The protocol for the Prospective Urban Rural Epidemiology China Action on Spine and Hip status study
Introduction
Osteoporosis is a systematic skeletal disorder characterized by low bone mass and microarchitectural deterioration of bone tissue, with a consequent increase in the fragility of bone and susceptibility to fracture (1). Osteoporotic fractures occur most commonly at the spine, hip, forearm and other sites, while hip fracture is associated with high mortality and morbidity (2,3). Studies have indicated an increasing incidence of hip fracture in Chinese cities (4,5), and this is a significant burden for society. Accurate and reliable knowledge of the prevalence of osteoporosis and osteoporotic fracture throughout China will be critical for policy-making and healthcare planning. A cross-sectional and population-based study conducted in Shanghai in 2010 showed that the prevalence of osteoporotic fractures was 14.9% in females (57.6±9.5 years) and 12.2% in males (58.5±10.1 years) (6). Results of Mister Osteoporosis Study and Miss Osteoporosis Study from 2001 to 2003 suggested that the prevalence of vertebral fractures (defined as grade ≥2 vertebral deformity according to Genant’s criteria) in Hong Kong was 5.0% among elderly men (mean age: 72.4 years old) and 12.1% among elderly women (mean age: 72.6 years old) (7).
In the past, dual energy X-ray absorptiometry (DXA) has been widely used to study the epidemiology of osteoporosis, and in the diagnosis and management of osteoporosis. It was demonstrated using DXA that the bone mineral density (BMD) of 85-year-old women reflected a loss of 32% at the spine and 30–35% at the femur measurement sites in China (8). The two-dimensional projection nature of DXA images makes the measurement susceptible to degenerative changes in the spine and aortic calcification. Our previous study verified that a substantial number of patients with osteoporosis were missed by DXA measurements (9). Quantitative computed tomography (QCT) is technically superior to DXA for measuring BMD in the spine and hip, and has attracted increasing attention in recent years (10-17). The diagnosis of osteoporosis by DXA relies on T score measurements at the spine and hip, and the calculation of T scores relies on the use of reference databases provided by the manufacturers. Therefore, the variations in the prevalence of osteoporosis reported in different studies may be partially due to the differences in the reference databases, and not indicative of true differences in the prevalence of osteoporosis. A diagnostic criterion of osteoporosis by QCT of a spinal trabecular volumetric BMD (vBMD) less than 80 mg/cm3 was recommended by the International Society for Clinical Densitometry in 2007 (17) and American College of Radiology in 2008 (18). Because the lateral scout view image of the CT scan can be used to assess for prevalent vertebral fractures (19-21), and vBMD measurements can be achieved simultaneously, QCT can provide accurate data on the prevalence of osteoporosis. However, the prevalence of osteoporosis and vertebral fractures using QCT data has not yet been studied in a Chinese population.
The Prospective Urban Rural Epidemiology (PURE) study is an international, large, multi-center, community-based, epidemiological cohort study in 18 countries, including China. The details of this study and the baseline characteristics have been reported (22,23). The details of Chinese participants and their baseline characteristics were reported recently by Peng et al. (24). The PURE China Action on Spine and Hip status (CASH) study focused on the prevalence of osteoporosis and osteoporotic spinal fractures in China. The participants in the PURE CASH study are all from the PURE study in China. The objectives of this study are: (I) to determine the prevalence of osteoporosis in this population by QCT vBMD measurement; (II) to determine the prevalence of osteoporotic vertebral fractures and their association with vBMD; (III) to determine the power of vBMD to predict future fractures in a follow-up study.
Study design
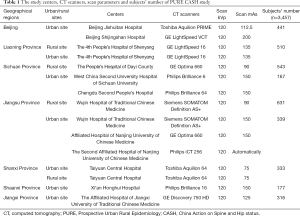
The PURE CASH study (identifier: NCT01758770) is a prospective, multicenter, epidemiological study. The subjects of PURE CASH study are enrolled from 12 centers (Beijing Jishuitan Hospital, Beijing Shijingshan Hospital, Taiyuan Central Hospital, West China Second University Hospital of Sichuan University, Chengdu Second People’s Hospital, the People’s Hospital of Dayi County, the 4th People’s Hospital of Shenyang, Wujin Hospital of Traditional Chinese Medicine, Affiliated Hospital of Nanjing University of Chinese Medicine, the Second Affiliated Hospital of Nanjing University of Chinese Medicine, Xi’an Honghui Hospital, the Affiliated Hospital of Jiangxi University of Traditional Chinese Medicine). From June 2013 to March 2017, all the subjects underwent QCT scans of the lumbar spine with thoracic and lumbar spine CT scout views. The participants of PURE CASH study will be followed up for incident fractures as required by the protocol of PURE study in the future.
Ethical approval is obtained from the ethics committee of the Beijing Jishuitan Hospital, Peking University (Approval No. 201210-01 and No. 201512-02). The study is conducted in accordance with ethical principles according to the Declaration of Helsinki and is consistent with Good Clinical Practice. Radiation safety and protection measures are strictly implemented in the whole study. Informed consent is obtained from every participant in the study.
The participants are from 12 centers in 7 Chinese provinces including Beijing, Liaoning, Shanxi, Shaanxi, Sichuan, Jiangsu and Jiangxi. The inclusion criteria are that participants should be aged over 40 years old and able to give informed consent. Exclusion criteria are pregnant women, individuals with metal implants in the lumbar spine, use of medications or the existence of any disease or condition known to have a major influence on BMD, and inability to give informed consent.
The estimation of sample size and the recruitment
When enrollment commenced the estimated number of participants is more than 3,000. Since there is no population based QCT prevalence data available in China, we use the published DXA data for osteoporosis prevalence in China instead. The prevalence of osteoporosis by DXA BMD measurements is between 5% and 20% according to areal measurements (25). Under a two-sided 0.05 alpha level, 500 participants per center is sufficient to ensure a ±3.5% estimated precision on the osteoporosis rate for each area (the width of the 95% confidence interval will be less than 7.0%). Since QCT is more sensitive than DXA for detecting osteoporosis (9), the detected prevalence of osteoporosis is expected to be higher. Hence the current sample size is sufficient to ensure adequate accuracy.
The assumed prevalence of osteoporotic vertebral fractures is between 15% and 25% (25,26). Given the sample size per province and the adopted significant level, the precision of the estimate of prevalent osteoporotic vertebral fractures will be less than ±3.8% (means that the maximum width of 95% CI will not exceed 7.6%).
Recruitment was started in June 2013, and details are shown in Table 1. Up to now, a total of 3,457 subjects have been enrolled in the 12 centers. Each subject completed a one-page questionnaire regarding factors that may have an effect on bone (Supplementary file). Full informed consent is obtained before an appointment being made for a QCT scan at the nearest participating imaging center.
Full table
The QCT scan
An abdominal CT scan is performed with a Mindways QCT calibration phantom beneath the spine. The scan parameters are predefined at each installation, and are different at different centers according to the CT scanners (Table 1). Radiation protection measures are implemented according to local requirements. A lateral scout view of T4 to L4 vertebrae is obtained for localization.
Quality control and cross calibration of QCT scan
All QCT scans are performed using the CT scanner available at each center (Table 1). The Mindways QCT (QCT Pro, Mindways software Inc., Austin, TX, USA) system is used in each center. Four sets of Mindways QCT Pro systems are rotated between centers. The Mindways QCT system is shipped to the center and installed. The staff are trained by research associates from Beijing Jishuitan Hospital. For cross-calibration, a single European Spine Phantom (ESP-145) is scanned at all centers before scanning the subjects. All QCT data are transferred to Beijing Jishuitan Hospital for analysis and quality control.
The BMD measurement of vertebral body
The vBMD values (mg/cm3) of the L1, L2 and L3 vertebral body are measured according to the Mindways protocol. The average vBMD value of L1–L3 is calculated as the spinal vBMD outcome of each subject.
The diagnosis of osteoporosis
The diagnostic criteria of osteoporosis for QCT, recommended by the International Society for Clinical Densitometry in 2007 (17) and American College of Radiology in 2008 (18), is used to classify the subjects as normal if average vBMD >120 mg/cm3, osteopenia if vBMD between 120 and 80 mg/cm3, and osteoporosis if vBMD <80 mg/cm3.
The vertebral fracture assessment (VFA)
The lateral scout view images from the QCT scans are used to detect vertebral body fractures according to Genant’s semiquantitative method (27,28). Each vertebral body is classified as normal (grade 0), mild (grade 1, approximately 20–25% depression in height and a reduction in area 10–20%), moderate (grade 2, approximately 25–40% depression in height and a reduction in area 20–40%), or severe (grade 3, more than 40% reduction in height and area) fracture (27,28). The digital images are displayed and viewed on a professional work station with the RadiAnt DICOM Viewer software (Version 4.5.9, Medixant Company, Poland); the quantitative diagnosis is performed by two musculoskeletal radiologists with many years’ experience of vertebral fracture assessment. The outcomes are determined via consensus opinion. A subject is considered to have a spinal osteoporotic fracture if any one of the T4–L4 vertebral bodies had a VFA score ≥ grade 1. The highest VFA score for each subject will be considered the severity.
The benefit for the study participants
The vBMD results along with any abnormal CT scan findings will be provided to the participants.
Conclusions
This study is the first to determine the prevalence of osteoporosis and vertebral fractures in China by QCT measurements in a large-scale, multicenter population. Accurate data on the prevalence of osteoporosis and osteoporotic fracture in China can be obtained, and their association can be assessed. These data may have great significance for future policy-making and the prevention of osteoporosis and osteoporotic fractures in China.
Questionnaire of PURE CASH Study
PURE Identifier: ____________________
Name: ________ Gender: _______ Date of Birth: _______ (mm)/ _______ (dd)/ _______ (yy)
Age: ________ years old Nation: ________
Weight: ________ kg Height: ________ cm
Waist Circumference: ________ cm Hip Circumference: ________ cm
Blood Pressure: ________ (SBP)/ ________ (DBP) mmHg
Fasting blood-glucose: ________ mmol/L
Age of menopause (if postmenopausal females): ________ years old
Fracture History: None ______
Yes ________ Date of Fracture if any _______ Fracture Site if any ________
Hip Fracture History of parents: None ________ Yes ________
Tobacco Use: No ______ Yes ______ How many cigarettes per day if any ________
Glucocorticoids use: No ________ Yes ________
History of Rheumatic Arthritis: No ________ Yes ________
History of Secondary Osteoporosis: No ________ Yes ________
[NOTE: Secondary osteoporosis referred to the osteoporosis caused by Type I diabetes mellitus (insulin-dependent diabetes mellitus), adult osteogenesis imperfecta (idiopathic osteopsathyrosis), hyperparathyroidism, hypogonadism or premature menopause (age <45 years old), chronic malnutrition or malabsorption, and chronic hepatopathy.]
Alcohol Use Amount equal to or more than 3 Units per day: No ________ Yes ________
[NOTE: One unit means 285 mL beer, 30 mL spirit, 120 mL wine, 60 mL fruit wine, or 60 mL sake.]
Date: _______ (mm)/ _______ (dd)/ _______ (yy)
Signature: _________
Acknowledgements
Funding: The study was supported by the National Natural Science Found of China (No. 81771831), Beijing Bureau of Health 215 Program (No. 2009-2-03) and Capital Health Development Research Program (No. 2014-2-1122).
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: Ethical approval was obtained from the ethics committee of the Beijing Jishuitan Hospital, Peking University (Approval No. 201210-01 and No. 201512-02) and informed consent was obtained from every participant in the study.
References
- Kanis JA, Melton LJ 3rd, Christiansen C, Johnston CC, Khaltaev N. The diagnosis of osteoporosis. J Bone Miner Res 1994;9:1137-41. [Crossref] [PubMed]
- Johnell O, Kanis JA. An estimate of the worldwide prevalence and disability associated with osteoporotic fractures. Osteoporos Int 2006;17:1726-33. [Crossref] [PubMed]
- Kanis JA, Odén A, McCloskey EV, Johansson H, Wahl DA, Cooper C. IOF Working Group on Epidemiology and Quality of Life. A systematic review of hip fracture incidence and probability of fracture worldwide. Osteoporos Int 2012;23:2239-56. [Crossref] [PubMed]
- Xia WB, He SL, Xu L, Liu AM, Jiang Y, Li M, Wang O, Xing XP, Sun Y, Cummings SR. Rapidly increasing rates of hip fracture in Beijing, China. J Bone Miner Res 2012;27:125-9. [Crossref] [PubMed]
- Wang J, Wang Y, Liu WD, Wang F, Yin ZS. Hip fractures in Hefei, China: the Hefei osteoporosis project. J Bone Miner Metab 2014;32:206-14. [Crossref] [PubMed]
- Liu JM, Ma LY, Bi YF, Xu Y, Huang Y, Xu M, Zhao HY, Sun LH, Tao B, Li XY, Wang WQ, Ning G. A population-based study examining calcaneus quantitative ultrasound and its optimal cut-points to discriminate osteoporotic fractures among 9352 Chinese women and men. J Clin Endocrinol Metab 2012;97:800-9. [Crossref] [PubMed]
- Kwok AW, Gong JS, Wang YX, Leung JC, Kwok T, Griffith JF, Leung PC. Prevalence and risk factors of radiographic vertebral fractures in elderly Chinese men and women: results of Mr. OS (Hong Kong) and Ms. OS (Hong Kong) studies. Osteoporos Int 2013;24:877-85. [Crossref] [PubMed]
- Cheng XG, Yang DZ, Zhou Q, Zhuo TJ, Zhang HC, Xiang J, Wang HF, Ou PZ, Liu JL, Xu L, Huang GY, Huang QR, Barden HS, Weynand LS, Faulkner KG, Meng XW. Age-related bone mineral density, bone loss rate, prevalence of osteoporosis, and reference database of women at multiple centers in China. J Clin Densitom 2007;10:276-84. [Crossref] [PubMed]
- Li N, Li XM, Xu L, Sun WJ, Cheng XG, Tian W. Comparison of QCT and DXA: Osteoporosis Detection Rates in Postmenopausal Women. Int J Endocrinol 2013;2013. [Crossref] [PubMed]
- Link TM, Lang TF. Axial QCT: clinical applications and new developments. J Clin Densitom 2014;17:438-48. [Crossref] [PubMed]
- Engelke K, Fuerst T, Dardzinski B, Kornak J, Ather S, Genant HK, de Papp A. Odanacatib treatment affects trabecular and cortical bone in the femur of postmenopausal women: results of a two-year placebo-controlled trial. J Bone Miner Res 2015;30:30-8. [Crossref] [PubMed]
- Tsai JN, Uihlein AV, Burnett-Bowie SA, Neer RM, Zhu Y, Derrico N, Lee H, Bouxsein ML, Leder BZ. Comparative effects of teriparatide, denosumab, and combination therapy on peripheral compartmental bone density, microarchitecture, and estimated strength: the DATA-HRpQCT Study. J Bone Miner Res 2015;30:39-45. [Crossref] [PubMed]
- Poole KE, Treece GM, Gee AH, Brown JP, McClung MR, Wang A, Libanati C. Denosumab rapidly increases cortical bone in key locations of the femur: a 3D bone mapping study in women with osteoporosis. J Bone Miner Res 2015;30:46-54. [Crossref] [PubMed]
- Engelke K, Lang T, Khosla S, Qin L, Zysset P, Leslie WD, Shepherd JA, Schousboe JT. Clinical Use of Quantitative Computed Tomography (QCT) of the Hip in the Management of Osteoporosis in Adults: the 2015 ISCD Official Positions-Part I. J Clin Densitom 2015;18:338-58. [Crossref] [PubMed]
- Zysset P, Qin L, Lang T, Khosla S, Leslie WD, Shepherd JA, Schousboe JT, Engelke K. Clinical Use of Quantitative Computed Tomography-Based Finite Element Analysis of the Hip and Spine in the Management of Osteoporosis in Adults: the 2015 ISCD Official Positions-Part II. J Clin Densitom 2015;18:359-92. [Crossref] [PubMed]
- Engelke K, Lang T, Khosla S, Qin L, Zysset P, Leslie WD, Shepherd JA, Shousboe JT. Clinical Use of Quantitative Computed Tomography-Based Advanced Techniques in the Management of Osteoporosis in Adults: the 2015 ISCD Official Positions-Part III. J Clin Densitom 2015;18:393-407. [Crossref] [PubMed]
- Engelke K, Adams JE, Armbrecht G, Augat P, Bogado CE, Bouxsein ML, Felsenberg D, Ito M, Prevrhal S, Hans DB, Lewiecki EM. Clinical use of quantitative computed tomography and peripheral quantitative computed tomography in the management of osteoporosis in adults: the 2007 ISCD Official Positions. J Clin Densitom 2008;11:123-62. [Crossref] [PubMed]
- American College of Radiology. ACR Practice Guideline for the Performance of Quantitative Computed Tomography (QCT) Bone Densitometry (Resolution 33), Reston, Va, USA, 2008. Available online: https://www.acr.org/-/media/ACR/Files/Practice-Parameters/QCT.pdf
- Kim YM, Demissie S, Genant HK, Cheng X, Yu W, Samelson EJ, Kiel DP, Bouxsein ML. Identification of prevalent vertebral fractures using CT lateral scout views: a comparison of semi-automated quantitative vertebral morphometry and radiologist semi-quantitative grading. Osteoporos Int 2012;23:1007-16. [Crossref] [PubMed]
- Samelson EJ, Christiansen BA, Demissie S, Broe KE, Zhou Y, Meng CA, Yu W, Cheng X, O'Donnell CJ, Hoffmann U, Genant HK, Kiel DP, Bouxsein ML. Reliability of vertebral fracture assessment using multidetector CT lateral scout views: the Framingham Osteoporosis Study. Osteoporos Int 2011;22:1123-31. [Crossref] [PubMed]
- Kim YM, Demissie S, Eisenberg R, Samelson EJ, Kiel DP, Bouxsein ML. Intra-and inter-reader reliability of semi-automated quantitative morphometry measurements and vertebral fracture assessment using lateral scout views from computed tomography. Osteoporos Int 2011;22:2677-88. [Crossref] [PubMed]
- Teo K, Chow CK, Vaz M, Rangarajan S, Yusuf S. PURE Investigators-Writing Group. The Prospective Urban Rural Epidemiology (PURE) study: examining the impact of societal influences on chronic noncommunicable diseases in low-, middle-, and high-income countries. Am Heart J 2009;158:1-7.e1. [Crossref] [PubMed]
- Corsi DJ, Subramanian SV, Chow CK, McKee M, Chifamba J, Dagenais G, Diaz R, Iqbal R, Kelishadi R, Kruger A, Lanas F, López-Jaramilo P, Mony P, Mohan V, Avezum A, Oguz A, Rahman MO, Rosengren A, Szuba A, Li W, Yusoff K, Yusufali A, Rangarajan S, Teo K, Yusuf S. Prospective Urban Rural Epidemiology (PURE) study: Baseline characteristics of the household sample and comparative analyses with national data in 17 countries. Am Heart J 2013;166:636-46.e4. [Crossref] [PubMed]
- Peng Y, Li W, Wang Y, Bo J, Chen H. The Cut-Off Point and Boundary Values of Waist-to-Height Ratio as an Indicator for Cardiovascular Risk Factors in Chinese Adults from the PURE Study. PLoS One 2015;10. [Crossref] [PubMed]
- Ling X, Cummings SR, Mingwei Q, Xihe Z, Xioashu C, Nevitt M, Stone K. Vertebral fractures in Beijing, China: the Beijing Osteoporosis Project. J Bone Miner Res 2000;15:2019-25. [Crossref] [PubMed]
- Lin X, Xiong D, Peng YQ, Sheng ZF, Wu XY, Wu XP, Wu F, Yuan LQ, Liao EY. Epidemiology and management of osteoporosis in the People's Republic of China: current perspectives. Clin Interv Aging 2015;10:1017-33. [PubMed]
- Genant HK, Wu CY, van Kuijk C, Nevitt MC. Vertebral fracture assessment using a semiquantitative technique. J Bone Miner Res 1993;8:1137-48. [Crossref] [PubMed]
- Wu CY, Li J, Jergas M, Genant HK. Comparison of semiquantitative and quantitative techniques for the assessment of prevalent and incident vertebral fractures. Osteoporos Int 1995;5:354-70. [Crossref] [PubMed]


