Associating liver partition and portal vein ligation for bleeding hepatocellular carcinoma in HBV cirrhosis: a safety strategy
Introduction
One of the most fatal complications of hepatocellular carcinoma (HCC) is spontaneous tumor rupture; the incidence varies between 3% and 26% (1). HCC rupture is worldwide decreasing thanks to ultrasound screening, however it remains a significant health problem in Eastern Asia with mortality rates are as high as 25–100% (2). For resectable HCC ruptures, emergency hepatectomy or staged hepatectomy after transcatheter arterial embolization (TAE) are life-saving procedures, and efficient therapeutic methods (3). Associating liver partition and portal vein ligation (ALPPS) for HCC has been reported to be safe even in patients with portal vein tumor thrombosis (PVTT) (4,5).
We report a multimodal therapy including TAE, ALPPS and immunoglobuline infusion for a huge bleeding HCC with PVTT in hepatitis B virus (HBV) cirrhosis.
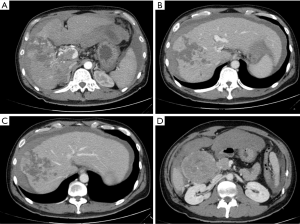
A 35 years old Chinese man was admitted to an emergency center for abdominal pain. BMI was 23. Blood exams an anemia was noted (9.3 g/dL), platelets were 386,000. A computed tomography was performed and a 7 cm nodule at segment VII was described with multiple necrotic nodules in the right liver (Figure 1). A Vp4 PVTT and a free intra-abdominal hemorrhage were described too. Hepatitis markers were negative for HCV and positive for HBV (4,352.00 UI). Patient was a Child A, Meld 14. Due to the hemodynamic instability a TAE was performed. In order to secure the left portal flow an ALPPS procedure was proposed to the patient two days after TAE.
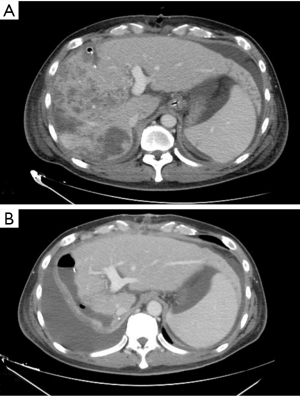
ALPPS first step began with an abdominal toilette due to the massive hemoperitoneum. Afterwards a mobilization of the huge HCC was necessary to control the hepatic hilum easily. A vessel loop was passed around left, right and portal vein trunk. A portal vein incision at the bifurcation of the right and left portal veins was performed. A freely floating left part of the thrombus was extracted from the left portal vein in order to restore the left portal vein. A 5/0 prolene left portal vein suture was done and portal flow was restore. A US-Doppler confirmed the correct left portal flow without presence of thrombosis. The right portal vein with complete thrombosis was closed. Liver partition was then performed. Postoperative first step CT confirmed the left portal vein patency (Figure 2A). Entecavir therapy was started since the first postoperative day with an intention to reduce the HBV DNA between the two surgical steps. The second step of ALPPS was performed 4 days after the first one. Surgery was uneventful. Pathological exam described a 90 mm ×70 mm ×50 mm nodule with multiple nodules in the right liver. A HCC Edmondson grade 4 (pT3b) and a cirrhotic liver parenchyma were described. Postoperative ascites decompensation (Figure 2B) was treated and patient was discharged in postoperative day 21.
First treatment in case of ruptured HCC is hemostasis. Staged hepatectomy after TAE decreases the mortality rate in these patients (6,7).
ALPPS for HCC has been successfully described as safe even in patient with PVTT and cirrhosis (6-9). Furthermore ALPPS for huge HCC has been reported without an increased risk of morbidity or mortality (10). In the reported case, a multimodal therapy was the winning strategy. As recommended a TAE was performed in order to control the HCC bleeding. One time the hemodynamic stability was obtained according with the high vascular risk with the PVTT an ALPPS procedure was planned. The first step was performed to have a vascular control and secure the left portal flow without which surgery would be useless. In addition to this we treated the HBV infection between the two steps. The second ALPPS step was a routinely one. The reported triple strategy allowed us to prolong patient live. Liver resection is associated with a longer survival outcome than non-surgical treatment in HCC patients with PVTT (11). Nevertheless, a Vp4 PVTT is a negative prognostic factor for patient survival and surgical resection remain debated (11).
In conclusion, a multimodal therapy including TAE, ALPPS and immunoglobuline is a good option for a life treatment in case of huge bleeding hepatocellular carcinoma with PVTT in HBV cirrhosis.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patients for publication of this manuscript and any accompanying images.
References
- Zhong F, Cheng XS, He K, et al. Treatment outcomes of spontaneous rupture of hepatocellular carcinoma with hemorrhagic shock: a multicenter study. Springerplus 2016;5:1101. [Crossref] [PubMed]
- Lin HM, Lei LM, Zhu J, et al. Risk factor analysis of perioperative mortality after ruptured bleeding in hepatocellular carcinoma. World J Gastroenterol 2014;20:14921-6. [Crossref] [PubMed]
- Ou D, Yang H, Zeng Z, et al. Comparison of the prognostic influence of emergency hepatectomy and staged hepatectomy in patients with ruptured hepatocellular carcinoma. Dig Liver Dis 2016;48:934-9. [Crossref] [PubMed]
- Vennarecci G, Laurenzi A, Santoro R, et al. The ALPPS procedure: a surgical option for hepatocellular carcinoma with major vascular invasion. World J Surg 2014;38:1498-503. [Crossref] [PubMed]
- Levi Sandri GB, Lai Q, Rayar M, et al. ALPPS procedure for hepatocellular carcinoma with macrovascular thrombosis: a new opportunity? J Hepatol 2015;62:241-2. [Crossref] [PubMed]
- Yang T, Sun YF, Zhang J, et al. Partial hepatectomy for ruptured hepatocellular carcinoma. Br J Surg 2013;100:1071-9. [Crossref] [PubMed]
- Tanaka S, Kaibori M, Ueno M, et al. Surgical Outcomes for the Ruptured Hepatocellular Carcinoma: Multicenter Analysis with a Case-Controlled Study. J Gastrointest Surg 2016;20:2021-34. [Crossref] [PubMed]
- Chan AC, Poon RT, Chan C, et al. Safety of ALPPS Procedure by the Anterior Approach for Hepatocellular Carcinoma. Ann Surg 2016;263:e14-6. [Crossref] [PubMed]
- Vennarecci G, Laurenzi A, Levi Sandri GB, et al. The ALPPS procedure for hepatocellular carcinoma. Eur J Surg Oncol 2014;40:982-8. [Crossref] [PubMed]
- Torres OJ, Vasques RR, Silva TH, et al. The ALPPS procedure for hepatocellular carcinoma larger than 10 centimeters. Int J Surg Case Rep 2016;26:113-7. [Crossref] [PubMed]
- Kokudo T, Hasegawa K, Matsuyama Y, et al. Survival benefit of liver resection for hepatocellular carcinoma associated with portal vein invasion. J Hepatol 2016;65:938-43. [Crossref] [PubMed]
Cite this article as: Levi Sandri GB, Vennarecci G, Lepiane P, Ettorre GM. Associating liver partition and portal vein ligation for bleeding hepatocellular carcinoma in HBV cirrhosis: a safety strategy. Transl Gastroenterol Hepatol 2017;2:20.


