
The 100 most cited manuscripts in esophageal motility disorders: a bibliometric analysis
Introduction
Esophageal motility disorders are a large group of pathologic conditions that involve both primary and secondary disorders of esophageal contraction (1). Motility disorders are considered to be primary if symptoms, such as dysphagia and chest pain, originate from the esophagus, and no other cause can be identified (1). The main primary conditions are achalasia, diffuse (distal) esophageal spasm, nutcracker esophagus, and hypertensive lower esophageal sphincter (1). The evaluation of esophageal motility disorders is mainly based on the use of manometry, and their classification is made according to the Chicago Classification system, which utilizes high-resolution manometry (HRM) (2). Although there is a fair amount of evidence for some of these disorders, such as achalasia, the data on others is not as granular.
Bibliometric citation analysis is a quantitative method that uses the number of citations received by scientific articles to develop citation ranking lists, in order to assess the quality and scientific impact of those articles (3). A publication receives a citation when another peer-reviewed publication references it. By establishing citation ranking lists, we can identify the most influential articles on a specific topic or scientific discipline and their impact on clinical practice. Bibliometric analysis can also provide insight into how our understanding of those topics or disciplines has evolved over the years (3).
In recent years, bibliometric citation analysis has been used to identify the most influential articles in various medical disciplines and specialties, such as plastic (4), orthopaedic (5), general (6), and emergency general surgery (7) as well as oncology (8). To date, the only bibliometric analysis in the field of esophageal diseases is on the topic of esophageal cancer (9). The purpose of this study is to determine which articles are the most cited and, therefore, influential on the subject of esophageal motility disorders and to examine how our understanding of these diseases has changed over time. It also aims to serve as a concise reference for the most cited papers on the subject.
Methods
Search methodology
The Web of Science citation indexing database and research platform of Clarivate Analytics was used to perform the study. The search strategy was to identify articles that contained specific search terms/keywords in their title, abstract or topic. After independent trial searches by two authors (P Kapsampelis, D Schizas), the following keywords were agreed upon and used in the final search: (esophag* OR oesophag*) AND (achalasia OR motility OR dysmotility OR spasm OR peristal* OR hypercontract* OR nutcracker OR hypertens* OR hypotens* OR sphincter* OR contraction* OR manometry OR dysphagia OR obstruction). The search was set to include results from all the databases within the Web of Science and all available years [1900–2018]. Also, it was set to include articles written only in the English language. The final search date was August 15th, 2018. This strategy is a modified version of the method initially developed by Paladugu and colleagues (6).
Article selection
The returned results were sorted by the total number of citations, in descending order, and reviewed for inclusion, with the article with the most citations examined first. Papers focusing on esophageal motility disorders as their main topic and written in the English language were included. The exclusion criteria were: (I) articles written in any language other than English; (II) articles irrelevant to the subject; or (III) articles focusing on broader topics, such as esophageal and gastrointestinal diseases in general, without giving specific emphasis to esophageal motility disorders.
Initially, two reviewers (P Kapsampelis, D Schizas) independently assessed abstracts for inclusion. Consequently, the two lists were compared and full manuscripts of articles were reviewed, when deemed necessary. After conflicts were resolved by a third author (DI Tsilimigras) and the list of 100 most cited papers was finalized, the full manuscripts of included papers were analyzed to extract the data of interest.
Data extraction
The 100 most cited articles were analyzed for title, names of first author and co-authors, institution and country of the first author, year of publication, total number of citations and citation rate. The ranking within the 100 most cited papers list was also recorded. The purpose of calculating the citation rate was to control for historical publication bias since older articles can accumulate more citations over time. In a method described by Powell et al. (10), the citation rate is calculated by dividing a publication’s number of citations by the number of years since its publication. Also, in the case of articles with same citation numbers, the ranking was done according to the citation rate and articles that received the same number of citations in a shorter period of time were ranked higher.
Results
The Web of Science search returned 29,521 full-length, English language papers. Table 1 lists the 100 most cited papers. The total cumulative number of citations received by the top 100 articles was 20,688. The article with the highest number of citations was “Peroral endoscopic myotomy (POEM) for esophageal achalasia” by Inoue et al., receiving 665 citations (11).
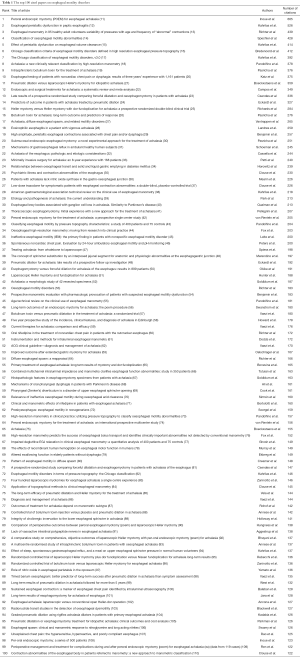
Full table
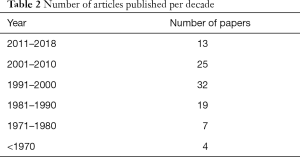
The oldest manuscript featured in the top 100 list was by Merendino et al. (“The concept of sphincter substitution by an interposed jejunal segment for anatomic and physiologic abnormalities at the esophagogastric junction”) and published in 1955 (48). “The Chicago classification of esophageal motility disorders, version 3.0” by Kahrilas et al. and “Per-oral endoscopic myotomy: a series of 500 patients” by Inoue et al. (17,108) were the most recent manuscripts, both published in 2015. Table 2 lists the number of articles from the top 100 list published in each decade.
Full table
To address the issue of historical bias, we calculated the citation rate of the manuscripts in the top 100 list. Table 3 shows the top 10 papers with the highest citation rate. “The Chicago classification of esophageal motility disorders, version 3.0” by Kahrilas et al., published in 2015, was the article with the highest citation rate (13,067 citations per year) (17).

Full table
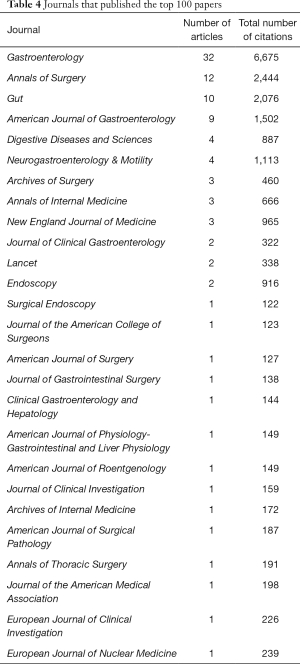
The 100 most influential papers appeared in 26 journals (Table 4). The number of manuscripts per journal ranged from 1 to 32. The journal Gastroenterology featured the highest number of papers and accrued the highest total number of citations (32 articles and 6,675 citations respectively). Following that, Annals of Surgery had 12 manuscripts and 2,444 total citations and Gut had 10 manuscripts and 2,076 total citations. Endoscopy published the most cited paper in the top 100 list [“Peroral endoscopic myotomy (POEM) for esophageal achalasia” by Inoue et al.] (11).
Full table
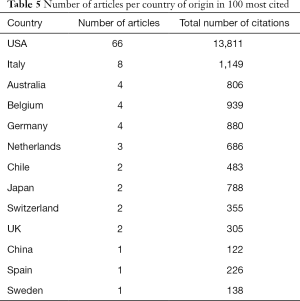
The United States of America was the country that produced most publications, with 66 out of 100 articles, followed by Italy with 8 publications (Table 5). Belgium, Australia, and Germany had 4 publications each. Most manuscripts in the top 100 list originated from Northwestern University (13 manuscripts) (Table 6). Northwestern University was also the institution that accrued the highest total number of citations (3,238 citations). Showa University Northern Yokohama Hospital in Japan produced the most cited manuscript in the top 100 list [“Peroral endoscopic myotomy (POEM) for esophageal achalasia” by Inoue et al.] (11).
Full table
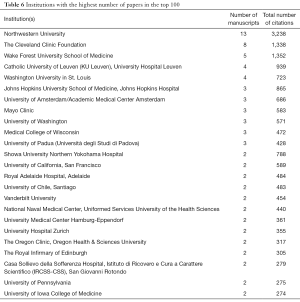
Full table
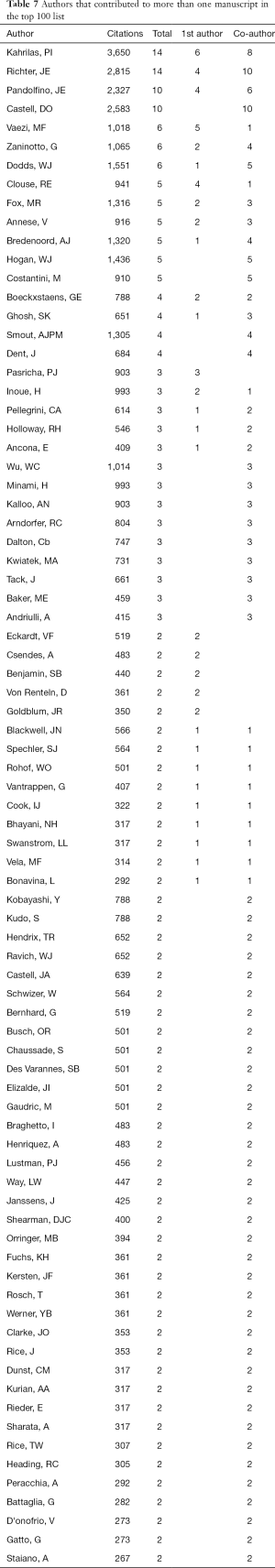
Table 7 lists all the authors that contributed to more than one manuscript, either as the 1st authors or as co-authors. Out of a total of 367 authors, 81 participated in the authorship of more than one publications featured in the top 100 list. Peter Kahrilas from Northwestern University was the most cited author (3,650 total citations), followed by Joel Richter from the University of South Florida (2,815 citations). Peter Kahrilas had 6 articles as the 1st author and 8 articles as co-author. Joel Richter had 4 articles as the 1st author and 10 articles as co-author.
Full table
Discussion
This bibliometric analysis is the first of its kind to study the most cited papers on the topic of esophageal motility disorders. The article with the highest total number of citations and second highest citation rate is the one entitled “Peroral endoscopic myotomy (POEM) for esophageal achalasia” and was performed by Inoue et al. from Showa University Northern Yokohama Hospital in Japan (11). This article was the first description of POEM, a technique developed by Inoue and his colleagues to treat esophageal achalasia with the use of endoscopic surgery. Their short-term outcomes were excellent opening the way towards less invasive permanent treatment methods for esophageal achalasia (11). This technique was widely accepted as an alternative to surgical myotomy, and some years later, Inoue et al. published a large series of 500 patients who underwent POEM at their institution confirming the safety and efficacy of this approach (108). The second most cited article is “Esophageal peristaltic dysfunction in peptic esophagitis” by Kahrilas et al. from the Northwestern University (12). In this article, the authors examined the association of reflux esophagitis with esophageal motility, reporting an increasing prevalence of peristaltic dysfunction with worsening esophagitis (12). In fact, abnormal peristalsis was identified in 25% of patients with mild esophagitis and 48% of patients with severe esophagitis (12). This was one of the first studies to show the association between the reflux of gastric acid and the disturbances in esophageal peristalsis, thus attracting much attention mainly due to the significant clinical implications of these findings (12).
Most papers in the top 100 list were published in more recent decades. Seventy [70] out of the 100 papers were published after 1990 and 57 of them were published between 1991–2010 (Table 2). Possible explanations for this trend could be the increased use of manometry in evaluating esophageal motility, as well as the introduction of novel therapeutic approaches, mainly for the treatment of achalasia.
Also, manuscripts published in recent years had generally higher citation rates and this may imply that these will accrue more citations and become even more influential within the next years (Table 2). The citation rate index for the most influential articles on esophageal motility disorders ranged from 34.17 to 130.67 (Table 3). The comparison with the citation rate index of other subjects shows that esophageal motility disorders accrue citations at a slower rate. For example, in a bibliometric analysis of the most influential papers on esophageal cancer by Powell et al., the citation rate index ranged from 69 to 227 (9). “The Chicago classification of esophageal motility disorders, version 3.0” by Kahrilas et al. is the article with the highest citation rate and was published in 2015 (17). The Chicago Classification system uses HRM to categorize esophageal motility disorders and all versions of this system are featured in the top 100 list.
The majority of manuscripts were published in the journal Gastroenterology, followed by Annals of Surgery and Gut. Most manuscripts were published in journals in the field of gastroenterology (56 articles), as opposed to manuscripts published in surgery journals (21) and general and internal medicine journals (12). Accordingly, the majority of the manuscripts with the highest number of citations or the highest citation rate were published in gastroenterology journals (Tables 1,3).
Out of the 367 authors, 12 had more than 1,000 citations and only 4 had more than 2,000 citations. The most cited author was Peter Kahrilas from Northwestern University, followed by Joel Richter from the University of South Florida. The third and fourth most cited authors were Donald Castell from the Medical University of South Carolina and John Pandolfino from Northwestern University. These four authors were also the most published ones in terms of publication volume. Kahrilas and Richter authored 14 manuscripts each, whereas Castell and Pandolfino authored 10 manuscripts each.
The main limitation of this study is that some types of bias might have impacted the results. Self-citation, powerful person bias, institutional bias or geographical bias may have caused disproportionate number of citations. Language bias may also be present, mainly because the search was limited to manuscripts only in the English language. Another issue that has to be taken into consideration is the possibility of historical bias; older publications often have a higher number of citations because they accumulated citations over many years, regardless of their scientific impact. We tried to address this issue by calculating the citation rate of the articles, in addition to their citation number. Nevertheless, the scientific impact of an article may be underestimated or overestimated with this study format. On the one hand, articles need a certain lead-time to start receiving citations. On the other hand, the likelihood of receiving citations rises with the increasing numbers of articles being published in peer-reviewed journals.
This citation analysis is the first to examine the most cited papers on the disorders of esophageal motility and can serve as a reference on the manuscripts, authors, and institutions that defined our understanding of the subject. Researchers and clinicians can also use this analysis to examine what are the key characteristics of citable articles. Finally, by studying the most impactful papers, researchers can determine the future directions in the research on esophageal motility disorders.
Acknowledgments
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
References
- Patti MG, Herbella FA. Achalasia and Other Esophageal Motility Disorders. J Gastrointest Surg 2011;15:703-7. [Crossref] [PubMed]
- Bowers SP. Esophageal Motility Disorders. Surg Clin North Am 2015;95:467-82. [Crossref] [PubMed]
- Murray MR, Wang T, Schroeder GD, et al. The 100 most cited spine articles. Eur Spine J 2012;21:2059-69. [Crossref] [PubMed]
- Loonen MPJ, Hage JJ, Kon M. Plastic surgery classics: Characteristics of 50 top-cited articles in four plastic surgery journals since 1946. Plast Reconstr Surg 2008;121:320e-7e. [Crossref] [PubMed]
- Kelly JC, Glynn RW, O’Briain DE, et al. The 100 classic papers of orthopaedic surgery. J Bone Joint Surg Br 2010;92:1338-43. [Crossref] [PubMed]
- Paladugu R, Schein M, Gardezi S, et al. One hundred citation classics in general surgical journals. World J Surg 2002;26:1099-105. [Crossref] [PubMed]
- Ellul T, Bullock N, Abdelrahman T, et al. The 100 most cited manuscripts in emergency abdominal surgery: A bibliometric analysis. Int J Surg 2017;37:29-35. [Crossref] [PubMed]
- Tas F. An analysis of the most-cited research papers on oncology: Which journals have they been published in? Tumour Biol 2014;35:4645-9. [Crossref] [PubMed]
- Powell AGMT, Hughes DL, Brown J, et al. Esophageal cancer’s 100 most influential manuscripts: A bibliometric analysis. Dis Esophagus 2017;30:1-8. [Crossref] [PubMed]
- Powell AGMT, Hughes DL, Wheat JR, et al. The 100 Most Influential Manuscripts in Gastric Cancer: A Bibliometric Analysis. Int J Surg 2016;28:83-90. [Crossref] [PubMed]
- Inoue H, Minami H, Kobayashi Y, et al. Peroral endoscopic myotomy (POEM) for esophageal achalasia. Endoscopy 2010;42:265-71. [Crossref] [PubMed]
- Kahrilas PJ, Dodds WJ, Hogan WJ, et al. Esophageal Peristaltic Dysfunction in Peptic Esophagitis. Gastroenterology 1986;91:897-904. [Crossref] [PubMed]
- Richter JE, Wu WC, Johns DN, et al. Esophageal Manometry in 95 Healthy Adult Volunteers - Variability of Pressures with Age and Frequency of “Abnormal” Contractions. Dig Dis Sci 1987;32:583-92. [Crossref] [PubMed]
- Spechler SJ, Castell DO. Classification of oesophageal motility abnormalities. Gut 2001;49:145-51. [Crossref] [PubMed]
- Kahrilas PJ, Dodds WJ, Hogan WJ. Effect of peristaltic dysfunction on esophageal volume clearance. Gastroenterology 1988;94:73-80. [Crossref] [PubMed]
- Bredenoord AJ, Fox M, Kahrilas PJ, et al. Chicago classification criteria of esophageal motility disorders defined in high resolution esophageal pressure topography. Neurogastroenterol Motil 2012;24:57-65. [Crossref] [PubMed]
- Kahrilas PJ, Bredenoord AJ, Fox MR, et al. The Chicago Classification of esophageal motility disorders, v3.0. Neurogastroenterol Motil 2015;27:160-74. [Crossref] [PubMed]
- Pandolfino JE, Kwiatek MA, Nealis T, et al. Achalasia: A New Clinically Relevant Classification by High-Resolution Manometry. Gastroenterology 2008;135:1526-33. [Crossref] [PubMed]
- Pasricha PJ, Ravich WJ, Hendrix TR, et al. Intrasphincteric Botulinum Toxin for the Treatment of Achalasia. N Engl J Med 1995;332:774-8. [Crossref] [PubMed]
- Katz PO, Dalton CB, Richter JE, et al. Esophageal Testing of Patients with Noncardiac Chest pain or Dysphagia. Results of Three Years’ Experience with 1161 patients. Ann Intern Med 1987;106:593-7. [Crossref] [PubMed]
- Boeckxstaens GE, Annese V, Varannes SB, des , et al. Pneumatic Dilation versus Laparoscopic Heller’s Myotomy for Idiopathic Achalasia. N Engl J Med 2011;364:1807-16. [Crossref] [PubMed]
- Campos GM, Vittinghoff E, Rabl C, et al. Endoscopic and Surgical Treatments for Achalasia: A Systematic Review and Meta-Analysis. Ann Surg 2009;249:45-57. [Crossref] [PubMed]
- Csendes A, Braghetto I, Henriquez A, et al. Late results of a prospective randomised study comparing forceful dilatation and oesophagomyotomy in patients with achalasia. Gut 1989;30:299-304. [Crossref] [PubMed]
- Eckardt VF, Aignherr C, Bernhard G. Predictors of Outcome in Patients With Achalasia Treated by Pneumatic Dilation. Gastroenterology 1992;103:1732-8. [Crossref] [PubMed]
- Richards WO, Torquati A, Holzman MD, et al. Heller Myotomy Versus Heller Myotomy With Dor Fundoplication for Achalasia: A Prospective Randomized Double-Blind Clinical Trial. Ann Surg 2004;240:405-12. [Crossref] [PubMed]
- Pasricha PJ, Rai R, Ravich WJ, et al. Botulinum toxin for achalasia: Long-term outcome and predictors of response. Gastroenterology 1996;110:1410-5. [Crossref] [PubMed]
- Vantrappen G, Janssens J, Hellemans J, et al. Achalasia, Diffuse Esophageal Spasm, and Related Motility Disorders. Gastroenterology 1979;76:450-7. [PubMed]
- Landres RT, Kuster GG, Strum WB. Eosinophilic Esophagitis in A Patient With Vigorous Achalasia. Gastroenterology 1978;74:1298-301. [Crossref] [PubMed]
- Benjamin SB, Gerhardt DC, Castell DO. High Amplitude, Peristaltic Esophageal Contractions Associated with Chest Pain and/or Dysphagia. Gastroenterology 1979;77:478-83. [Crossref] [PubMed]
- Pasricha PJ, Hawari R, Ahmed I, et al. Submucosal endoscopic esophageal myotomy: a novel experimental approach for the treatment of achalasia. Endoscopy 2007;39:761-4. [Crossref] [PubMed]
- Schoeman MN, Tippett MD, Akkermans LMA, et al. Mechanisms of Gastroesophageal Reflux in Ambulant Healthy Human Subjects. Gastroenterology 1995;108:83-91. [Crossref] [PubMed]
- Cassella RR, Brown AL, Sayre GP, et al. Achalasia of the Esophagus: Pathologic and Etiologic Considerations. Ann Surg 1964;160:474-87. [Crossref] [PubMed]
- Patti MG, Pellegrini CA, Horgan S, et al. Minimally Invasive Surgery for Achalasia: An 8-Year Experience With 168 Patients. Ann Surg 1999;230:587-93. [Crossref] [PubMed]
- Horowitz M, Maddox AF, Wishart JM, et al. Relationships between oesophageal transit and solid and liquid gastric emptying in diabetes mellitus. Eur J Nucl Med 1991;18:229-34. [Crossref] [PubMed]
- Clouse RE, Lustman PJ. Psychiatric Illness and Contraction Abnormalities of the Esophagus. N Engl J Med 1983;309:1337-42. [Crossref] [PubMed]
- Mearin F, Mourelle M, Guarner F, et al. Patients with achalasia lack nitric oxide synthase in the gastro‐oesophageal junction. Eur J Clin Invest 1993;23:724-8. [Crossref] [PubMed]
- Clouse RE, Lustman PJ, Eckert TC, et al. Low-Dose Trazodone for Symptomatic Patients With Esophageal Contraction Abnormalities: A Double-Blind, Placebo-Controlled Trial. Gastroenterology 1987;92:1027-36. [Crossref] [PubMed]
- Kahrilas PJ, Clouse RE, Hogan WJ. American gastroenterological association technical review on the clinical use of esophageal manometry. Gastroenterology 1994;107:1865-84. [Crossref] [PubMed]
- Park W, Vaezi MF. Etiology and Pathogenesis of Achalasia: The Current Understanding. Am J Gastroenterol 2005;100:1404-14. [Crossref] [PubMed]
- Qualman SJ, Haupt HM, Yang P, et al. Esophageal Lewy Bodies Associated with Ganglion Cell loss in Achalasia. Similarity to Parkinson’s Disease. Gastroenterology 1984;87:848-56. [Crossref] [PubMed]
- Pellegrini C, Wetter LA, Patti MG, et al. Esophagomyotomy Initial Experience With a New Approach for the Treatment ofAchalasia. Ann Surg 1992;216:291-6. [Crossref] [PubMed]
- von Renteln D, Inoue H, Minami H, et al. Peroral Endoscopic Myotomy for the Treatment of Achalasia: A Prospective Single Center Study. Am J Gastroenterol 2012;107:411-7. [Crossref] [PubMed]
- Pandolfino JE, Ghosh SK, Rice J, et al. Classifying Esophageal Motility by Pressure Topography Characteristics: A Study of 400 Patients and 75 Controls. Am J Gastroenterol 2008;103:27-37. [Crossref] [PubMed]
- Fox MR, Bredenoord AJ. Oesophageal high-resolution manometry: moving from research into clinical practice. Gut 2008;57:405-23. [Crossref] [PubMed]
- Leite LP, Johnston BT, Barrett J, et al. Ineffective Esophageal Motility (IEM): The Primary Finding in Patients with Nonspecific Esophageal Motility Disorder. Dig Dis Sci 1997;42:1859-65. [Crossref] [PubMed]
- Peters L, Maas L, Petty D, et al. Spontaneous Noncardiac Chest Pain: Evaluation by 24-Hour Ambulatory Esophageal Motility and pH Monitoring. Gastroenterology 1988;94:878-86. [Crossref] [PubMed]
- Spiess AE, Kahrilas PJ. Treating Achalasia: From Whalebone to Laparoscope. JAMA 1998;280:638-42. [Crossref] [PubMed]
- Merendino KA, Dillard DH. The Concept of Sphincter Substitution by an Interposed Jejunal Segment for Anatomic and Physiologic Andomalities at the Esophagogastric Junction. Ann Surg 1955;142:486-506. [Crossref] [PubMed]
- Eckardt VF, Gockel I, Bernhard G. Pneumatic dilation for achalasia: late results of a prospective follow up investigation. Gut 2004;53:629-33. [Crossref] [PubMed]
- Okike N, Payne WS, Neufeld DM, et al. Esophagomyotomy versus Forceful Dilation for Achalasia of the Esophagus: Results in 899 Patients. Ann Thorac Surg 1979;28:119-25. [Crossref] [PubMed]
- Hunter JG, Trus TL, Branum GD, et al. Laparoscopic Heller Myotomy and Fundoplication for Achalasia. Ann Surg 1997;225:655-64. [Crossref] [PubMed]
- Goldblum JR, Whyte RI, Orringer MB, Appelman HD. Achalasia: A Morphologic Study of 42 Resected Specimens. Am J Surg Pathol 1994;18:327-37. [Crossref] [PubMed]
- Richter JE. Oesophageal motility disorders. Lancet 2001;358:823-8. [Crossref] [PubMed]
- Benjamin SB, Richter JE, Cordova CM, et al. Prospective Manometric Evaluation with Pharmacologic Provocation of Patients with Suspected Esophageal Motility Dysfunction. Gastroenterology 1983;84:893-901. [Crossref] [PubMed]
- Pandolfino JE, Kahrilas PJ. AGA Technical Review on the Clinical Use of Esophageal Manometry. Gastroenterology 2005;128:209-24. [Crossref] [PubMed]
- Swanstrom LL, Kurian AA, Dunst CM, et al. Long-Term Outcomes of an Endoscopic Myotomy for Achalasia: The POEM Procedure. Ann Surg 2012;256:659-67. [Crossref] [PubMed]
- Vaezi MF, Richter JE, Wilcox CM, et al. Botulinum toxin versus pneumatic dilatation in the treatment of achalasia: A randomized trial. Gut 1999;44:231-9. [Crossref] [PubMed]
- Howard PJ, Maher L, Pryde A, et al. Five year prospective study of the incidence, clinical features, and diagnosis of achalasia in Edinburgh. Gut 1992;33:1011-5. [Crossref] [PubMed]
- Vaezi MF, Richter JE. Current Therapies for Achalasia. J Clin Gastroenterol 1998;27:21-35. [Crossref] [PubMed]
- Richter JE, Dalton CB, Bradley LA, et al. Oral Nifedipine In The Treatment Of Noncardiac Chest Pain In Patients With The Nutcracker Esophagus. Gastroenterology 1987;93:21-8. [Crossref] [PubMed]
- Dodds WJ. Instrumentation and Methods for Intraluminal Esophageal Manometry. Arch Intern Med 1976;136:515-23. [Crossref] [PubMed]
- Vaezi MF, Pandolfino JE, Vela MF. ACG clinical guideline: Diagnosis and management of achalasia. Am J Gastroenterol 2013;108:1238-49. [Crossref] [PubMed]
- Oelschlager BK, Chang L, Pellegrini CA, et al. Improved Outcome After Extended Gastric Myotomy for Achalasia. Arch Surg 2003;138:490-5. [Crossref] [PubMed]
- Richter JE, Castell DO. Diffuse Esophageal Spasm: A Reappraisal. Ann Intern Med 1984;100:242-5. [Crossref] [PubMed]
- Bonavina L, Nosadini A, Bardini R, et al. Primary Treatment of Esophageal Achalasia: Long-term Results of Myotomy and Dor Fundoplication. Arch Surg 1992;127:222-6. [Crossref] [PubMed]
- Tutuian R, Castell DO. Combined Multichannel Intraluminal Impedance and Manometry Clarifies Esophageal Function Abnormalities: Study in 350 Patients. Am J Gastroenterol 2004;99:1011-9. [Crossref] [PubMed]
- Goldblum JR, Rice TW, Richter JE. Histopathologic features in esophagomyotomy specimens from patients with achalasia. Gastroenterology 1996;111:648-54. [Crossref] [PubMed]
- Ali GN, Wallace KL, Schwartz R, et al. Mechanisms of Oral-Pharyngeal Dysphagia in Patients With Parkinson’s Disease. Gastroenterology 1996;110:383-92. [Crossref] [PubMed]
- Cook IJ, Gabb M, Panagopoulos V, et al. Pharyngeal (Zenker’s) Diverticulum is A Disorder of Upper Esophageal Sphincter Opening. Gastroenterology 1992;103:1229-35. [Crossref] [PubMed]
- Simrén M, Silny J, Holloway RH, Tack J, et al. Relevance of ineffective oesophageal motility during oesophageal acid clearance. Gut 2003;52:784-90. [Crossref] [PubMed]
- Bortolotti M, Labo G. Clinical and Manometric Effects of Nifedipine in Patients with Esophageal Achalasia. Gastroenterology 1981;80:39-44. [Crossref] [PubMed]
- Soergel KH, Zboralske FF, Amberg JR. Presbyesophagus: Esophageal Motility in Nonagenarians. J Clin Invest 1964;43:1472-9. [Crossref] [PubMed]
- Pandolfino JE, Fox MR, Bredenoord AJ, et al. High-resolution manometry in clinical practice: Utilizing pressure topography to classify oesophageal motility abnormalities. Neurogastroenterol Motil 2009;21:796-806. [Crossref] [PubMed]
- Von Renteln D, Fuchs K-H, Fockens P, et al. Peroral Endoscopic Myotomy for the Treatment of Achalasia: An International Prospective Multicenter Study. Gastroenterology 2013;145:309-11.e1. [Crossref] [PubMed]
- Boeckxstaens GE, Zaninotto G, Richter JE. Achalasia. Lancet 2014;383:83-93. [Crossref] [PubMed]
- Fox M, Hebbard GS, Janiak P, et al. High-resolution manometry predicts the success of oesophageal bolus transport and identifies clinically important abnormalities not detected by conventional manometry. Neurogastroenterol Motil 2004;16:533-42. [Crossref] [PubMed]
- Ghosh SK, Pandolfino JE, Rice J, et al. Impaired deglutitive EGJ relaxation in clinical esophageal manometry: a quantitative analysis of 400 patients and 75 controls. Am J Physiol - Gastrointest Liver Physiol 2007;293:G878-85. [Crossref] [PubMed]
- Murray JA, Ledlow A, Launspach J, et al. The Effects of Recombinant Human Hemoglobin on Esophageal Motor Function in Humans. Gastroenterology 1995;109:1241-8. [Crossref] [PubMed]
- Ekberg O, Feinberg MJ. Altered Swallowing Function in Elderly Patients without Dysphagia: Radiologic Findings in 56 Cases. AJR Am J Roentgenol 1991;156:1181-4. [Crossref] [PubMed]
- Creamer B, Donoghue FE, Code CF. Pattern of Esophageal Motility in Diffuse Spasm. Gastroenterology 1958;34:782-96. [Crossref] [PubMed]
- Csendes A, Velasco N, Braghetto I, et al. A Prospective Randomized Study Comparing Forceful Dilatation and Esophagomyotomy in Patients with Achalasia of the Esophagus. Gastroenterology 1981;80:789-95. [Crossref] [PubMed]
- Kahrilas PJ, Ghosh SK, Pandolfino JE. Esophageal Motility Disorders in Terms of Pressure Topography: The Chicago Classification. J Clin Gastroenterol 2008;42:627-35. [Crossref] [PubMed]
- Zaninotto G, Costantini M, Rizzetto C, et al. Four Hundred Laparoscopic Myotomies for Esophageal Achalasia: A Single Centre Experience. Ann Surg 2008;248:986-93. [Crossref] [PubMed]
- Clouse RE, Staiano A, Alrakawi A, et al. Application of Topographical Methods to Clinical Esophageal Manometry. Am J Gastroenterol 2000;95:2720-30. [Crossref] [PubMed]
- Vela MF, Richter JE, Khandwala F, et al. The Long-term Efficacy of Pneumatic Dilatation and Heller Myotomy for the Treatment of Achalasia. Clin Gastroenterol Hepatol 2006;4:580-7. [Crossref] [PubMed]
- Vaezi MF, Richter JE. Diagnosis and Management of Achalasia. Am J Gastroenterol 1999;94:3406-12. [Crossref] [PubMed]
- Rohof WO, Salvador R, Annese V, et al. Outcomes of Treatment for Achalasia Depend on Manometric Subtype. Gastroenterology 2013;144:718-25. [Crossref] [PubMed]
- Annese V, Basciani M, Perri F, et al. Controlled Trial of Botulinum Toxin Injection Versus Placebo and Pneumatic Dilation in Achalasia. Gastroenterology 1996;111:1418-24. [Crossref] [PubMed]
- Holloway RH, Dodds WJ, Helm JF, et al. Integrity of cholinergic innervation to the lower esophageal sphincter in achalasia. Gastroenterology 1986;90:924-9. [Crossref] [PubMed]
- Hungness ES, Teitelbaum EN, Santos BF, et al. Comparison of Perioperative Outcomes Between Peroral Esophageal Myotomy (POEM) and Laparoscopic Heller Myotomy. J Gastrointest Surg 2013;17:228-35. [Crossref] [PubMed]
- Aggestrup S, Uddman R, Sundler F, et al. Lack of Vasoactive Intestinal Polypeptide Nerves in Esophageal Achalasia. Gastroenterology 1983;84:924-7. [Crossref] [PubMed]
- Bhayani NH, Kurian AA, Dunst CM, et al. A Comparative Study on Comprehensive, Objective Outcomes of Laparoscopic Heller Myotomy With Per-Oral Endoscopic Myotomy (POEM) for Achalasia. Ann Surg 2014;259:1098-103. [Crossref] [PubMed]
- Annese V, Bassotti G, Coccia F, et al. A multicentre randomised study of intrasphincteric botulinum toxin in patients with oesophageal achalasia. Gut 2000;46:597-600. [Crossref] [PubMed]
- Kahrilas PJ, Dodds WJ, Dent J, et al. Effect of Sleep, Spontaneous Gastroesophageal Reflux, and a Meal on Upper Esophageal Sphincter Pressure in Normal Human Volunteers. Gastroenterology 1987;92:466-71. [Crossref] [PubMed]
- Rebecchi F, Giaccone C, Farinella E, et al. Randomized Controlled Trial of Laparoscopic Heller Myotomy Plus Dor Fundoplication Versus Nissen Fundoplication for Achalasia: Long-Term Results. Ann Surg 2008;248:1023-30. [Crossref] [PubMed]
- Zaninotto G, Annese V, Costantini M, et al. Randomized Controlled Trial of Botulinum Toxin Versus Laparoscopic Heller Myotomy for Esophageal Achalasia. Ann Surg 2004;239:364-70. [Crossref] [PubMed]
- Yamato S, Specler SJ, Goyal RK. Role of Nitric Oxide in Esophageal Peristalsis in the Opossum. Gastroenterology 1992;103:197-204. [Crossref] [PubMed]
- Vaezi MF, Baker ME, Achkar E, et al. Timed barium oesophagram: better predictor of long term success after pneumatic dilation in achalasia than symptom assessment. Gut 2002;50:765-70. [Crossref] [PubMed]
- West RL, Hirsch DP, Bartelsman JFWM, et al. Long Term Results of Pneumatic Dilation in Achalasia Followed for More Than 5 Years. Am J Gastroenterol 2002;97:1346-51. [Crossref] [PubMed]
- Balaban DH, Yamamoto Y, Liu J, et al. Sustained Esophageal Contraction: A Marker of Esophageal Chest Pain Identified by Intraluminal Ultrasonography. Gastroenterology 1999;116:29-37. [Crossref] [PubMed]
- Jara FM, Toledo Pereyra LH, Lewis JW, et al. Long-term Results of Esophagomyotomy for Achalasia of Esophagus. Arch Surg 1979;114:935-6. [Crossref] [PubMed]
- Ancona E, Anselmino M, Zaninotto G, et al. Esophageal achalasia: Laparoscopic versus conventional open heller-dor operation. Am J Surg 1995;170:265-70. [Crossref] [PubMed]
- Blackwell JN, Hannan WJ, Adam RD, et al. Radionuclide transit studies in the detection of oesophageal dysmotility. Gut 1983;24:421-6. [Crossref] [PubMed]
- Kadakia SC, Wong RKH. Graded Pneumatic Dilation using Rigiflex Achalasia Dilators in Patients with Primary Esophageal Achalasia. Am J Gastroenterol 1993;88:34-8. [PubMed]
- Parkman HP, Reynolds JC, Ouyang A, et al. Pneumatic Dilatation or Esophagomyotomy Treatment For Idiopathic Achalasia: Clinical Outcomes and Cost Analysis. Dig Dis Sci 1993;38:75-85. [Crossref] [PubMed]
- Swamy N. Esophageal Spasm: Clinical and Manometric Response to Nitroglycerine and Long Acting Nitrites. Gastroenterology 1977;72:23-7. [PubMed]
- Rao SSC, Gregersen H, Hayek B, et al. Unexplained Chest Pain: The Hypersensitive, Hyperreactive, and Poorly Compliant Esophagus. Ann Intern Med 1996;124:950-8. [Crossref] [PubMed]
- Inoue H, Sato H, Ikeda H, et al. Per-Oral Endoscopic Myotomy: A Series of 500 Patients. J Am Coll Surg 2015;221:256-64. [Crossref] [PubMed]
- Ren Z, Zhong Y, Zhou P, et al. Perioperative management and treatment for complications during and after peroral endoscopic myotomy (POEM) for esophageal achalasia (EA) (data from 119 cases). Surg Endosc 2012;26:3267-72. [Crossref] [PubMed]
- Clouse RE, Staiano A. Contraction Abnormalities of the Esophageal Body in Patients Referred to Manometry. A New Approach to Manometric Classification. Dig Dis Sci 1983;28:784-91. [Crossref] [PubMed]


