Time to tracheal intubation over a fibreoptic bronchoscope using a silicone left double-lumen endobronchial tube versus polyvinyl chloride single-lumen tube with bronchial blocker: a randomized controlled non-inferiority trial
Introduction
Many intrathoracic procedures demand optimal collapse of the operative lung to facilitate surgical exposure (1). Single-lung ventilation can be achieved using a double-lumen tube (DLT), a Univent tube, or an independent bronchial blocker. Among these, DLTs are advantageous for several reasons, including quick placement, rapid and clear deflation, suctioning from the isolated lung, and application of continuous positive airway pressure when necessary (2-10). Insertion of a DLT using a direct laryngoscope can be more difficult than that of single-lumen tube (SLT), especially in patients for whom airway difficulty is anticipated (11). Several techniques have been suggested to address this issue, including direct placement of the DLT over a fibreoptic bronchoscope (FOB), use of a lighted stylet, use of a fibreoptic laryngoscope (WuScope), and the retrograde wire technique (12-14). The safest of the proposed methods involves the placement of an SLT with the aid of an FOB, following which the SLT is replaced with a DLT using an airway exchange technique (12,15), because it is believed that direct placement of the DLT over the FOB is more traumatic and difficult than that of the SLT (9,11,12,15-19). Only two case reports have discussed the direct placement of a polyvinylchloride (PVC) DLT over an FOB (20,21). The expected difficulty is mainly associated with railroading (advancement over the FOB) the DLT into the trachea because DLTs are larger and less compliant (19,21).
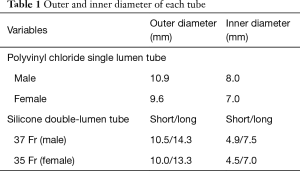
One recent simulation study demonstrated that a soft silicone DLT with a flexible, wire-reinforced bronchial tip (Fuji-Phycon tube) may shorten the time to intubation via tube exchange when compared with less compliant, PVC DLTs such as the Mallinckrodt or Rusch DLT (22). HumanBroncho® (Insung Medical, Seoul, Korea) is a new silicone DLT with a soft, flexible, non-bevelled, wire-reinforced tip. The oval shape, obtuse angle, and short lateral internal diameter of the bronchial lumen and its flexibility (Table 1, Figure 1) may allow for advancement to the trachea over the FOB with as much as ease as a PVC SLT.
Full table
In the present study, we aimed to test the hypothesis that the silicone DLT would be non-inferior to a PVC SLT with regard to intubation time over an FOB. We further aimed to compare the ease of railroading the tracheal tube over the FOB between the silicone DLT and PVC SLT.
Methods
The present study was a single-centre, prospective, open-label, randomized controlled, non-inferiority trial involving two parallel groups. We recruited patients from Ajou University Hospital in Suwon, South Korea, from May 2017 to Aug 2017. Patients with American Society of Anaesthesiologists (ASA) physical status class I or II, aged 20–75 years, and scheduled for thoracic surgery requiring single-lung ventilation were eligible for inclusion. Patients with histories of cardiopulmonary, gastrointestinal, or upper airway disease; increased risk of pulmonary aspiration; or body mass index >30 kg/m2 were excluded. Written informed consent was obtained from each patient on the day prior to surgery. The patients were randomly assigned to one of two groups (SLT group and DLT group) in a 1:1 allocation ratio using a computer-generated random number table. The allocation process was conducted by a colleague who remained independent of this research project. The randomization result was concealed within serially numbered opaque envelopes, which were opened in the operating room prior to induction of anaesthesia.
The operation was performed with the patient’s head resting on a large, donut-shaped pillow, and all patients received standardized general anaesthesia until the end of the research protocol. All patients underwent electrocardiography, non-invasive monitoring of blood pressure, pulse oximetry, capnography, and measurement of volatile anaesthetic levels. The depth of anaesthesia was monitored using a bispectral index monitor [BIS VISTATM Monitor (four-electrode sensor), Aspect Medical Systems, Norwood, MA, USA]. Following preoxygenation with a tight-fitting mask for 3 min, anaesthesia was induced using fentanyl (2 µg/kg) and thiopental sodium (4 mg/kg). Neuromuscular blockade was established using rocuronium (0.6 mg/kg). The patient’s lungs were ventilated with sevoflurane (end-tidal concentration: 2–3%) in oxygen. Two min after rocuronium injection, mouth opening (inter-incisor distance), thyromental distance, and modified Cormack-Lehane grade were measured via direct laryngoscopy.
In both groups, a flexible FOB (PortaView® LF-GP; Olympus Optical Company, Tokyo, Japan) with a diameter of 4.1 mm was used for tracheal intubation, and jaw thrust was applied to all patients to clear the airway without the aid of an intubating airway. The tip of the FOB was positioned above the carina, following which the preloaded SLT or DLT was railroaded over the FOB. If advancement of the tracheal tube was impeded during the attempt, the tracheal tube was withdrawn 2–3 cm over the FOB, rotated 90° counter-clockwise, and re-advanced towards the trachea. If further resistance was encountered, the degree of counter-clockwise rotation was increased until successful intubation was achieved.
Time to insertion of the FOB was defined as the time from the passage of the FOB beyond the teeth to FOB positioning above the carina. Railroading time was defined as the time from FOB positioning above the carina to confirmation of tracheal tube positioning in the trachea above the carina, not to the correct positioning of the DLT or SLT. Time to tracheal tube intubation was defined as the time to insertion plus the railroading time. Total time required for correct positioning of the DLT or bronchial blocker was defined as the time from the passage of the FOB beyond the teeth to confirmation of correct positioning of the bronchial blocker or DLT into the desired mainstem bronchus via the FOB. The difficulty of railroading the tube was graded along a four-point scale (1, no difficulty passing the tube; 2, obstruction while passing the tube, relieved by withdrawal and a 90° counter-clockwise rotation; 3, obstruction necessitating more than one manipulation or external laryngeal manipulation; 4, direct laryngoscopy was required) (23). After correct positioning had been achieved, anaesthesia was maintained using sevoflurane (end-tidal concentration: 1.5–2.5%) in 50% oxygen in an oxygen-air mixture.
In the SLT group, a standard bevelled Portex® endotracheal tube (Smiths Medical, Hythe, UK; male patients: 8.0 mm internal diameter, female patients: 7.0 mm internal diameter, Table 1) was used, and the bevel of the tube was oriented to the patient’s left. Once the SLT was positioned 2–3 cm above the carina, a smaller FOB (PortaView® LF-DP; Olympus Optical Company, Tokyo, Japan; outer diameter 3.1 mm) was passed through the SLT to allow for visualization of the carina, and the bronchial blocker (Coopdech Endobronchial Blocker tube; Daiken, Osaka, Japan) was passed into the appropriate mainstem bronchus, following which the FOB was removed. In the DLT group, the insertion of bronchial lumen through the vocal cord was initially performed with the concave curvature facing left. Once the left-sided silicone DLT (Figure 1) appeared above the carina in the eyepiece of the FOB, the FOB was used to confirm entry of the bronchial lumen into the left main bronchus. The FOB was then withdrawn and re-inserted into the tracheal lumen for correct positioning of the DLT.
All fibreoptic intubations and bronchial blocker insertions were performed by a single anaesthetist (DH Kim) who was familiar with and had been trained in bronchial blocker insertion and intubation using an FOB. Times were recorded by another anaesthetist (YJ Chae) using a video camera.
The primary outcome measure of the present study was the difference in the time to intubation between the groups, designed as a non-inferiority test. The acceptable margin for non-inferiority was pre-set at 10 s. The sample size for this non-inferiority margin was calculated based on an assumed standard deviation (SD) of 18 s, based on the findings of previous study (24). This calculation revealed that a total of 40 patients per group would be necessary to achieve a power of 80% at a significance level of 5%. Other secondary endpoints included the following: time to insertion of the FOB, railroading time, total time for correct tube and bronchial blocker positioning, grade of railroading difficulty over the FOB, and degree of hoarseness, sore throat, and swallowing difficulty in the post-anaesthesia care unit (PACU). All secondary endpoints were analysed for superiority.
Statistical analysis was performed using SPSS version 21 (SPSS Inc., Chicago, IL, USA). Continuous data were tested for normality of distribution using the Kolmogorov-Smirnov test. The primary outcome was assessed based on the median difference and 95% confidence interval using the Hodges-Lehmann method. Non-inferiority would have been declared if the upper bound of the two-sided 95% confidence interval for the true difference in the time to endotracheal tube intubation between groups (DLT intubation time minus SLT intubation time) was below the non-inferiority margin of 10 s. Normally distributed data were presented as means with SDs and examined using Student’s t-test; non-normally distributed data were compared between the groups using Mann-Whitney U-tests and presented as medians with interquartile ranges. Categorical data were presented as numbers and percentages. Chi-square or Fisher’s exact tests were used to compare categorical variables between the groups. The level of statistical significance was set at P<0.05.
Results
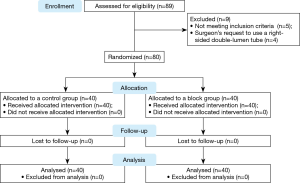
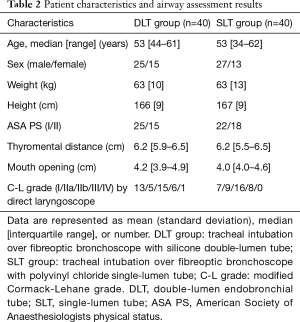
A total of 89 patients were assessed for eligibility. Five patients were excluded for meeting exclusion criteria, while four patients were excluded because of the surgeon’s request to use a right-sided DLT. Thus, a total of 80 patients were randomized into two groups. The participant flow diagram is presented in Figure 2. These 80 patients underwent fibreoptic tracheal intubation, the first attempt at which was successful in all patients. There were no missing data. Patient characteristics and airway assessment data are presented in Table 2. There were no significant differences in patient characteristics between the groups.
Full table
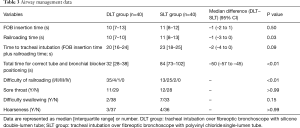
The median intubation time over the FOB was 20 s in the DLT group and 23 s in the SLT group. The median difference and 95% confidence interval were –2 s and –4 to 0 s, respectively. The upper confidence boundary was below the prospectively determined non-inferiority margin of 10 s (Table 3). The time to insertion of the FOB into the trachea was comparable between the groups; however, the railroading time was significantly shorter in the DLT group than in the SLT group (median time: 10 vs. 11 s; median difference: –1 s; 95% confidence interval: –3 to 0 s, respectively; P=0.03). Railroading over the FOB (rated on a four-point scale) was regarded as less difficult in the DLT group than in the SLT group (P<0.01). There was a significant difference in the total time for correct tube and bronchial blocker positioning (median time: 33 vs. 84 s; median difference: –50 s; 95% confidence interval: –57 to –45 s, respectively; P<0.01). There were no differences in the incidence of hoarseness, sore throat, or difficulty swallowing in the PACU between the two groups.
Full table
Discussion
The results of the present study demonstrate that the silicone DLT was non-inferior to the PVC SLT with regard to tracheal intubation time over the FOB. In addition, the railroading time over the FOB was shorter—and railroading was rated as less difficult—in the DLT group than in the SLT group.
FOB-guided tracheal intubation is safe and effective in patients with both anticipated and unanticipated difficult airways (19,25-27). However, direct insertion of the DLT over the FOB is expected to be more difficult and traumatic than that of the SLT because the DLT is longer, larger, and less compliant (9,11,12,15-19). Therefore, many anaesthesiologists first insert an SLT into the trachea in order to secure the airway, following which the DLT is placed using a tube exchanger in patients with airway difficulties (12,15). During FOB-guided tracheal intubation, difficulties can be encountered in two main areas: placement of the FOB into the trachea and railroading of the tracheal tube over the FOB (19). The former difficulty is associated with the length of the DLT, while the latter is associated with its larger diameter and relative lack of compliance. Based on our experience in the present study, the length of the DLT did not compromise our ability to manipulate the FOB in the vicinity of the vocal cords. While advancing the FOB in an attempt to position it above the carina, the end portion of the bronchial lumen of the DLT entered into the oropharynx, which did not occur with the SLT.
Previous studies have also reported that the larger diameter and relative lack of compliance of the DLT may make the railroading process more complicated than when performed using a SLT (11,15-17). This difficulty is assumed to result mainly from the PVC material of which DLTs are commonly constructed (28). Softer tubes may represent an appropriate alternative to PVC DLTs (19,29). As expected, our results indicated that the silicone DLT is not only non-inferior to PVC SLT, but rather 3 s faster than the PVC SLT with regard to tracheal intubation time and securing the airway. Moreover, the silicone DLT exhibited superior performance with regard to railroading time and railroading difficulty over the FOB, relative to the PVC SLT. In addition, we observed no significant differences in intubation-related complications such as sore throat, difficulty swallowing, or hoarseness between the two groups. These findings suggest that, with the use of the silicon DLT, direct placement of the DLT over the FOB is feasible. Furthermore, there may be no need to first insert an PVC SLT into the trachea for securing the airway in patients with anticipated airway difficulties.
In the present study, we observed no impingement while railroading the tube over the FOB in 33% of patients in the SLT group and 88% of patients in the DLT group, likely for two reasons. First, the flexible, wire-reinforced bronchial tip allows the silicone DLT to more easily change its direction to follow the curve of the FOB (19,29,30). In previous studies in which an SLT was used, a flexible tube proved easier to advance over the FOB than a PVC tube (29,30). One simulation study demonstrated that a soft, silicone DLT with a flexible, wire-reinforced bronchial tip (Fuji-Phycon tube) resulted in a significantly shorter time to intubation via tube exchange than a PVC DLT such as the Mallinckrodt or Rusch DLT (22). Our results suggest that the flexibility of the tube tip is an important factor that affects railroading over the FOB, regardless of whether it is an SLT or DLT. Second, the non-bevelled, oval, obtuse tip has a bronchial lumen with a short lateral internal diameter, allowing for unobstructed passage of the tube over the FOB, in contrast to the PVC SLT. An orally inserted FOB tends to move posteriorly and rest against the posterior portion of the glottis opening (19,31). The bevelled, acute-angled tip of the SLT may be at risk to impinge on the right arytenoid cartilage, indicating that the obtuse tip of the silicone DLT may have decreased the difficulty of railroading (19,29,32). The tip of the silicone DLT is oval in shape, and the long internal diameter is equal to or shorter (7.5 mm in 37 Fr; 7.0 mm in 35 Fr)—and the short lateral internal diameter is far shorter (4.9 mm in 37 Fr; 4.5 mm in 35 Fr)—than the internal diameter of the PVC SLT. This may reduce the gap between the tube tip and the FOB, thereby decreasing impingement (19). When the tube becomes impinged, counter-clockwise rotation by 90° can reliably overcome the impingement by allowing the bevelled tracheal tube to come into close contact with the FOB (19,33,34). Consistent with this finding, successful advancement was achieved via counter-clockwise rotation by 90° in most patients of the SLT group in whom the first attempt at advancement had failed. Such rotation was also effective in the DLT group, despite the difference in the shape of the tip, indicating that the site of impingement may differ. In patients in whom railroading the tracheal tube had failed following counter-clockwise rotation of 90°, the tracheal tube was rotated counter-clockwise at an angle greater than 90° (railroading difficulty: grade 3). We adopted this manoeuvre from a previous study, which reported that, when the tip of the tracheal tube was rotated counter-clockwise by 90°, impingement was overcome regardless of the impingement site (31). However, to achieve the desired 90° counter-clockwise rotation of the tip, it may be necessary to further increase the degree of rotation at the proximal end of the tracheal tube, since proximal rotation does not always result in proportional rotation at the distal tip of the tube (35). In the present study, further counter-clockwise rotation resolved the impingement in the remaining patients (two patients of the SLT group and one patient of the DLT group) without head manipulation or external laryngeal manipulation.
The time required to place the bronchial lumen of the DLT or a bronchial blocker in the correct position was greater in patients of the SLT group in whom a bronchial blocker was used, consistent with the findings of previous reports (7,36,37). In the SLT group, the time to insertion of the bronchial blocker and confirmation using the FOB seemed to be a time-consuming process: The median time required for this process was 32 s in the DLT group—considerably shorter than the range of 85 to 128 s reported in previous studies (7,36,37), even when individual differences in experience were taken into consideration. This drastic difference may be attributable to the nearly continuous process that began with direct insertion of the silicone DLT over the FOB and ended with final confirmation of tube placement. Tracheal intubation and guidance/placement of the left bronchial tube into the left main bronchus was performed with the aid of an FOB placed in the bronchial lumen. Then, the final position of the DLT was confirmed using the FOB after it had been withdrawn and re-inserted into the tracheal lumen. This process was simple to implement and occurred without interruption. In two patients of the present study, the bronchial lumen was advanced into the right mainstem bronchus under direct observation through the FOB. The DLT was withdrawn, and the FOB was advanced into the left mainstem bronchus for use as a stylet, following which the bronchial lumen was guided into the left mainstem bronchus
The present study had several limitations. First, the anaesthetist performing FOB insertion was not blinded to the tracheal tube used; consequently, the potential for bias exists. Second, the FOB procedure was performed by a single experienced anaesthetist only. Therefore, this finding may not be generalizable to less experienced anaesthetists. Third, the present study was performed in patients with normal airway status, and our findings may not be directly applicable to difficult airway situations. Fourth, tracheal intubation over an FOB requires an additional operator to assist with the jaw thrust.
Conclusions
The findings of the present study indicate that tracheal intubation using an FOB can be achieved at least as fast using the silicone DLT as using the PVC SLT. Furthermore, our results indicate that the silicone DLT exhibited superior performance with regard to railroading over the FOB when compared with the PVC SLT.
Acknowledgements
This work was supported by Insung Medical, Seoul, Korea (to DH Kim).
Footnote
Conflicts of Interest: This study was presented as a poster presentation at the 12th Asian Society of Cardiothoracic Anaesthesiologists, Scientific meeting at Hong Kong, in 2017.
Ethical Statement: The study was approved by the Institutional Review Board of Ajou University Hospital (Suwon, South Korea) (No. AJIRB-DEV-OBS-17-070) and was registered with ClinicalTrials.gov (NCT No: NCT03173443).
References
- Bernasconi F, Piccioni F. One-lung ventilation for thoracic surgery: current perspectives. Tumori 2017;103:495-503. [Crossref] [PubMed]
- Weiskopf RB, Campos JH. Current techniques for perioperative lung isolation in adults. Anesthesiology 2002;97:1295-301. [Crossref] [PubMed]
- El-Tahan MR. Videolaryngoscopes for placement of double lumen tubes: Is it time to say goodbye to direct view? Saudi J Anaesth 2016;10:218-27. [Crossref] [PubMed]
- Della Rocca G, Langiano N, Baroselli A, et al. Survey of thoracic anesthetic practice in Italy. J Cardiothorac Vasc Anesth 2013;27:1321-9. [Crossref] [PubMed]
- Eldawlatly A, Turkistani A, Shelley B, et al. Anesthesia for thoracic surgery: a survey of middle eastern practice. Saudi J Anaesth 2012;6:192-6. [Crossref] [PubMed]
- Shelley B, Macfie A, Kinsella J. Anesthesia for thoracic surgery: a survey of UK practice. J Cardiothorac Vasc Anesth 2011;25:1014-7. [Crossref] [PubMed]
- Narayanaswamy M, McRae K, Slinger P, et al. Choosing a lung isolation device for thoracic surgery: a randomized trial of three bronchial blockers versus double-lumen tubes. Anesth Analg 2009;108:1097-101. [Crossref] [PubMed]
- Yoo JY, Kim DH, Choi H, et al. Disconnection technique with a bronchial blocker for improving lung deflation: a comparison with a double-lumen tube and bronchial blocker without disconnection. J Cardiothorac Vasc Anesth 2014;28:904-7. [Crossref] [PubMed]
- Montague J, Krivskiy L. Difficult Intubation and Double Lumen Tubes, Time to Embrace Videolaryngoscopy. Austin J Anesthesia and Analgesia 2016;4:1047.
- Orlewicz MS. Double-Lumen Endotracheal Tube Placement. 2016. Accessed 9, Aug 2017. Available online: http://emedicine.medscape.com/article/1999993-overview
- Shulman GB, Connelly NR. Double lumen tube placement with the Bullard laryngoscope. Can J Anaesth 1999;46:232-4. [Crossref] [PubMed]
- Campos JH. Lung isolation techniques for patients with difficult airway. Curr Opin Anaesthesiol 2010;23:12-7. [Crossref] [PubMed]
- O'Connor CJ, O'Connor TA. Use of lighted stylets to facilitate insertion of double-lumen endobronchial tubes in patients with difficult airway anatomy. J Clin Anesth 2006;18:616-9. [Crossref] [PubMed]
- Alfery DD. Double-lumen endobronchial tube intubation using a retrograde wire technique. Anesth Analg 1993;76:1374-5. [Crossref] [PubMed]
- Perlin DI, Hannallah MS. Double-lumen tube placement in a patient with a difficult airway. J Cardiothorac Vasc Anesth 1996;10:787-8. [Crossref] [PubMed]
- Thota RS. Conversion of a single lumen tube to double lumen tube in an anticipated difficult airway: Flexible fiberoptic bronchoscope assisted with intubating introducer-guided technique. Ann Card Anaesth 2016;19:149-51. [Crossref] [PubMed]
- Benumof JL. Difficult tubes and difficult airways. J Cardiothorac Vasc Anesth 1998;12:131-2. [Crossref] [PubMed]
- Brodsky JB. Lung separation and the difficult airway. Br J Anaesth 2009;103 Suppl 1:i66-75. [Crossref] [PubMed]
- Asai T, Shingu K. Difficulty in advancing a tracheal tube over a fibreoptic bronchoscope: incidence, causes and solutions. Br J Anaesth 2004;92:870-81. [Crossref] [PubMed]
- Haitov Z, Evron S, Gofman V, et al. Awake fiberoptic double lumen tube insertion in five patients with anticipated difficult airways. Indian J Thorac Cardiovasc Surg 2011;27:125. [Crossref]
- Shulman MS, Brodsky JB, Levesque PR. Fibreoptic bronchoscopy for tracheal and endobronchial intubation with a double-lumen tube. Can J Anaesth 1987;34:172-3. [Crossref] [PubMed]
- Gamez R, Slinger P. A simulator study of tube exchange with three different designs of double-lumen tubes. Anesth Analg 2014;119:449-53. [Crossref] [PubMed]
- Makino H, Katoh T, Kobayashi S, et al. The effects of tracheal tube tip design and tube thickness on laryngeal pass ability during oral tube exchange with an introducer. Anesth Analg 2003;97:285-8. table of contents. [Crossref] [PubMed]
- Kim DH, Yoo JY, Ha SY, et al. Comparison of the paediatric blade of the Pentax-AWS and Ovassapian airway in fibreoptic tracheal intubation in patients with limited mouth opening and cervical spine immobilization by a semi-rigid neck collar: a randomized controlled trial. Br J Anaesth 2017;119:993-9. [Crossref] [PubMed]
- Collins SR, Blank RS. Fiberoptic intubation: an overview and update. Respir Care 2014;59:865-78; discussion 878-80. [Crossref] [PubMed]
- Rodrigues AJ, Scordamaglio PR, Palomino AM, et al. Difficult airway intubation with flexible bronchoscope. Braz J Anesthesiol 2013;63:358-61. [Crossref]
- Tawfeek MM, Abdelbaky AM. Is fiberoptic bronchoscope a good intubating choice in anesthetized patients with anticipated difficult intubation? Egyptian Journal of Anaesthesia 2011;27:157-61. [Crossref]
- Jeon J, Lee K, Ahn G, et al. Comparison of postoperative sore throat and hoarseness between two types of double-lumen endobronchial tubes: a randomized controlled trial. J Cardiothorac Vasc Anesth 2015;29:121-5. [Crossref] [PubMed]
- Brull SJ, Wiklund R, Ferris C, et al. Facilitation of fiberoptic orotracheal intubation with a flexible tracheal tube. Anesth Analg 1994;78:746-8. [Crossref] [PubMed]
- Calder I. When the endotracheal tube will not pass over the flexible fiberoptic bronchoscope. Anesthesiology 1992;77:398. [Crossref] [PubMed]
- Jackson AH, Orr B, Yeo C, et al. Multiple sites of impingement of a tracheal tube as it is advanced over a fibreoptic bronchoscope or tracheal tube introducer in anaesthetized, paralysed patients. Anaesth Intensive Care 2006;34:444-9. [Crossref] [PubMed]
- Johnson DM, From AM, Smith RB, et al. Endoscopic study of mechanisms of failure of endotracheal tube advancement into the trachea during awake fiberoptic orotracheal intubation. Anesthesiology 2005;102:910-4. [Crossref] [PubMed]
- Sharma D, Bithal P, Rath G, et al. Effect of orientation of a standard polyvinyl chloride tracheal tube on success rates during awake flexible fibreoptic intubation. Anaesthesia 2006;61:845-8. [Crossref] [PubMed]
- Shearer AJ, McGuire BE. Railroading tracheal tubes over a fibrescope. Anaesthesia 2006;61:1222-author reply 1222-3. [Crossref] [PubMed]
- Marfin AG, Iqbal R, Mihm F, et al. Determination of the site of tracheal tube impingement during nasotracheal fibreoptic intubation. Anaesthesia 2006;61:646-50. [Crossref] [PubMed]
- Ruetzler K, Grubhofer G, Schmid W, et al. Randomized clinical trial comparing double-lumen tube and EZ-Blocker for single-lung ventilation. Br J Anaesth 2011;106:896-902. [Crossref] [PubMed]
- Campos JH, Kernstine KH. A comparison of a left-sided Broncho-Cath with the torque control blocker univent and the wire-guided blocker. Anesth Analg 2003;96:283-9. table of contents. [Crossref] [PubMed]