
Does previous unsuccessful shockwave lithotripsy influence the outcomes of ureteroscopy?—a systematic review and meta-analysis
Introduction
The urinary stone disease prevalence varies from 1% to 20% (1). In some economically developed countries such as Sweden, Canada or the USA, the prevalence rates for renal stone surpass 10% (2). Stone incidence can differ on the basis of geographical, dietary, climatic, ethnic and genetic factors. Currently, shockwave lithotripsy (SWL) and ureteroscopy (URS) are two common treatment options for the management of urinary stone disease. SWL might be conducted as an outpatient procedure and no standard antibiotic prophylaxis is recommended. URS is usually conducted as an inpatient procedure under regional or general anesthesia (3) and peri-operative antibiotic prophylaxis should be offered to all patients (1). SWL is less-invasive and associated with a lower complication rate compared to URS, but the stone-free rate (SFR) of SWL was significantly affected by factors such as stone characteristics (size, location and hardness), patient’s habitus and performance of SWL (shockwave rate, energy setting and repeat treatment sessions) (4-6). The case is deemed SWL-resistant if no fragmentation occurs after two SWL sessions. In clinical practice, URS is often employed as salvage therapy in SWL-resistant stones. However, only a few studies (7-13) have determined the impact of previous unsuccessful SWL on the outcomes of URS with conflicting results. Holland et al. reported that URS was associated with a lower SFR and higher complication rate when performed after unsuccessful SWL (7). Irer et al. also demonstrated that complications were significantly higher in patients with a previous SWL (8). In contrast, several studies showed that previous failed SWL had no impact on the SFR and complications of URS (9-13). Therefore, we conducted a meta-analysis, for the first time, to compare the outcomes of URS performed as a primary procedure (SWL−) and salvage URS (SWL+) after failed SWL. This study adhered to the Cochrane standards and PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines (PROSPERO CRD42020213633) (14) (available at http://dx.doi.org/10.21037/tau-21-39).
Methods
Search strategy
An exhaustive search of PubMed, EMBASE, Web of Science and Cochrane Library were conducted to find eligible studies before September 2020. The following key words were used: “previous” or “failed” or “failure” or “complementary” or “unsuccessful” and “ureteroscopy” or “URS” or “RIRS” and “ESWL” or “shockwave lithotripsy” or “SWL”. Additional studies were searched by the references of relevant articles.
Inclusion criteria and exclusion criteria
All eligible articles were selected on the basis of the following criteria: (I) patients who were diagnosed with renal or ureteral stones; (II) studies determining the safety and effectiveness of URS with or without a previous failed SWL; (III) researches reporting on ≥1 of the following variables: Stone-free rate (SFR), operation time, complications; d. researches on rigid and flexible URS.
The exclusion criteria were: (I) congenital anatomic abnormalities, previous ureteral strictures and malignancy; (II) previous URS, laparoscopy and open surgery; (III) non-comparative articles, review, case reports or comments.
Data extraction
Two reviewers (WW and LP) independently extracted the following items: author, publication date, country; study design, level of evidence (LE); interventions; number of individuals; demographics; body mass index (BMI); laterality and stone size; Hounsfield unit; stone location; impacted stones (stones that were immobilized and surrounded by excessive mucosa edema were defined as impacted stones under endoscopic visualization); lithotripter type; ureteral stenting; SFR (the definition of SFR was complete stone clearance or maximum residual fragment ranging from 2 to 4 mm); operation time (the definition of operation time was the time from the placement of safety guidewire to the end of the procedure, or the duration between the insertion of cystoscope and the placement of double J stent); complications [complications were graded based on modified Clavien system (15)]. Patients who diagnosed with ureteral stones were regarded as SWL-resistant if stone persistence was noticed 2 weeks after the second SWL session. Patients with renal stones were considered SWL-resistant if stone persistence was noticed 2–4 weeks after the third session. Disagreements were resolved by discussing with the third reviewer (XW).
Quality assessment
Two authors (WW and LP) evaluated all relevant clinical studies independently for methodological quality and levels of evidence (LE), and the disagreements were solved by discussion. The Oxford Centre for Evidence-Based Medicine was used to estimate the LE of each eligible study (16). We evaluated the methodological quality of eligible case-control trials (CCTs) on the basis of Newcastle Ottawa Scale (NOS) (17). In addition, the Risk of Bias in Non-randomized Studies-of Interventions (ROBINS-I) were employed to identify confounding factors for non-randomized studies (18).
Statistical analysis
Review Manager Version 5.3 software was utilized to conduct analysis. Dichotomous variables were displayed using the odds ratio (OR) and 95% confidence interval (CI), and continuous variables were presented by the weighted mean difference (WMD) and 95% CI. The P value was calculated from the Z-test, and a P≤0.05 was deemed as statistically significant. The heterogeneity of the included studies was assessed by Q and I2 statistics. The P value higher than 0.1 and I2 lower than 50% were considered as low heterogeneity among studies, and the fixed-effects model was performed; if not, demonstrated high heterogeneity, and the random-effects model was conducted. We used a single-item removal method to perform sensitivity analysis. Funnel plot was performed to assess publication bias.
Results
Study selection
According to the literature search and the inclusion criteria, 243 studies were initially identified, and ultimately, 7 studies (7-13) were incorporated in our analysis, 1,096 patients undergoing URS after a failed SWL [SWL (+)] and 1317 patients treated with URS primarily [SWL (−)]. The process of literature selection was presented in Figure 1.
Study characteristics and assessment of quality
Seven studies (7-13) were finally included, all of which were CCT (LE:3b). Table 1 presented the characteristics of the eligible researches. Patients were diagnosed with renal stones in 4 studies (7,10,11,13) or ureteral stones in 3 studies (8,9,12). The placement of the access sheath was routinely performed in all patients in 3 studies (7,11,13), and was conducted only if needed in 2 studies (8,10). A double-J stent was placed in all patients in 4 studies (7,9,11,13), and was not routinely used, but only in cases with relevant clinical indications in 3 studies (8,10,12). The fragments were removed employing basket for intrarenal stones or grasping forceps for ureteral stones. In addition, the methodological quality of eligible 7 CCTs were demonstrated in the Table S1. On the whole, the methodological quality of included studies was relatively high (NOS: six to eight out of nine points) (Table S1). Additionally, the ROB of seven non-randomized studies were presented in the Table S2, and the overall ROB judgement of included studies was moderate to serious. We performed the forest plots to determine the effectiveness of URS with or without a previous failed SWL.
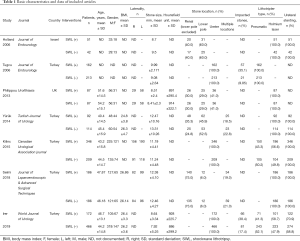
Full table
Stone-free rate
Seven studies (7-13) were included in the forest plot of SFR. Definition of SFR was complete stone clearance or a maximum residual fragment ranging from 2 to 4 mm. Detections (Kidneys-Ureters-Bladder radiography, ultrasound, and abdominal computed tomography scan) were performed at postoperative 1–3 months. The heterogeneity was low (P=0.60, I2=0%), and fixed-effects model displayed that the SWL (+) and SWL (−) group were statistically similar concerning SFR (OR: 0.84; 95% CI: 0.67, 1.06; P=0.15; Figure 2).
Operation time
The definition of operation time was the time from the placement of the safety guidewire to the end of the procedure (8), or the duration between the insertion of cystoscope and the placement of double J stents (11,13). Six studies (8-13) provided data concerning the operation time. The heterogeneity was high (P<0.00001, I2=99%), and random-effects model demonstrated that no statistically difference exists between SWL (+) and SWL (−) group. (WMD: 6.79; 95% CI: −3.25, 16.82; P=0.19; Figure 3).
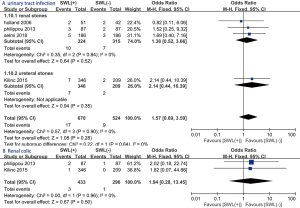
Modified Clavien grade I complications
No statistically significant difference was seen regarding the following modified Clavien grade I complications: fever (OR: 1.36; 95% CI: 0.74, 2.49; P=0.32; Figure 4A), hematuria (OR: 0.81; 95% CI: 0.23, 2.90; P=0.75; Figure 4B).
Modified Clavien grade II complications
Two groups were statistically similar concerning the following modified Clavien grade II complications: urinary tract infection (OR: 1.57; 95% CI: 0.69, 3.59; P=0.28; Figure 5A), renal colic (OR: 1.94; 95% CI: 0.28, 13.45; P=0.50; Figure 5B).
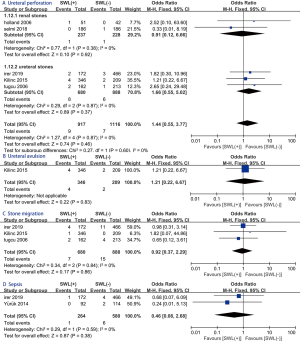
Modified Clavien grade III–IV complications
No statistically significant difference exists between SWL (+) and SWL (−) group with regard to the following modified Clavien grade III–IV complications: ureteral perforation (OR: 1.44; 95% CI: 0.55, 3.77; P=0.46; Figure 6A), ureteral avulsion (OR: 1.21; 95% CI: 0.22, 6.67; P=0.83; Figure 6B), stone migration (OR: 0.92; 95% CI: 0.37, 2.29; P=0.86; Figure 6C), sepsis (OR: 0.46; 95% CI: 0.08, 2.68; P=0.38; Figure 6D).
Sensitivity analysis and publication bias
Sensitivity analysis of the variable with greater heterogeneity was performed by the removal of the single study. When it was applied to operation time, the results demonstrated that the reduction of heterogeneity was not significant. Additionally, we utilized funnel plot to estimate publication bias, and the symmetrical distribution displayed no obvious evidence of publication bias (Figure S1).
Discussion
In the present study, we compared the outcomes of URS performed as a primary procedure and salvage URS after failed SWL. We found that no statistically significant difference existed between SWL (−) and SWL (+) URS group regarding SFR, operation time and modified Clavien grade I–IV complication rate, demonstrating that the outcomes of URS were not affected by previous unsuccessful SWL.
SWL and URS are the commonly performed procedure for the surgical management of urinary stones. EAU 2020 guidelines recommended that the SWL is the first-line treatment option for kidney stones <20 mm or ureteral stones <10 mm (1). It is less-invasive compared to URS, and can be conducted as an outpatient procedure without the need for general anesthesia; its shortcomings consist a high re-treatment rate and unable to dissect large or impacted stones (19). The acute pelvic-lower pole infundibular angle, long calyceal neck and narrow infundibulum negatively affect the outcomes of SWL (20). In addition, the efficacy of SWL might be decreased by stone-related variables such as stone size, stone location and stone composition. It was reported that the SFR of SWL for stones 5 to 10mm in diameter was 85.8% to 90.4% (21). The success rates decreased to 70.4% for stones 11 to 15 mm in diameter and 53.1% for stones 16 to 20 mm in diameter (22). The efficacy of SWL also differs in upper, middle and lower-pole stones (22). Moreover, urinary stones composed of calcium oxalate monohydrate, brushite and cystine are especially hard and are usually SWL-resistant. Therefore, SWL failure is not rare in the clinical practices. Although URS has been widely used as the salvage procedure for unsuccessful SWL, the efficacy and safety of salvage URS are not well-established.
No statistically significant difference concerning SFR was observed between the salvage and primary URS group according to our findings. Holland et al. noticed a statistically significant lower SFR for salvage URS compared to primary URS (7). They attributed their relatively low success rate to anatomical parameters and partially fragmented stones that embedded in the renal mucosa (5). In terms of anatomical parameters in their study, 60% of the included patients were diagnosed with lower-pole stones. The anatomical parameters that negatively impacted the outcomes of SWL might also decrease the success rate of URS for lower-pole stones (23). However, the improvement of flexible ureteroscopes with clearer vision and elevated flexibility allows urologists to access the whole collecting system. Together with improved laser fibers and stone retrieval devices, it becomes feasible to smash and clear stones in almost every location. From the perspective of stones embedded in the mucosa, some previous studies did report that SWL-related injury involved the entire renal structures from the cortex to the medulla (24). Tubular destruction, cell vacuolization and membrane blebbing were observed in SWL-treated kidneys (24). As a consequence, residual fragments might become embedded in the mucosa and was covered with pseudo-membranes as part of the healing process. This is also the reason why the percentage of impacted stones in the salvage URS group was statistically higher than the primary URS group in the two of the included studies (35.1% vs. 9.85% and 38.4% vs. 17.4%, respectively). Unfavorable anatomical parameters and pseudo-membranes covering residual stones might make it more difficult to perform URS, but do not necessarily negatively affect the outcomes.
Auxiliary treatment rate is a crucial factor to evaluate the effectiveness of endoscopic stone surgery. However, only two studies (7,10) presented this data. We gave up pooled the auxiliary rate for meta-analysis. Holland et al. reported that the auxiliary procedure rate was 20% and 33% in the SWL (−) and SWL (+) group, respectively (7). This difference was not statistically significant (P=0.176, Chi square test). Additionally, 20.7% of patients in the SWL (+) and 12.6% in the SWL (−) group underwent an auxiliary procedure, but the difference was statistically similar (P=0.154) (10). Therefore, we concluded that the auxiliary treatment rate is similar between two groups. Future studies with larger sample sized are needed to further evaluate the auxiliary procedure rate between SWL (−) and SWL (+) group.
In our study, we observe similar operation time between salvage and primary URS group with high heterogeneity. Two included studies (11,13) defined operation time as the duration between insertion of cystoscope and the double-J stent placement, and one study (8) recorded the time from the placement of safety guidewire to the end of the procedure. Other included studies did not give a clear definition of operation time. Additionally, only one study (9) clearly reported surgical experience of urologists while others did not state. Different definition of operation time and surgical experience accounted for high heterogeneity among studies. On the one hand, Philippou et al. noticed statistically lower total laser energy used in salvage URS compared to primary URS group (10), which indicated partial fragmented stones by previous SWL resulted in less time spent for stone fragmentation. On the other hand, pseudo-membranes covering residual stones aforementioned increased the technical difficulty of URS, leading to a more prolonged procedure. Therefore, the operation time of the two groups was similar when takes it together. However, future high-quality studies clearly and uniformly defining operation time are needed to support our findings.
We graded postoperative complications on the basis of the modified Clavien system (15), and presented pooled results in a specific complication manner for more precisely and accurately assessment of safety. Postoperative fever was most commonly observed in both group patients with the incidence of 2.3–3.0%. Somani and colleagues reported 1.72% of patients had postoperative fever after URS (25), which is comparable to our results. Hematuria, urinary tract infection and renal colic were common complications after SWL, and due to the minimally invasive nature of URS procedure, these complications were well managed by conservative or medical treatment.
A recent study assessing the postoperative complications of URS in 11,885 patients showed a Clavien grade I–II rate of 2.8%, and only 0.5–0.1 of Clavien grade III–IV (26). In our findings, the overall postoperative Clavien grade III–IV were 0.09% and 0.1% of salvage and primary URS group, respectively. Nine patients in salvage URS and 7 patients in the primary group developed ureteral perforation postoperatively. These patients were managed by the placement of double-J catheters and no additional treatment was needed. 1.0–1.6% of our patients developed stone migration, and they required re-operation, which is slightly higher than a previous study that reported an incidence of 0.4% for stone migration demanding repeat procedure (27). Aridogan and colleagues demonstrated a statistically higher stone migration rate in the proximal ureter (29%) compared to stones located in mid (11%) and distal (5.5%) ureter (28). The ureteral avulsion is a rare but serious complication, particularly if it is underestimated or misdiagnosed. The management choices consist end-to-end anastomosis, reimplantation and pyeloplasty (29). In addition, the urosepsis observed in 1 patient of salvage URS and 6 patients of primary URS group was treated with parenteral antibiotics and supportive measures. Therefore, previous failed SWL did not have a negative impact on the complications of URS.
The double J stent was routinely placed in all patients in four of our included studies (7,9,11,13), and two other researches (8,10) only used ureteral J stents in patients who had relevant clinical indication. They observed a statistically higher ureteral J stent rate in salvage URS group (8,10). This might be explained by that previous failed SWL-related mucosal edema resulted in a more challenging URS procedure, which makes stents placement necessary.
The present study still has some limitations. Firstly, all of our included studies were retrospective and non-randomized, which might bring about selection bias. Secondly, only three out of seven studies give a clear definition of operation time (8,11,13), and the definition was inconsistent. The pooled result for operation time should be interpreted with caution as high heterogeneity among included studies. Thirdly, patients were diagnosed with ureteral stones in three studies (8,9,12), while the others with renal stones were also included in our analysis. However, we subdivided SFR into renal stones and ureteral stones group with low heterogeneity. Thus, we think our results are convincible enough to provide evidence for urologists. Fourthly, none of our included studies presented the corresponding surgical outcomes according to the number of previous failed SWL. We cannot evaluate whether there exist differences between the cases with different number of previous SWL. Next, the duration between diagnosis and surgical management can be delayed in the SWL (+) compared to SWL (−) group. It might affect peri-operative renal function, but none of our included studies provided this data. Last but not least, most of our included studies did not present the data of Hounsfield unit, which is a critical influencing factors for the success rate. Future high-quality studies with rigorous design are needed to support our findings.
Conclusions
The salvage URS after previous unsuccessful SWL in urinary stones is equally effective and safe to primary URS, and they have similar operation time, except for the increased possibility for double J stent placement.
Acknowledgments
Funding: This study was supported by the Special Fund for Science and Technology Cooperation between Sichuan University and Panzhihua (2018CDPZH-29).
Footnote
Reporting Checklist: The authors have completed the PRISMA reporting checklist. Available at http://dx.doi.org/10.21037/tau-21-39
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/tau-21-39). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Türk C, Neisius A, Petřík A, et al. EAU Guidelines on Urolithiasis 2020. European Association of Urology Guidelines. 2020 Edition. Arnhem, The Netherlands: The European Association of Urology Guidelines Office, 2020.
- Stamatelou KK, Francis ME, Jones CA, et al. Time trends in reported prevalence of kidney stones in the United States: 1976-1994. Kidney Int 2003;63:1817-23. [Crossref] [PubMed]
- Wang W, Gao X, Ma Y, et al. Regional vs. General Anesthesia for Retrograde Intrarenal Surgery: A Systematic Review and Meta-Analysis. J Endourol 2020;34:1121-8. [Crossref] [PubMed]
- Connors BA, Evan AP, Blomgren PM, et al. Extracorporeal shock wave lithotripsy at 60 shock waves/min reduces renal injury in a porcine model. BJU Int 2009;104:1004-8. [Crossref] [PubMed]
- Honey RJ, Ray AA, Ghiculete D, et al. Shock wave lithotripsy: a randomized, double-blind trial to compare immediate versus delayed voltage escalation. Urology 2010;75:38-43. [Crossref] [PubMed]
- Yilmaz E, Batislam E, Basar M, et al. Optimal frequency in extracorporeal shock wave lithotripsy: prospective randomized study. Urology 2005;66:1160-4. [Crossref] [PubMed]
- Holland R, Margel D, Livne PM, et al. Retrograde intrarenal surgery as second-line therapy yields a lower success rate. J Endourol 2006;20:556-9. [Crossref] [PubMed]
- Irer B, Sahin MO, Erbatu O, et al. Impact of previous SWL on ureterorenoscopy outcomes and optimal timing for ureterorenoscopy after SWL failure in proximal ureteral stones. World J Urol 2020;38:769-74. [Crossref] [PubMed]
- Kilinc MF, Doluoglu OG, Karakan T, et al. Ureteroscopy in proximal ureteral stones after shock wave lithotripsy failure: Is it safe and efficient or dangerous? Can Urol Assoc J 2015;9:E718-22. [Crossref] [PubMed]
- Philippou P, Payne D, Davenport K, et al. Does previous failed ESWL have a negative impact of on the outcome of ureterorenoscopy? A matched pair analysis. Urolithiasis 2013;41:531-8. [Crossref] [PubMed]
- Selmi V, Sarı S, Çakıcı M, et al. Does Previous Failed Shockwave Lithotripsy Treatment Have an Influence on Retrograde Intrarenal Surgery Outcome? J Laparoendosc Adv Surg Tech A 2019;29:627-30. [Crossref] [PubMed]
- Tugcu V, Gürbüz G, Aras B, et al. Primary ureteroscopy for distal-ureteral stones compared with ureteroscopy after failed extracorporeal lithotripsy. J Endourol 2006;20:1025-9. [Crossref] [PubMed]
- Yürük E, Binbay M, Akman T, et al. Previous shock-wave lithotripsy treatment does not impact the outcomes of flexible ureterorenoscopy. Turk J Urol 2014;40:211-5. [Crossref] [PubMed]
- Shamseer L, Moher D, Clarke M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: elaboration and explanation. Bmj 2015;350:g7647. [Crossref] [PubMed]
- Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 2004;240:205-13. [Crossref] [PubMed]
- Peng L, Wang W, Gao X, et al. Fluoroless versus conventional ureteroscopy for urinary stones: a systematic review and meta-analysis. Minerva Urol Nefrol 2020; [Epub ahead of print]. [Crossref] [PubMed]
- Dalla Volta A, Valcamonico F, Zamboni S, et al. Is androgen deprivation therapy protective against SARS-CoV-2 infection and related complications in prostate cancer patients? Minerva Urol Nefrol 2020;72:778-9. [Crossref] [PubMed]
- Sterne JA, Hernán MA, Reeves BC, et al. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ 2016;355:i4919. [Crossref] [PubMed]
- Bader MJ, Eisner B, Porpiglia F, et al. Contemporary management of ureteral stones. Eur Urol 2012;61:764-72. [Crossref] [PubMed]
- Sampaio FJ, D'Anunciação AL, Silva EC. Comparative follow-up of patients with acute and obtuse infundibulum-pelvic angle submitted to extracorporeal shockwave lithotripsy for lower caliceal stones: preliminary report and proposed study design. J Endourol 1997;11:157-61. [Crossref] [PubMed]
- Demirbas M, Samli M, Karalar M, et al. Extracorporeal shockwave lithotripsy for ureteral stones: twelve years of experience with 2836 patients at a single center. Urol J 2012;9:557-61. [PubMed]
- Chung VY, Turney BW. The success of shock wave lithotripsy (SWL) in treating moderate-sized (10-20 mm) renal stones. Urolithiasis 2016;44:441-4. [Crossref] [PubMed]
- Grasso M, Ficazzola M. Retrograde ureteropyeloscopy for lower pole caliceal calculi. J Urol 1999;162:1904-8. [Crossref] [PubMed]
- Shao Y, Connors BA, Evan AP, et al. Morphological changes induced in the pig kidney by extracorporeal shock wave lithotripsy: nephron injury. Anat Rec A Discov Mol Cell Evol Biol 2003;275:979-89. [Crossref] [PubMed]
- Somani BK, Giusti G, Sun Y, et al. Complications associated with ureterorenoscopy (URS) related to treatment of urolithiasis: the Clinical Research Office of Endourological Society URS Global study. World J Urol 2017;35:675-81. [Crossref] [PubMed]
- de la Rosette J, Denstedt J, Geavlete P, et al. The clinical research office of the endourological society ureteroscopy global study: indications, complications, and outcomes in 11,885 patients. J Endourol 2014;28:131-9. [Crossref] [PubMed]
- Tepeler A, Resorlu B, Sahin T, et al. Categorization of intraoperative ureteroscopy complications using modified Satava classification system. World J Urol 2014;32:131-6. [Crossref] [PubMed]
- Aridogan IA, Zeren S, Bayazit Y, et al. Complications of pneumatic ureterolithotripsy in the early postoperative period. J Endourol 2005;19:50-3. [Crossref] [PubMed]
- Cindolo L, Castellan P, Primiceri G, et al. Life-threatening complications after ureteroscopy for urinary stones: survey and systematic literature review. Minerva Urol Nefrol 2017;69:421-31. [PubMed]






