
Association between N-terminal pro-BNP and 12 months major adverse cardiac events among patients admitted with NSTEMI
Introduction
Non-ST-elevation myocardial infarction (NSTEMI), an important subtype of ACS, is a cardiac pathology characterized by troponin elevation, which suggests heart damage, but no ST elevation is observable on electrocardiogram (ECG) (1). NSTEMI is critically urgent due to its high morbidity and mortality rates (2,3). It has been reported that the rates of death, myocardial infarction (MI), and recurrent instability in contemporary registries are greater than 10% by 12 months (1). The hospital admission rates of NSTEMI are increasing (about 11-fold from 2001 to 2011), and a forthcoming transition from ST-elevation myocardial infarction (STEMI) to NSTEMI has been observed in China (4).
NT-proBNP is a prohormone that is secreted by cardiomyocytes, N-terminal 76 amino-acid cleavage product of proBNP, mainly in response to increased cardiac chamber wall-filling stress, which is then released into the peripheral circulation. After acute myocardial ischemia, the production of NT-proBNP is upregulated secondary to the local stretch mechanismin the area surrounding the ischemic region (5). NT-proBNP and BNP are released from the same precursor, proBNP; BNP is bioactive, while NT-proBNP is not. NT-proBNP is more stable and has a relatively long half-life in the human body (6), and its prognostic values for short-time mortality have been reported. The prognostic value of elevated NT-proBNP was reported in recent years, and the most studied outcome was in-hospital/30-day mortality (7-9). However, the association between NT-proBNP levels and long-term major adverse cardiac events (MACEs) has rarely been reported, and the subgroup of patients who could potentially benefit from NT-proBNP measurement remains unclear.
In this study, we analyzed the 12-month predictive value of NT-proBNP in a large NSTEMI population. We also assessed the GRACE risk score’s additional value in the Tianjin Inpatient Acute Myocardial Infarction Registry (TAMI) cohort, a registered multicenter (36 hospitals) observational cohort study from Tianjin, China. Based on the NSTEMI patients from TAMI, we aim to demonstrate the relationship between NT-proBNP and MACEs in patients with NSTEMI within 12 months after discharge. Furthermore, we explored the subgroup of patients who could potentially benefit from NT-proBNP measurement. We hypothesize that NT-proBNP is a robust prognostic biomarker and integrating NT-proBNP and the GRACE score could help improve the prediction of MACEs in patients with NSTEMI within 12 months after discharge. We present the following article following the STROBE reporting checklist (available at http://dx.doi.org/10.21037/apm-20-2538).
Methods
Study population
From January 2018 to December 2018, a total of 1,357 consecutive Chinese patients with NSTEMI from TAMI, registered at ClinicalTrials.gov (identifier NCT03600259), were enrolled. The diagnosis and treatment methods were systematically determined using current clinical guidelines (10), physicians’ judgments, and patients’ preferences. The eligibility criteria were as follows: (I) patients age ≥18, and (II) patients definitively diagnosed with NSTEMI. Patients were ineligible if their ECG were persistent ST-segment elevation or their chest pain was differentially diagnosed as a non-cardiac cause, such as aortic dissection, pulmonary embolism, etc. The diagnostic criteria were as follows: (I) clinical presentation is compatible with myocardial ischemia; (II) a dynamic elevation of cardiac troponin above the 99th percentile of healthy individuals. The study was conducted following the Declaration of Helsinki (as revised in 2013). The ethics board approved Tianjin Chest Hospital’s study (No. 2018KY-010-01), and informed consent was obtained from all individual participants.
Data collection
We collected data at the initial presentation, including patient demographics (age, gender, smoking, and drinking status), admission features (heart rate, left main involvement, systolic and diastolic pressure, LVEF, Killip class, GRACE score, and occluded lesion), complications (hypertension, diabetes, hyperlipidaemia, previous stroke, and previous MI), medical therapy (DAPT, beta-blockers, ACEI/ARBs, statins, anticoagulants), and laboratory tests (HDLC, LDLC, NT-proBNP, and hs-TnT). Measurement of NT-proBNP and hs-TnT were performed using Roche Diagnostics (Mannheim, Germany), which provided high reproducibility (11). Blood samples were obtained from the patients within 12 hours after presentation. All samples were centrifuged at 3,000 g for 10 minutes to obtain the serum, and the samples were then stored in aliquots at −80 °C until measurement. There were no missing data for the most interesting variable, i.e., NT-proBNP level, while other variables were imputed with the mean value for a very few missing.
GRACE was calculated for all patients on admission using eight variables, including age, systolic blood pressure, heart rate, serum creatinine, Killip class, cardiac arrest, elevated cardiac biomarkers (hs-TnT), and ST deviation. The calculator used is available at (http://www.outcomes-umassmed.org/GRACE/).
Follow-up and outcome assessment
Follow-up began at discharge and lasted 12 months for outcome confirmation. Patients lost to follow-up or those with no MACEs were treated as censored. Telephone interviews were conducted monthly by professional cardiologists, which were supplemented by spontaneous clinical visits. All follow-ups ended in December 2019.
The MACEs were a composite outcome consisting of all-cause death, hospital admission for unstable angina, hospital admission for heart failure, nonfatal recurrent myocardial infarction, and target lesion revascularization (TLR). Heart failure was diagnosed according to the current guidelines (12) from the European Society of Cardiology. The diagnosis of recurrent myocardial infarction was defined by the “fourth universal definition of myocardial infarction”. TLR was defined as clinically driven coronary revascularization due to restenosis.
Statistical analysis
There were no particular considerations for power and sample size calculation as we collected patients as much as possible. X-tile analysis, developed for biomarker cut-point selection in a survival scenario by Robert L. Camp, was performed to categorize the serum concentration of NT-proBNP into three levels: low, medium, and high. X-tile analysis was performed to select the cut-off point using both NT-proBNP level and survival status of patients so that survival homogeneity (within a group) and heterogeneity (between groups) can be achieved as much as possible (13). Descriptive statistics for continuous variables were denoted as mean ± SD or M (Q1, Q3), as appropriate according to its distribution. Counts and percentages were used for categorical variables. For group comparison, one-way ANOVA, the Kruskal-Wallis test, or Wald Chi-square test was selected as appropriate (Table 1). Kaplan-Meier curves were used to display patients’ survival, and the log-rank test was used to examine differences. To reveal the effect of NT-proBNP on diverse MACEs, univariate and multivariable Cox proportional hazard models were used for adjusted potential confounders. An exploratory post-hoc subgroup was recommended by expertise, i.e., age ≤60 vs. age >60 years; male vs. female; low/medium vs. high GRACE risk; medicine treatment vs. PCI vs. CABG surgery; vessel completely occluded or not; and LVEF ≤40% vs. LVEF >40%.

Full table
To explore the additional prognostic value of NT-proBNP on GRACE, we first calculated the Pearson correlation coefficient between NT-proBNP (log scale) and GRACE. The Harrell C-index (known as area under the ROC curve) was subsequently calculated to quantify the discrimination ability of NT-proBNP only, GRACE only, or both (14). The net reclassification improvement (NRI) and integrated discrimination improvement (IDI) were also used to evaluate the clinical value of adding NT-proBNP to GRACE. IDI is a more sensitive metric because it is free of arbitrary boundaries delineating discrete risk categories (15-17).
Analyses were performed using SAS software (version 9.4, SAS Institute, Cary, NC) and R software (version 3.6.2). X-tile analysis was performed using X-tile software (version 3.6.1, Copyright Yale University). A two-sided P<0.05 was considered statistically significant.
Results
Clinical characteristics and NT-proBNP
As shown in Table 1, the baseline characteristics profile the enrolled NSTEMI patients. The details are grouped by NT-proBNP level: low-level (5–1,632 pmol/L), medium-level (1,638–5,847 pmol/L), and high-level (5,847–35,000 pmol/L), as shown in Figure S1. The distribution of NT-proBNP level and survival (composite MACEs) of these three groups discretized by X-tile analysis were shown in Figures S2,S3, respectively. The patients’ average age was 64.7±11.5 years old, and those in the high NT-proBNP level were significantly older. Approximately 69.64% of patients were male, although this proportion decreased in the medium and high NT-proBNP levels. 58.26% of patients were current/former smokers, and 27.04% were drinkers, and patients with low NT-proBNP levels tended to have higher levels of smoking and drinking.
Hyperlipidaemia was the most common complication observed in the present study (approximately 76.82%); the average HDLC and LDLC were 1.02±0.27 and 3.01±0.97 mmol/L, respectively. Correspondingly, the use of statins in our cohort reached 96.54%. Higher NT-proBNP-level patients tended to be negatively correlated with the onset of hyperlipidaemia and LDLC concentration. Inversely, hypertension, diabetes, previous stroke, and MI were more frequent in the higher NT-proBNP level group.
Hypertension was the second most common complication in the present study (approximately 67.58%). Furthermore, the average systolic and diastolic pressure was 133.98±20.91 and 76.74±13.01 mmHg, respectively. Correspondingly, the use of beta-blockers and ACEI/ARBs in our patient cohort was 77.23% and 63.52%, respectively. Roughly one-third of patients (33.90%) were complicated with diabetes; approximately 22.99% had the previous stroke, and 18.24% patients had previous MI. Almost all patients were using DAPT (98.38%) and anticoagulants (98.31%).
At the initial presentation, we calculated the GRACE score using the calculator provided by Fox, KAA, Dabbous (18). GRACE scores were classified into three levels: <109 (30.43%), 109–140 (37.29%), and >140 (32.28%). Approximately 85.19% of patients were classified as Killip class 1. We noted that nearly half (45.91%) of the patients had lesions in three vessels, and this proportion reached 80.30% in the high NT-proBNP level group. Treatment strategies, including medicine treatment, PCI, or CABG, were based on the physician’s advice and the patient’s preferences. More than half (56.74%) patients received PCI surgery, 8.47% chose CABG surgery, and 34.78% opted for medicine treatment.
Follow-up and outcomes
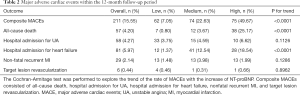
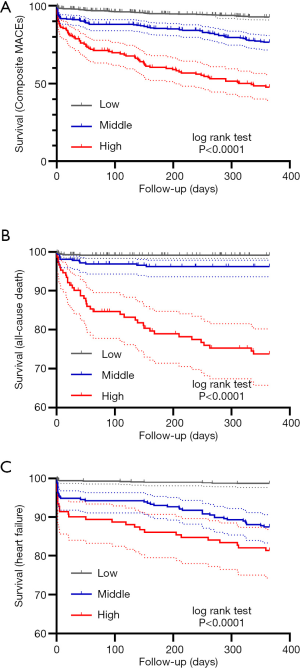
MACEs that occurred within the 12-month follow-up period after discharge are shown in Table 2 and Figure 1. The overall average follow-up was 313 days, and 97 patients were lost to follow-up, with a median follow-up time of 147 days. Also, 1,057 patients were free of any events at the end of follow-up. A total of 211 (15.55%) patients suffered from at least one MACE. Specifically, 57 patients (4.20%) experienced all-cause death, including cardiac and non-cardiac death, 38 of which had a high NT-proBNP level; 58 patients (4.27%) were hospitalized for unstable angina (UA); 81 patients (5.97%) were hospitalized for heart failure. Moreover, 29 patients (2.14%) experienced non-fatal recurrent MI, and six patients (0.44%) experienced target lesion revascularization.
Full table
Also, 19 patients experienced more than once MACE. Of these, five patients experienced heart failure and ultimately died, and another two patients died after recurrent MI. Two patients were hospitalized for heart failure and UA. Four patients experienced recurrent MI and UA. One patient experienced recurrent MI and heart failure. Five patients experienced recurrent MI and were treated with revascularization, one of which subsequently died of a MI attack 2 months later.
Relationship between NT-proBNP and outcomes
The Cochran-Armitage test was performed to assess the trend of the rate of MACEs with the increase of NT-proBNP. As expected, there was a significant uptrend among the low-, medium-, and high NT-proBNP levels (7.05% vs. 22.63% vs. 49.67%, respectively, P<0.0001). Furthermore, all-cause death (0.80% vs. 3.67% vs. 25.17%, respectively, P<0.0001) and hospital admissions for heart failure (1.37% vs. 12.54% vs. 18.54%, respectively, P<0.0001) exhibited a similarly marked uptrend among the three groups. Hospital admission for UA (3.75% vs. 4.59 vs. 6.62%, respectively, P=0.1126) was clinically significant but was not a notable statistical uptrend among three NT-proBNP levels. No linear trend was observed between the rate of nonfatal recurrent MI and target lesion revascularization.
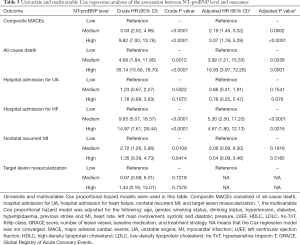
The univariate and multivariable Cox analyses are displayed in Table 3 and Figure 2 (more details are shown in Table S1). The result indicated that a higher NT-proBNP was strongly associated with composite MACEs (medium- vs. low-, adjusted HR 2.19, 95% CI: 1.45–3.32, P=0.0002; high- vs. low-, adjusted HR 3.07, 95% CI: 1.78–5.29, P<0.0001). We also found that higher NT-proBNP was a significant independent risk factor for all-cause death (medium- vs. low-, adjusted HR 3.92, 95% CI: 1.21–15.33, P=0.0258; high- vs. low-, adjusted HR 16.93, 95% CI: 3.97–72.26, P=0.0001) and heart failure (medium- vs. low-, adjusted HR 5.30, 95% CI: 2.50–11.20, P<0.0001; high- vs. low-, adjusted HR 4.67, 95% CI: 1.80–12.13, P=0.0016). No notable statistical association was identified between NT-proBNP level and unstable angina, nonfatal recurrent MI, or target lesion revascularization.
Full table
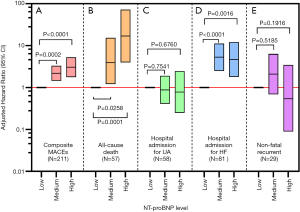
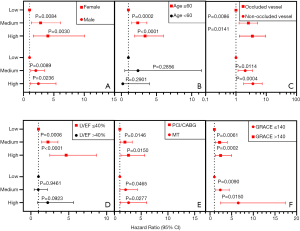
Furthermore, subgroup analysis of NT-proBNP levels on composite MACEs was performed using a Cox model (shown in Figure 3; detailed results are displayed in Table S2). We found that NT-proBNP was a robust prognostic biomarker across different genders, GRACE risk groups, and revascularization strategies, and the prognostic value was more evident for patients older than 60 years and whose LVEF was less than 40%.
Additional prognostic value of NT-proBNP
NT-proBNP (log-scaled for normally distributed data) was positively correlated with the GRACE score (r=0.58 95% CI: 0.54–0.61, P<0.0001). The Harrell C-index of NT-proBNP combined with the GRACE score was higher than those of NT-proBNP or GRACE alone to predict composite MACEs and all of its components (as shown in Table S3). For composite MACEs, the IDI of NT-proBNP combined with the GRACE score (IDI =0.064, 95% CI: 0.027–0.106, P<0.001) and NT-proBNP alone (IDI =0.048, 95% CI: 0.001–0.102, P=0.047) significantly improved the GRACE score alone, although the NRI was not statistically significant. When predicting all-cause death and heart failure, the IDI of NT-proBNP combined with the GRACE score and NT-proBNP alone were both marginally significant, while the NRI was not significant. Due to limited target lesion revascularization (six cases), the NRI and IDI were unavailable.
Other potential prognostic variables
Although this study’s primary aim was to analyze the impact of NT-proBNP on composite MACEs using multivariable Cox regression, some other meaningful variables were identified (as shown in Table S1). Higher LVEF was found to be a protective factor (HR 0.98, 95% CI: 0.96–0.99, P=0.0280). Higher hs-TnT (HR 1.16, 95% CI: 1.06–1.26, P=0.0011) and high GRACE risk (HR 3.43, 95% CI: 1.66–7.07, P=0.0008) were determined to be independent risk factors. Moreover, patients with single occluded vessels had a poor prognosis (HR 1.69, 95% CI: 1.16–2.45, P=0.0059). Patients with NSTEMI could significantly benefit from PCI surgery (HR 0.42, 95% CI: 0.25–0.69, P=0.0006) compared with conservative medicine treatment. Baseline medication including beta-blockers (HR 0.17, 95% CI: 0.10–0.28, P<0.0001), ACEI/ARBs (HR 0.68, 95% CI: 0.49–0.94, P=0.0186), and anticoagulants (HR 0.17, 95% CI: 0.06–0.52, P=0.0018) were found to be protective factors against composite MACEs.
Discussion
This prospective, multicenter cohort study aimed to explore the prognostic value of NT-proBNP in patients with NSTEMI. The key findings were as follows. Firstly, the rate of composite MACEs shows a significant uptrend with increasing levels of NT-proBNP, as does the rate of all-cause death and heart failure. Secondly, higher NT-proBNP levels were identified as an independent risk factor for composite MACEs within 12 months in patients with NSTEMI. Subgroup analysis suggested that NT-proBNP was a robust prognostic biomarker across different genders, GRACE risk groups, and revascularization strategies. However, the prognostic value was more evident for patients older than 60 years and those whose LVEF was less than 40%. High NT-proBNP levels were also found to be an independent risk biomarker for all-cause death and heart failure. Thirdly, predicting composite MACEs, all-cause death, and heart failure were substantially improved when NT-proBNP was combined with the GRACE score. However, there was no significant improvement for predicting hospital admission for UA, nonfatal recurrent MI, and target lesion revascularization.
NT-proBNP is synthesized and secreted by cardiomyocytes to increase blood pressure in the left ventricle, which consequently brings about ventricular dysfunction. When the pressure of the left ventricle overloads in patients with acute coronary syndrome or recurrent ischemic episodes in stable ischemic heart disease, the level of NT-proBNP in peripheral circulation increases. A previous study (19) reported that high NT-proBNP level at initial admission could identify patients with a high risk of progression to MACEs following the onset of NSTEMI, which was consistent with our findings in Chinese patients.
In a real-world clinical scenario, exertional dyspnea and chest pain were common reasons for NSTEMI patients’ presentation, and revascularization procedure selection was based on the severity of NSTEMI and patient preferences. In our cohort, there were 770 (56.74%) patients who received PCI surgery, 115 (8.47%) who received CABG surgery, and 472 (34.78%) who received medicine treatment. A study from Korea revealed that the NT-proBNP level predicted the incidence of MACEs within 12 months in patients with NSTEMI who underwent early invasive PCI (20), which is consistent with our findings. We also found that patients with medium/high levels of NT-proBNP who receive conservative medicine treatment were at a high risk of composite MACEs.
Although the subgroup analyses performed in this study were explorative, the results raise some important points. Our results showed that higher NT-proBNP was correlated with composite MACEs, especially in older patients (HR 3.37, 95% CI: 1.90–5.98). Huang et al. revealed that NT-proBNP levels (log scale) were independently associated with mortality in each age group (61–71 group: HR =1.82; ≥72 groups: HR 1.48) (21). Furthermore, a meta-analysis showed that patients with totally occluded vessels were at a higher risk of mortality and MACEs. Consequently, more precise risk stratification tools are needed to facilitate earlier revascularization to potentially improve outcomes (22). Our finding that NT-proBNP was a prognostic factor for patients with completely occluded vessels may be illuminating. A similar study demonstrated that NT-proBNP was a potential biomarker for risk stratification of ACS patients with the three-vessel disease (23). A lower LVEF suggests an impaired left ventricular function and is correlated with worse outcomes (HR =0.98, 95% CI: 0.96–0.99). We found that NT-proBNP was an independent prognostic factor for patients with LVEF ≤40%, but not for those with LVEF >40%, indicating that early measurement of NT-proBNP may be valuable for patients with impaired left ventricular function.
The GRACE score is a clinical risk prediction tool for estimating the cumulative 6-month risk of death and death or myocardial infarction for both STEMI and NSTMEI patients. Although the GRACE score is widely used to facilitate the triage and management of patients with the acute coronary syndrome, its accuracy needs to be improved (18). There was a moderate positive correlation between NT-proBNP and the GRACE score (r=0.58, P<0.0001). The Harrell C-index of GRACE alone for predicting composite MACEs was 0.7149 and reached 0.7715 when combined with NT-proBNP level. The IDI of NT-proBNP was 0.064, P<0.001, that is, 6.4% increased (decreased) predicted probability for patients with MACEs (without MACEs) was obtained by adding NT-proBNP. The NRI of NT-proBNP was 0.059, P=0.252, which is equivalent to the difference between the proportion of MACE patients in whom the risk scores were determined using the “new model” (GRACE score combined with NT-proBNP) were higher than the risk scores determined using the “old model” (GRACE score alone), minus the same proportion among non-MACE patients.
Interestingly, we observed a near Harrell C-index of GRACE and NT-proBNP (0.7194 vs. 0.7223) with an IDI of 0.048 (P=0.047). Evidence of the additional prognostic value of NT-proBNP was also reported in patients with three-vessel disease. Thus, we concluded that there was a moderate additional value of NT-proBNP. In particular, the NT-proBNP can serve as an approximate surrogate when it is inconvenient or impossible to obtain the GRACE score. NT-proBNP is an independent prognostic biomarker for NSTEMI, but for a synergistic prognostic effect, the GRACE score should be combined at the same time when facilitating triage and management of patients (Table S3).
Considering that MACEs were a composite outcome, further analysis revealed that NT-proBNP was a noteworthy prognostic factor for the occurrence of all-cause death and heart failure, but not for hospital admission for UA, nonfatal recurrent MI, or target lesion revascularization. A previous study has shown that the baseline NT-proBNP level was a strong independent predictor of in-hospital and 180-day mortality (8). Hospital admission for heart failure was the most common outcome in the present study (approximately 5.97%). Compared with STEMI, the triggers of heart failure development following NSTEMI have been poorly studied. It has been reported that NT-proBNP was an independent predictor of heart failure development after NSTEMI (24). Hospital admission for UA, nonfatal recurrent MI, and target lesion revascularization were included in the composite MACEs as they were common clinical practice outcomes. However, they exhibited were no positive relationship with the level of NT-proBNP. A potential reason for this may be that these patients were less severe than heart failure or death and relatively low power of the study.
Limitations
This study had some limitations that should be noted. Firstly, the rates of MACEs were relatively low. As a result, the HRs, NRI, and IDI of NT-proBNP on target lesion revascularization failed to be included in the multivariable Cox regression analysis due to the low power. Thus, subgroup analyses were not performed on each specific outcome (only composite MACEs were analyzed). Although hospital admission for unstable angina was captured, in practice, some patients might bear the pain, and no admission, hence the rate of unstable angina is some what underestimated, despite double-checking by the interviewers.
Moreover, the dosages of medications used during the follow-up period were unavailable. However, in our clinical experience, the medicines used were stable relative to baseline medications, so we inferred no substantial bias in the results. Lastly, considering that the patients in our study were all from China, caution should be applied before generalizing the results to other races.
Conclusions
The present study demonstrated that NT-proBNP is a relatively robust prognostic biomarker following admission with NSTEMI in the Chinese population. Patients with high NT-proBNP levels should be extra vigilant, especially older patients and those with impaired cardiac ejection function. Combining NT-proBNP levels with the GRACE score produced significant incremental benefits in prognostic accuracy for composite MACEs at 12 months, as well as for all-cause death and heart failure. We recommend more accurate risk stratification using NT-proBNP for patients with NSTEMI, which would help subsequent patient management.
Acknowledgments
We would like to thank A. Kassem and J. Chapnick (AME Editing Service) for their help in polishing the language of our paper.
Funding: This research project was funded, in part, by the Key Project of Scientific and Technological Support Plan of Tianjin in 2020 (No. 20YFZCSY00820); Major Science and Technology Projects of Tianjin Science and Technology Commission in 2016 (No. 16ZXMJSY00150); National 135 Key Research and Development Program in 2016 (No.2016YFC1301203).
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at http://dx.doi.org/10.21037/apm-20-2538
Data Sharing Statement: Available at http://dx.doi.org/10.21037/apm-20-2538
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/apm-20-2538). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted following the Declaration of Helsinki (as revised in 2013). This study was approved by the ethics board of Tianjin Chest Hospital (No. 2018KY-010-01), and informed consent was obtained from all individual participants.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Amsterdam EA, Wenger NK, Brindis RG, et al. 2014 AHA/ACC Guideline for the Management of Patients with Non-ST-Elevation Acute Coronary Syndromes: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol 2014;64:e139-228. [Crossref] [PubMed]
- Puymirat E, Simon T, Cayla G, et al. Acute Myocardial Infarction: Changes in Patient Characteristics, Management, and 6-Month Outcomes Over a Period of 20 Years in the FAST-MI Program (French Registry of Acute ST-Elevation or Non-ST-elevation Myocardial Infarction) 1995 to 2015. Circulation 2017;136:1908-19. [Crossref] [PubMed]
- Chan MY, Sun JL, Newby LK, et al. Long-term mortality of patients undergoing cardiac catheterization for ST-elevation and non-ST-elevation myocardial infarction. Circulation 2009;119:3110-7. [Crossref] [PubMed]
- Zhang Q, Zhao D, Xie W, et al. Recent Trends in Hospitalization for Acute Myocardial Infarction in Beijing. Medicine 2016;95:e2677 [Crossref] [PubMed]
- de Lemos JA, McGuire DK, Drazner MH. B-type natriuretic peptide in cardiovascular disease. Lancet 2003;362:316-22. [Crossref] [PubMed]
- Emdin M, Passino C, Prontera C, et al. Comparison of Brain Natriuretic Peptide (BNP) and Amino-Terminal ProBNP for Early Diagnosis of Heart Failure. Clin Chem 2007;53:1289-97. [Crossref] [PubMed]
- Schellings DA, Adiyaman A, Dambrink JE, et al. Predictive value of NT-proBNP for 30-day mortality in patients with non-ST-elevation acute coronary syndromes: a comparison with the GRACE and TIMI risk scores. Vasc Health Risk Manag 2016;12:471-6. [Crossref] [PubMed]
- Bazzino O, Fuselli JJ, Botto F, et al. Relative value of N-terminal probrain natriuretic peptide, TIMI risk score, ACC/AHA prognostic classification and other risk markers in patients with non-ST-elevation acute coronary syndromes. Eur Heart J 2004;25:859-66. [Crossref] [PubMed]
- Scirica BM, Kadakia MB, de Lemos JA, et al. Association between Natriuretic Peptides and Mortality among Patients Admitted with Myocardial Infarction: A Report from the ACTION Registry®–GWTG™. Clin Chem 2013;59:1205-14. [Crossref] [PubMed]
- Roffi M, Patrono C, Collet JP, et al. 2015 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation: Task Force for the Management of Acute Coronary Syndromes in Patients Presenting without Persistent ST-Segment Elevation of the European Society of Cardiology (ESC). Eur Heart J 2016;37:267-315. [Crossref] [PubMed]
- Collinson PO, Barnes SC, Gaze DC, et al. Analytical performance of the N terminal pro B type natriuretic peptide (NT-proBNP) assay on the Elecsys 1010 and 2010 analysers. Eur J Heart Fail 2004;6:365-8. [Crossref] [PubMed]
- Ponikowski P, Voors AA, Anker SD, et al. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: The Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC)Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur Heart J 2016;37:2129-200. [Crossref] [PubMed]
- Camp RL, Dolled-Filhart M, Rimm DL. X-tile: a new bio-informatics tool for biomarker assessment and outcome-based cut-point optimization. Clin Cancer Res 2004;10:7252-9. [Crossref] [PubMed]
- Kang L, Chen W, Petrick NA, et al. Comparing two correlated C indices with right-censored survival outcome: a one-shot nonparametric approach. Stat Med 2015;34:685-703. [Crossref] [PubMed]
- Kerr KF, McClelland RL, Brown ER, et al. Evaluating the incremental value of new biomarkers with integrated discrimination improvement. Am J Epidemiol 2011;174:364-74. [Crossref] [PubMed]
- Pencina MJ, D’Agostino RB Sr, Steyerberg EW. Extensions of net reclassification improvement calculations to measure usefulness of new biomarkers. Stat Med 2011;30:11-21. [Crossref] [PubMed]
- Uno H, Tian L, Cai T, et al. A unified inference procedure for a class of measures to assess improvement in risk prediction systems with survival data. Stat Med 2013;32:2430-42. [Crossref] [PubMed]
- Fox KA, Dabbous OH, Goldberg RJ, et al. Prediction of risk of death and myocardial infarction in the six months after presentation with acute coronary syndrome: prospective multinational observational study (GRACE). BMJ 2006;333:1091. [Crossref] [PubMed]
- Piotrowski G, Gawor R, Banach M, et al. High sensitivity C-reactive protein, NT-proBNP and hemodynamic left ventricular function in acute coronary syndrome without ST segment elevation - a preliminary report. Med Sci Monit 2010;16:CR313-7. [PubMed]
- Shon HS, Bae JW, Kim KO, et al. Biomarker for the Prediction of Major Adverse Cardiac Events in Patients with Non-ST-Segment Elevation Myocardial Infarction. Osong Public Health Res Perspect 2017;8:237-46. [Crossref] [PubMed]
- Huang FY, Huang BT, Tsauo JY, et al. The influence of age on the clinical implications of N-terminal pro-B-type natriuretic peptide in acute coronary syndrome. Intern Emerg Med 2016;11:1077-86. [Crossref] [PubMed]
- Khan AR, Golwala H, Tripathi A, et al. Impact of total occlusion of culprit artery in acute non-ST elevation myocardial infarction: a systematic review and meta-analysis. Eur Heart J 2017;38:3082-9. [Crossref] [PubMed]
- Zhang C, Jiang L, Xu L, et al. Implications of N-terminal pro-B-type natriuretic peptide in patients with three-vessel disease. Eur Heart J 2019;40:3397-405. [Crossref] [PubMed]
- Aronson D, Khatib R, Kapeliovich M, et al. C-Reactive protein on admission is an independent predictor of late development of heart failure in survivors of myocardial infarction. A prospective study. Available online: https://onlinelibrary.wiley.com/doi/pdf/10.1016/S1567-4215%2805%2980005-0


