The diseases of airway-tracheal diverticulum: a review of the literature
Introduction
Paratracheal air cysts (PTACs) encompass various pathological entities, including tracheocele, tracheal diverticula, lymphoepithelial cysts, and bronchogenic cysts. The reported prevalence of PTACs ranges from 0.75–8.1% (1-3). Tracheal diverticulum (DV) consists of small air collections at the paratracheal area lined by ciliated columnar epithelium. Tracheal DV is commonly asymptomatic and incidentally detected by imaging methods. The incidence of tracheal DV is 2.4% (4). Tracheal diverticula are usually located at the right posterolateral region of the trachea (97.1%) and rarely located at the left side (2.9%) (4). Tracheal DV are divided into two subgroups: congenital and acquired. Congenital tracheal DV is seen more commonly in males than in females. Its diameter is smaller and its connection to the trachea is narrow. It is located 4–5 cm below the vocal cords or just above the carina (5). Congenital tracheal DV occurs due to developmental defects in the tracheal cartilage. Acquired tracheal DV may arise at any level and is typically wide-mouthed and larger in size than congenital DV. They occur due to long standing increased intraluminal pressure caused by chronic cough or chronic obstructive pulmonary disease (COPD) combined with a weakened tracheal wall (6).
Review
Epidemiology
Tracheal DV is a benign condition characterized by one or multiple invaginations of the tracheal wall (7). It is usually located in the right posterolateral region of the trachea at the level between the T1 and T3 vertebrae. The mean tracheal DV size is 4 mm (ranging from 2–6 mm) (4). The wall of the tracheal DV can be thin or thick. Kurt et al. revealed that the mean age of patients with tracheal diverticulum was 58 years (range, 16–93 years) (4). Polat et al. (8) reported that the mean age of the patients with paratracheal air cysts was 55±16.6. They also reported no significant difference between the presence of PTACs and age. Kurt et al. (4) reported that tracheal DV is more common in men (64%) than in women (36%). However, Cheng et al. (9) and Buterbaugh et al. (2) reported that PTACs were found to be significantly more common in women than in men. There are several different studies in the literature evaluating the relationship between tracheal DV and airway or parenchymal lung pathologies. Goo et al. (1) demonstrated that tracheal DV and bronchial DV may be accompanied by COPD (emphysema, chronic bronchitis, and/or bronchiectasis). A study by Buterbaugh and Erly (2) found no association between the presence of emphysematous lung changes and PTACs. In addition, Kurt et al. (4) showed no significant association between tracheal DV and COPD. Polat et al. (8) demonstrated a statistically significant relationship between COPD and PACs. However, there was no relationship between primary or metastatic malignancies, pneumonia, and other pulmonary diseases and PTACs. Kurt et al. found that 84 out of 412 tracheal DV patients had a bronchial DV, and 72 out of those 84 tracheal diverticula cases were associated with COPD. They also demonstrated a significant correlation between COPD and bronchial DV (P<0.05).
Classification
Congenital tracheal DV is located 4–5 cm below the vocal cords or just above the carina; it is often located in the right paratracheal area (5). Also, it is smaller that of acquired DV, and it communicates with a small tract to the tracheal lumen. Congenital tracheal DV arises from a defect in endodermal differentiation during development of the membranous posterior tracheal wall or from a defect in the development of the tracheal cartilage during the sixth week of fetal life (10). Congenital tracheal DV affects the entire anatomy (respiratory epithelium, smooth muscle, and cartilage) of the trachea, and it is often filled with mucus. It is rarely associated with other congenital malformations, such as tracheoesophageal fistula (11).
Acquired tracheal DV can occur at any level, and it only includes respiratory epithelium. It does not affect the smooth muscle or the cartilage (1). It is frequently located in the posterolateral area at the level of the thoracic inlet between the extrathoracic and intrathoracic area. It is also commonly located in the posterolateral area between the extrathoracic and intrathoracic trachea at the entrance to the thorax, and it is larger than congenital tracheal diverticulum. Acquired tracheal DV can occur as a complication of surgical procedures or as a result of tracheomalacia. In addition, an increase of the tracheal intraluminal pressure caused by chronic cough or obstructive lung disease with emphysema combined with a weakened musculature of the trachea wall due to repeated respiratory infections can lead to the acquired form of tracheal DV (5). Acquired tracheal DV can be single or multiple. Multiple acquired tracheal DV is the hallmark of tracheobronchomegaly or Mounier-Kuhn disease (11,12).
Clinical presentation
Acquired and congenital DVs are often asymptomatic. Chronic cough, dyspnea, stridor, or recurrent tracheobronchitis may be seen in symptomatic patients (6). Dysphagia, odynophagia, neck pain, hoarseness, hemoptysis, choking, recurrent episodes of hiccups, and/or burping may also seen (6,13). Tracheal DV can also cause dysphonia due to recurrent paralysis resulting from direct compression of the DV. Infected tracheal DV may lead to paratracheal abscess (5,13). Tracheal intubation can be difficult in patients with tracheal diverticula. There was a case report of pneumomediastinum as a result of perforation of a tracheal diverticulum caused by tracheal intubation in the literature (14).
Diagnosis
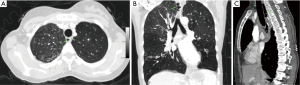
Multidetector computed tomography (MDCT) is the best imaging method to demonstrate tracheal DV. It is useful for evaluating the localization, size, contour, and wall thickness of tracheal DV. Communication between the DV and trachea can also be seen with MDCT. Characteristic MDCT findings of tracheal DV include a thin-walled air sac at the paratracheal area with or without communication to the tracheal lumen (7). MDCT also can be use to distinguish between congenital and acquired lesions, depending on the presence or absence of cartilage and the size of the neck of the DV (5). Slice thicknes of the chest MDCT should be thinner than 1 mm for detailed, accurate evaluation of tracheal DV. Axial, coronal, and sagittal multiplanar images can be obtained with thinner (≤1 mm) slice thicknesses (Figure 1). Connection between DV and the trachea can be evaluated easily with these multiplanar images (Figure 2).
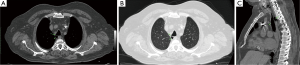
Kurt et al. (4) demonstrated communication between the tracheal lumen and diverticula in 53 (12.9%) of the 412 tracheal diverticulum cases. In addition, Polat et al. (8) demonstrated communication between the tracheal lumen and air cysts in 50 (16.6%) of the 301 PTACs.
Bronchoscopy can be used for diagnosis of tracheal DV; however, this is an invasive procedure. In addition, tracheal DV with a very narrow opening or those joined to the trachea by only a fibrous tract may not be revealed by bronchoscopy (5). The finding of a collection of paratracheal air necessitates first determining whether its origin is tracheal or from another nearby structure. Differential diagnosis of PTACs include laryngocele, pharyngocele, Zenker’s DV, apical hernia, and lung bullae (5). Pharyngocele and Zenker’s DV can be differentiated from tracheal DV by barium studies or thorax MDCT. In addition, apical hernia and apical bullae can be distinguish from tracheal DV by thorax MDCT (15).
Tracheal DV can become infected due to recurrent upper respiratory tract infections, and infected tracheal DV can progress into a paratracheal abscess. Infected tracheal DV can be viewed as a paratracheal mediastinal mass with a fluid-containing cyst that usually enhances following the intravascular administration of contrast materials in thorax MDCT. Infection may also progress into empyema or subphrenic abscess (13). Infected paratracheal diverticula cannot not be easily distinguished from infected Zenker’s DV. If the connection between the tracheal lumen and the DV is not visualized in thorax MDCT or bronchoscopy, upper gastrointestinal system endoscopy should be performed. If previous studies are available, radiographic records can be compared (13).
Treatment
Treatment is not necessary in asymptomatic patients (9). The age of the patient, the clinical presentation, and the presence of comorbidities should be taken into account when choosing a treatment approach in symptomatic patients (16). Surgical resection is often the treatment of choice for young, symptomatic patients (9). Surgical resection can be performed with the lateral cervical approach without the need for thoracotomy. In addition, endoscopic cauterization with laser or electrocoagulation can be used to treat symptomatic patients (5). However, conservative treatment can be performed in older patients. Conservative management (antibiotics, mucolytic agents, and physiotherapy) may also be applied for these patients.
Patients with acquired tracheal DV cannot always benefit from surgical resection. Prevention of the infection of diverticulum is the optimum choice in patients with multiple and wide-based acquired tracheal DV (7). Surgical resection is needed for congenital tracheal DV due to the long-term accumulated mucous in the lesion, which could be a source of infection. Surgical resection should be performed carefully in these patients due to the risk of injury of the laryngeal nerve and the esophagus (7).
Emergency intubation and surgical drainage is indicated in patients with paratracheal abscess who present with respiratory distress (13).
Conclusions
Tracheal DV is a type of PTAC that is usually discovered incidentally on thorax MDCT. The connection between the trachea and DV is not always shown by imaging methods and bronchoscopy. There are two different types of tracheal DV: congenital and acquired. The differential diagnosis of congenital and acquired tracheal DV is important for treatment. Surgical resection is needed for congenital tracheal DV due to the long-term accumulated mucous in the lesion, which could be a source of infection.
Acknowledgements
None.
Footnote
Conflicts of Interest: A Tanrivermis Sayit is the guarantor. The other authors have no conflicts of interest to declare.
References
- Goo JM, Im JG, Ahn JM, et al. Right paratracheal air cysts in the thoracic inlet: clinical and radiologic significance. AJR Am J Roentgenol 1999;173:65-70. [Crossref] [PubMed]
- Buterbaugh JE, Erly WK. Paratracheal air cysts: a common finding on routine CT examinations of the cervical spine and neck that may mimic pneumomediastinum in patients with traumatic injuries. AJNR Am J Neuroradiol 2008;29:1218-21. [Crossref] [PubMed]
- Bae HJ, Kang EY, Yong HS, et al. Paratracheal air cysts on thoracic multidetector CT: incidence, morphological characteristics and relevance to pulmonary emphysema. Br J Radiol 2013;86:20120218. [Crossref] [PubMed]
- Kurt A, Sayit AT, Ipek A, et al. A multi detector computed tomography survey of tracheal diverticulum. Eurasian J Med 2013;45:145-8. [Crossref] [PubMed]
- Soto-Hurtado EJ, Peñuela-Ruíz L, Rivera-Sánchez I, et al. Tracheal diverticulum: a review of the literature. Lung 2006;184:303-7. [Crossref] [PubMed]
- Srivastava A, Guitron J, Williams VA. Tracheal diverticulum: an atypical presentation. J Thorac Cardiovasc Surg 2014;148:3244-5. [Crossref] [PubMed]
- Lin H, Cao Z, Ye Q. Tracheal diverticulum: a case report and literature review. Am J Otolaryngol 2014;35:542-5. [Crossref] [PubMed]
- Polat AV, Elmali M, Aydin R, et al. Paratracheal air cysts: prevalence and correlation with lung diseases using multi-detector CT. J Med Imaging Radiat Oncol 2014;58:144-8. [Crossref] [PubMed]
- Cheng HM, Chang PY, Chiang KH, et al. Prevalence and characteristics of paratracheal air cysts and their association with emphysema in a general population. Eur J Radiol 2012;81:2673-7. [Crossref] [PubMed]
- Tanaka H, Mori Y, Kurokawa K, et al. Paratracheal air cysts communicating with the trachea: CT findings. J Thorac Imaging 1997;12:38-40. [Crossref] [PubMed]
- Bhatnagar V, Lal R, Agarwala S, et al. Endoscopic treatment of tracheal diverticulum after primary repair of esophageal atresia and tracheoesophageal fistula. J Pediatr Surg 1998;33:1323-4. [Crossref] [PubMed]
- Lazzarini-de-Oliveira LC, Costa de Barros Franco CA, Gomes de Salles CL, et al. A 38-year-old man with tracheomegaly, tracheal diverticulosis, and bronchiectasis. Chest 2001;120:1018-20. [Crossref] [PubMed]
- Akabane S, Kawachi J, Fukai R, et al. A rare case of an infected tracheal diverticulum requiring emergency intervention: A case report. Int J Surg Case Rep 2016;24:7-9. [Crossref] [PubMed]
- Möller GM, ten Berge EJ, Stassen CM. Tracheocele: a rare cause of difficult endotracheal intubation and subsequent pneumomediastinum. Eur Respir J 1994;7:1376-7. [PubMed]
- Dabbs DJ, Duhaylongsod F, Schour L. Fine needle aspiration cytology of congenital tracheal diverticulum. A case report. Acta Cytol 1994;38:98-100. [PubMed]
- Amaral CB, Silva S, Feijó S. Infected tracheal diverticulum: a rare association with alpha-1 antitrypsin deficiency. J Bras Pneumol 2014;40:669-72. [Crossref] [PubMed]


