C5 palsy after insertion of a winged expandable cervical cage: a case report and literature review
Introduction
Multiple definitions of C5 nerve root palsy (C5P) have been reported basing on the grade of weakness and biceps involvement. One reports it as the loss of motor strength in the deltoid and/or biceps brachii associated to sensory deficit or increased pain in the C5 distribution (1). After cervical spine decompression, it is a well-known complication with a variable incidence ranging from 1.4% to 18.4% (2). Its onset has been reported in both posterior and anterior approaches. The use of a winged expandable titanium cage (WETC) after single or multiple corpectomy is among the used techniques in reconstructing the cervical spine. Herein we report a case of C5P after a three-level corpectomy and reconstruction using this device for the treatment of cervical spondylosis.
Case presentation
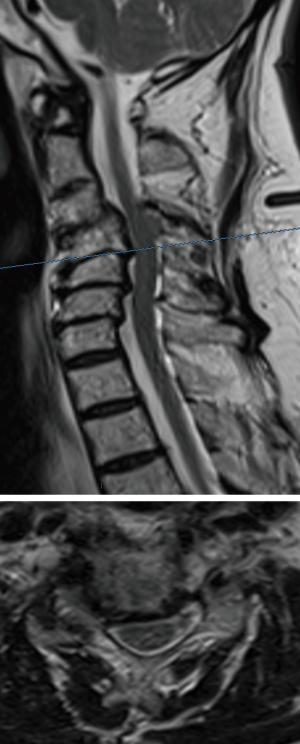
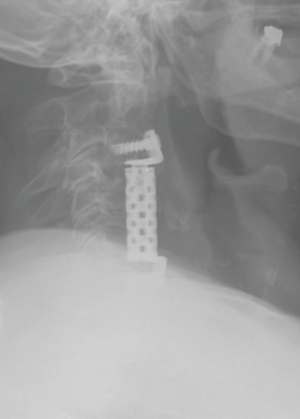
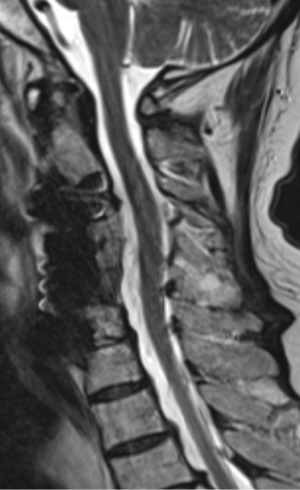
We report the case of a 66-year-old man with a two years history of left cervico-brachialgia and spastic ataxia. He referred to our clinic after a fall determined neurological worsening. Neurological exam showed power 4/5 in the left biceps and triceps, 4/5 in the left quadriceps, hyperactive lower limbs tendon reflexes and bilateral Babinski. Cervical radiograph demonstrated a severe spondylosis and loss of lordosis (Figure 1). Degenerative changes and spondylolisthesis at C4-C5-C6 with spinal cord compression were reported at MRI. C4-C5 was the most compressed level where a right foraminal stenosis was present (Figure 2). In order to decompress the spinal cord and improve patient’s symptoms, a three-level C4-C5-C6 corpectomy followed by the insertion of WETC was executed. In postsurgical hours and on first postsurgical day the patient showed good recovery from the weakness and the post-operative cervical radiograph demonstrated correct position of the device (Figure 3). Unfortunately, on second postsurgical day a right C5P was present. Urgent cervical MRI was executed, the exam demonstrated good spinal cord decompression excluding a postoperative hematoma or spinal cord injury (Figure 4). Dexamethasone 8 mg e.v. two times a day was started, but the patient did not recover from the palsy in post-surgical days and physiotherapy was continued in a rehabilitation centre. He was followed-up in our clinic and showed a full recovery at 2 months from the operation.
Discussion
Multiple definitions of C5P have been reported in literature basing on the different grade of weakness in the deltoid and biceps muscle and this may have contributed to its variable incidence. Nevertheless, C5P is a well-known complication after anterior or posterior decompression. Herein we report a case of C5P after a triple corpectomy for the treatment of cervical spondylosis using a WETC in reconstructing the spine.
In posterior decompression, the most described theory is the spinal cord shift due to wider posterior space after surgery determining C5 nerve root traction. A direct correlation between wider posterior decompression and C5P has been reported (3) and some authors propose a limited decompression in order to reduce the spinal cord shift. Nevertheless, Klement et al. (4) evaluated the width of laminectomy at CT imaging reporting no correlation between width of laminectomy and nerve root palsy. Preexisting foraminal stenosis has been associated with C5P (5,6) and some authors recommend prophylactic foraminotomy to prevent the palsy (7,8). A higher incidence of C5P has been reported in patients with ossified posterior longitudinal ligament, presumably because the spinal cord shift undergoes a wider movement after the removal of the ligament. In some studies laminectomy, laminoplasty and laminectomy plus fusion have been compared with contrasting results. Yang et al. (9) confronted laminectomy group vs. laminoplasty group reporting a higher incidence in laminectomy group. On the other hand, Basaran et al. (10), after a review of the literature, reported a higher incidence in laminoplasty compared to laminectomy, perhaps the highest incidence was found in laminectomy and fusion. The correction of cervical lordotic alignment with posterior instrumentation has been supposed as a contributing factor since able to induce iatrogenic foraminal stenosis and increase the spinal cord shift (11).
In anterior cervical decompression, the change in the intervertebral height after ACDF has been reported as a possible mechanism (12). Wang et al. (13) reported an association to cervical lordosis correction, preexistent C4/C5 foraminal stenosis and larger decompression. On the same way, the C5P has been described after single or multiple corpectomies. Bydon et al. (14) reported an incidence of 4% after single or multiple corpectomy and 1% after ACDFs. In corpectomy a wide and asymmetric anterior decompression has been supposed to determine asymmetric dural expansion and tension to the ventral rootlets (15). Hashimoto et al. (16) reported higher incidence after multilevel corpectomy respect to single level corpectomy.
Other proposed mechanisms are due to the iatrogenic injury during surgery as spinal cord ischemia and reperfusion injury. Takenaka et al. (17) proposed the use of chilled saline irrigation during bone drilling in order to reduce this damage. On the other hand, an intraoperative nerve root injury has been ruled out by Tanaka et al. (18) who monitored the intraoperative evoked potentials and no abnormalities were seen even in those patients who developed postoperative C5P.
The use of a WETC after single or multiple corpectomy was proposed to overcome the limits of the non-expandable cages as the high rates of subsidence and is considered more practical respect the expandable cages since the anterior plate is included. In literature, a case series about the use of this device for the treatment of cervical spondylosis has been recently reported with good results (19).
In this case the patient presented a preexisting right C4-C5 foraminal stenosis and we fully decompressed the foramen during the corpectomy. Nevertheless, a C5P was present on second post-operative day. We suppose that the preexisting foraminal stenosis, wide anterior decompression and partial improvement of cervical alignment were all factors contributing to the palsy.
Conclusions
In literature, many theories at the base of the onset of C5P after anterior or posterior cervical decompression have been advanced. In this case we report that the preexisting foraminal stenosis, wide anterior decompression and partial improvement of cervical alignment were all factors contributing to the palsy.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Nassr A, Eck JC, Ponnappan RK, et al. The incidence of C5 palsy after multilevel cervical decompression procedures: a review of 750 consecutive cases. Spine (Phila Pa 1976) 2012;37:174-8. [Crossref] [PubMed]
- Gu Y, Cao P, Gao R, et al. Incidence and Risk Factors of C5 Palsy following Posterior Cervical Decompression: A Systematic Review. PLoS One 2014;9:e101933. [Crossref] [PubMed]
- Bydon M, Macki M, Aygun N, et al. Development of postoperative C5 palsy is associated with wider posterior decompressions: an analysis of 41 patients. Spine J 2014;14:2861-7. [Crossref] [PubMed]
- Klement MR, Kleeman LT, Blizzard DJ, et al. C5 palsy after cervical laminectomy and fusion: does width of laminectomy matter? Spine J 2016;16:462-7. [Crossref] [PubMed]
- Imagama S, Matsuyama Y, Yukawa Y, et al. C5 palsy after cervical laminoplasty: a multicentre study. J Bone Joint Surg Br 2010;92:393-400. [Crossref] [PubMed]
- Katsumi K, Yamazaki A, Watanabe K, et al. Can prophylactic bilateral C4/C5 foraminotomy prevent postoperative C5 palsy after open-door laminoplasty?: a prospective study. Spine (Phila Pa 1976) 2012;37:748-54. [Crossref] [PubMed]
- Komagata M, Nishiyama M, Endo K, et al. Prophylaxis of C5 palsy after cervical expansive laminoplasty by bilateral partial foraminotomy. Spine J 2004;4:650-5. [Crossref] [PubMed]
- Yanase M, Matsuyama Y, Mori K, et al. Intraoperative spinal cord monitoring of C5 palsy after cervical laminoplasty. J Spinal Disord Tech 2010;23:170-5. [Crossref] [PubMed]
- Yang L, Gu Y, Shi J, et al. Modified Plate-only Open-door Laminoplasty Versus Laminectomy and Fusion for the Treatment of Cervical Stenotic Myelopathy. Orthopedics 2013;36:e79-87. [Crossref] [PubMed]
- Basaran R, Kaner T. C5 nerve root palsy following decompression of cervical spine with anterior versus posterior types of procedures in patients with cervical myelopathy. Eur Spine J 2016;25:2050-9. [Crossref] [PubMed]
- Takemitsu M, Cheung KM, Wong YW, et al. C5 nerve root palsy after cervical laminoplasty and posterior fusion with instrumentation. J Spinal Disord Tech 2008;21:267-72. [Crossref] [PubMed]
- Bai J, Zhang X, Zhang D, et al. Impact of over distraction on occurrence of axial symptom after anterior cervical discectomy and fusion. Int J Clin Exp Med 2015;8:19746-56. [PubMed]
- Wang H, Zhang X, Lv B, et al. Analysis of correlative risk factors for C5 palsy after anterior cervical decompression and fusion. Int J Clin Exp Med 2015;8:3983-91. [PubMed]
- Bydon M, Macki M, Kaloostian P, et al. Incidence and prognostic factors of c5 palsy: a clinical study of 1001 cases and review of the literature. Neurosurgery 2014;74:595-604; discussion 604-5. [Crossref] [PubMed]
- Odate S, Shikata J, Yamamura S, et al. Extremely wide and asymmetric anterior decompression causes postoperative C5 palsy: an analysis of 32 patients with postoperative C5 palsy after anterior cervical decompression and fusion. Spine (Phila Pa 1976) 2013;38:2184-9. [Crossref] [PubMed]
- Hashimoto M, Mochizuki M, Aiba A. C5 palsy following anterior decompression and spinal fusion for cervical degenerative diseases. Eur Spine J 2010;19:1702-10. [Crossref] [PubMed]
- Takenaka S, Hosono N, Mukai Y, et al. Significant reduction in the incidence of C5 palsy after cervical laminoplasty using chilled irrigation water. Bone Joint J 2016;98-B:117-24. [Crossref] [PubMed]
- Tanaka N, Nakanishi K, Fujiwara Y, et al. Postoperative segmental C5 palsy after cervical laminoplasty may occur without intraoperative nerve injury: a prospective study with transcranial electric motor-evoked potentials. Spine (Phila Pa 1976) 2006;31:3013-7. [Crossref] [PubMed]
- Tarantino R, Nigro L, Donnarumma P, et al. Cervical reconstruction techniques. After adequate selection of the patient report of a series of 34 patients treated with winged expandable cages. Neurosurg Rev 2017;40:281-6. [Crossref] [PubMed]



