
Ellison NM, Lewis GO. Plasma concentrations following single doses of morphine sulfate in oral and rectal suppository. Clinical Pharmacy 3: 614–617, 1984
Ettinger DS, Vitale PJ, Trump DL. Important clinical pharmacological considerations in the use of methadone in cancer patients. Cancer Treatment Reports 63: 457–459, 1979
Gourlay GK, Wilson PR, Glynn GJ. Pharmacodynamics and pharmacokinetics of methadone during the perioperative period. Anesthesiology 57: 458–467, 1982
Grabinski PY, Kaiko RF, Walsh TD, Foley KM, Houde RW. Morphine radioimmunoassay specificity before and after extraction of plasma and cerebrospinal fluid. Pharmacology Science 72: 27–30, 1983
Hanks GW, Thomas PJ, Truman T, Weeks E. The myth of haloperidol potentiation. Lancet 2: 523–524, 1983
Hanks GW, Aherne GW. Morphine metabolism: does the renal hypothesis hold water? Lancet 2: 221–222, 1985
Holmstrand J, Änggård E, Gunne LH. Methadone maintenance: plasma levels and therapeutic outcome. Clinical Pharmacology and Therapeutics 23: 175–180, 1978
Horns W, Rado M, Goldstein A. Plasma levels and symptom complaints in patients maintained on daily dosage of methadone hydrochloride. Clinical Pharmacology and Therapeutics 17: 636–649, 1975
Inturrisi CE, Verebely K. Disposition of methadone in man after single oral dose. Clinical Pharmacology and Therapeutics 13: 923–930, 1972a
Inturrisi CE, Verebely K. The levels of methadone in plasma in methadone maintenance. Clinical Pharmacology and Therapeutics 13: 633–637, 1972b
Iwamoto K, Klaassen C. The first pass of morphine in rats. Journal of Pharmacology and Experimental Therapeutics 200: 236–244, 1977
Jaffe JJ, Martin WR. Narcotic analgesics. In Goodman & Gilman (Eds) The pharmacological basis of therapeutics, 6th edition, pp. 494–534 MacMillan, New York, 1980
Kager L, Ljungdahl I, Rane A, Säwe J. Per oral morphine treatment of pain in terminal cancer. Läkartidningen 76: 3411–3415, 1979
Kaiko R. Age and morphine analgesia in cancer patients with postoperative pain. Clinical Pharmacology and Therapeutics 28: 823–826, 1980
Kreek MJ, Gutjahr CL, Garfield JN, Bowen DV, Field FH. Drug interactions with methadone. Annals of the New York Academy of Science 281: 350–370, 1976
Kreek MJ, Schecter AJ, Gutjahr CL, Hecht M. Methadone use in patients with chronic renal disease. Drug and Alcohol Dependence 5: 197–205, 1980
Laidlaw J, Read AE, Sherlock S. Morphine tolerance in hepatic cirrhosis. Gastroenterology 40: 389–396, 1961
Lasagna L, Kornfeld TL. Analgesic potency of normorphine in patients with postoperative pain. Journal of Pharmacology and Experimental Therapeutics 124: 260–263, 1958
Leslie ST, Rhodes A, and Black FM. Controlled release morphine sulphate tablets — a study in normal volunteers. British Journal of Clinical Pharmacology 9: 531–534, 1980
Liu SJ, Wang RIH. Effects of phenobarbital and SKF 525-A on the in vivo metabolism of morphine in rats. Drug Metabolism and Disposition 8: 260–264, 1980
Marks RM, Sachar EJ. Undertreatment of medical inpatients with narcotic analgesics. Annals of Internal Medicine 78: 173–181, 1973
Masten LW, Peterson G, Burkhalter A, Way EL. Microsomal enzyme induction by methadone and its implications on tolerance to methadone lethality. Nature 253: 200–201, 1975
Melzack R, Mount BM, Gorden JM. The Brompton mixture versus morphine solution given orally: effects on pain. Canadian Medical Association Journal 120: 435–438, 1979
Mojaverian P, Fedder IL, Vlasses PH, Heshi R, Rocci ML, et al. Cimetidine does not alter morphine disposition in man. British Journal of Clinical Pharmacology 14: 809–813, 1982
Morrison G, Soong TC, Koepke HH, Walker BR. Effect of renal impairment and hemodialysis on lorazepam kinetics. Clinical Pharmacology and Therapeutics 35: 646–652, 1984
Mount BM, Melzack R, Mackinnon KJ. The management of intractable pain in patients with advanced malignant disease. Journal of Urology 120: 720–725, 1978
Murphy MR, Hug CC. Pharmacokinetics of intravenous morphine in patients anesthetized with enflurane-nitrous oxide. Anesthesiology 54: 187–192, 1981
Neal EA, Meffin PJ, Gregory PB, Blaschke TF. Enhanced bioavailability and decreased clearance of analgesics in patients with cirrhosis. Gastroenterology 77: 96–102, 1979
Neumann PB, Henriksen H, Grosman N, Christensen CB. Plasma morphine concentrations during chronic oral administration in patients with cancer pain. Pain 13: 247–252, 1982
Nilsson MJ. Clinical pharmacokinetics of methadone. Academic Thesis of Uppsala University, Uppsala, Sweden, 1982
Nilsson MJ, Änggard E, Holmstrand H, Gunne LM. Pharmacokinetics of methadone during maintenance treatment: Adaptive changes during the induction phase. European Journal of Clinical Pharmacology 22: 343–349, 1982a
Nilsson MJ, Widelöv E, Meresaar U, Änggård E. Effect of urinary pH on the disposition of methadone in man. European Journal of Clinical Pharmacology 22: 337–342, 1982b
Novic DM, Kreek MJ, Fanizza AH, Yancovitz SR, Gelb AM, et al. Methadone disposition in patients with chronic liver disease. Clinical Pharmacology and Therapeutics 30: 353–362, 1981
Odar-Cederlöf I, Vessman J, Alván G, Sjöqvist F. Oxazepam disposition in uremic patients. Acta Pharmacologica et Toxicologica 40: 52–62, 1977
Olsen GD. Methadone binding to human plasma proteins. Clinical Pharmacology and Therapeutics 14: 338–343, 1973
Olsen GD. Morphine binding to human plasma proteins. Clinical Pharmacology and Therapeutics 17: 31–35, 1975
Owen JA, Sitar DS, Berger L, Brownell L, Duke PC, et al. Age related morphine kinetics. Clinical Pharmacology and Therapeutics 34: 364–368, 1983
Paalzow L, Nilsson L, Stenberg P. Pharmacokinetic basis for optimal methadone treatment of pain in cancer patients. Acta Anaesthesiologica Scandinavica 74 (Suppl.): 55–58, 1982
Pacifici GM, Rane A. Distribution of UDP-glucuronyltransferase in different human foetal tissues. British Journal of Clinical Pharmacology 13: 732–735, 1982
Patwardhan RV, Johnsson RF, Hoyumpa A, Sheehan JJ, Desmond PV, et al. Normal metabolism of morphine in cirrhosis. Gastroenterology 81: 1006–1011, 1981
Regnard C, Twycross RG. Metabolism of narcotics. British Medical Journal 288: 860, 1984
Romach MK, Piafsky KM, Abel JG, Khouw V, Sellers EM. Methadone binding to orosomucoid (α1-acid glycoprotein). Determinant of free fraction in plasma.Clinical Pharmacology and Therapeutics 29: 211–217, 1981
Saunders CM. The challenge of terminal care. In Symington T & Carter RL (Eds) Scientific foundations of oncology, pp. 673–679, William Heinemann Medical Books, London, 1976
Säwe J, Dahlström B, Rane A. Morphine kinetics in cancer patients. Clinical Pharmacology and Therapeutics 30: 629–635, 1981a
Säwe J, Hansen J, Ginman C, Hartvig P, Jakobsson PA, et al. Patient-controlled dose regimen of methadone for chronic cancer pain. British Medical Journal 282: 771–779, 1981b
Säwe J, Pacifici GM, Kager L, von Bahr O, Rane A. Glucuronidation of morphine in human liver and interaction with oxazepam. Acta Anaesthesia Scandinavica 74 (Suppl.): 47–51, 1982
Säwe J, Svensson JO, Rane A. Morphine metabolism in cancer patients on increasing oral doses — no evidence for autoinduction or dose-dependence. British Journal of Clinical Pharmacology 16: 85–93, 1983
Säwe J. Oral morphine and methadone in the treatment of cancer pain. Clinical pharmacokinetic studies. Doctoral thesis at the Karolinska Institute, Stockholm, Sweden, 1984
Säwe J. Morphine and its 3- and 6-glucuronides during chronic oral administration in cancer patients. Advances in Pain Research and Therapy. In press, 1985
Säwe J, Svensson JO, Odar-Cederlöf I. Kinetics of morphine in patients with renal failure. Lancet 2: 211, 1985a
Säwe J, Kager L, Svensson JO, Rane A. Comparison of in vivo and in vitro glucuronidation of morphine in cancer patients. British Journal of Clinical Pharmacology 19: 495–501, 1985b
Schäli C, Roch-Ramel F. Transport and metabolism of (3H)-morphine in isolated nonperfused proximal tubular segments of the rabbit kidney. Journal of Pharmacology and Experimental Therapeutics 223: 811–815, 1982
Spector S, Vesell ES. Disposition of morphine in man. Science 174: 421–422, 1971
Stanski DR, Greenblatt DJ, Lappas DG, Koch-Weser J, Lowenstein E. Kinetics of high-dose intravenous morphine in cardiac surgery patients. Clinical Pharmacology and Therapeutics 19: 752–756, 1976
Stanski DR, Greenblatt DJ, Lowenstein E. Kinetics of intravenous and intramuscular morphine. Clinical Pharmacology and Therapeutics 24: 52–59, 1978
Svensson JO, Rane A, Säwe J, Sjöqvist F. Determination of morphine, morphine-3-glucuronide and (tentatively) morphine-6-glucuronide in plasma and urine using ion-pair high-performance liquid chromatography. Journal of Chromatography 230: 427–432, 1982
Symonds P. Methadone and the elderly. British Medical Journal 1: 512, 1977
Tamsen A. Patient-controlled analgesic therapy. Doctoral thesis at the University of Uppsala, Sweden, 1981
Todd R, Muldoon SM, Watson RL. Determination of morphine in cerebrospinal fluid and plasma by high performance liquid chromatography with electrochemical detection. Journal of Chromatography 232: 101–110, 1982
Twycross RG. Clinical experience with diamorphine in advanced malignant disease. International Journal of Clinical Pharmacology, Therapy and Toxicology 9: 184–198, 1974
Twycross RG. A comparison of diamorphine with cocaine and methadone. British Journal of Clinical Pharmacology 4: 691–693, 1977
Twycross RG. Relief of pain. In Saunder CM (Ed.) The management of terminal disease, pp. 65–92, Edward Arnold, London, 1978
Twycross RG. Morphine and diamorphine in the terminally ill patient. Acta Anaesthesiologica Scandinavica 74 (Suppl.): 128–134, 1982
Twycross RG, Wald SJ. Long-term use of diamorphine in advanced cancer. In Bonica JJ & Albert-Fessard D (Eds) Advances in pain research therapy, Vol. 1, Raven Press, New York, 1976
Vater M, Smith G, Aherne GW, Aitkenhead AR. Pharmacokinetics and analgesic effect of slow-release oral morphine sulphate in volunteers. British Journal of Anaesthesiology 56: 821–827, 1984
Verebely K, Volavka J, Mulé S, Resnick R. Methadone in man: pharmacokinetic and excretion studies in acute and chronic treatment. Clinical Pharmacology and Therapeutics 18: 180–190, 1975
Westerling D, Lindahl S, Andersson KE, Andersson A. Absorption and bioavailability of rectally administered morphine in women. European Journal of Clinical Pharmacology 23: 59–64, 1982
Yeh SY. Urinary excretion of morphine and its metabolites in morphine-dependent subjects. Journal of Pharmacology and Experimental Therapeutics 192: 201–210, 1975
Yoshimura H, Ida S, Oguri K, Tsukamoto H. Biochemical basis for analgesic activity of morphine-6-glucuronide. I. Penetration of morphine-6-glucuronide in the brain of rats. Biochemical Pharmacology 22: 1423–1430, 1973
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Säwe, J. High-Dose Morphine and Methadone in Cancer Patients. Clin-Pharmacokinet 11, 87–106 (1986). https://doi.org/10.2165/00003088-198611020-00001
Published:
Issue Date:
DOI: https://doi.org/10.2165/00003088-198611020-00001