Higher serum lipids and oxidative stress in patients with normal tension glaucoma, but not pseudoexfoliative glaucoma
DOI:
https://doi.org/10.17305/bjbms.2016.830Keywords:
Oxidative Stress, Paraoxonase, High-Density Lipoprotein, Hyperlipidemia, Normal Tension Glaucoma, Pseudoexfoliative Glaucoma, PON1 PhenotypeAbstract
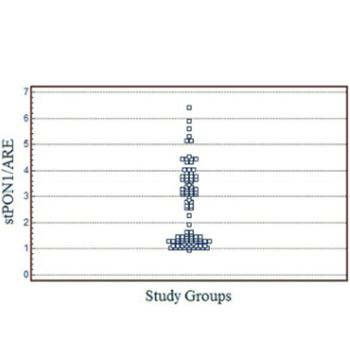
This study entailed a cross-examination of oxidant/antioxidant balance, high-density lipoprotein (HDL)-linked paraoxonase 1 (PON1) phenotypes, and levels of serum routine lipids among patients with normal tension glaucoma (NTG) or pseudoexfoliative glaucoma (PEXG) compared with healthy control groups. We aimed to investigate the links between oxidative stress (OS), HDL-related antioxidant enzyme activities and dyslipidemia in distinct subtypes of glaucoma. The study included 32 patients with NTG, 31 patients with PEXG, and 40 control subjects. Levels of PON1 and arylesterase enzymatic activity, total oxidant status (TOS), and total antioxidant status were measured by spectrophotometry and OS indexes (OSI) were calculated. The phenotype distribution of PON1 was determined using the dual substrate method. Blood serum levels of HDL, low-density lipoprotein, total cholesterol (TC), and triglyceride (TG) were measured. The TOS and OSI values in the NTG group were significantly higher compared with the other groups (both p < 0.01). The phenotype distribution found in the glaucoma and control groups were NTG: QQ, 59.4%; QR, 37.5%; RR, 3.1%; PEXG: QQ, 45.1%; QR, 48.4%; RR, 6.5%; and in the control group: QQ, 42.5%; QR, 50.0%; RR, 7.5%. Serum TC levels were significantly higher than the control in both NTG and PEXG groups, whereas TG was significantly higher in NTG only (p < 0.01 and p < 0.02, respectively). Hyperlipidemia, OS and variations in phenotype distribution of PON1 may play a role in the pathogenesis of different types of glaucoma.
Downloads
References
Casson RJ, Chidlow G, Wood JP, Crowston JG, Goldberg I. Definition of glaucoma: Clinical and experimental concepts. Clin Experiment Ophthalmol 2012;40(4):341-9. http://dx.doi.org/10.1111/j.1442-9071.2012.02773.x.
Weinreb RN, Aung T, Medeiros FA. The pathophysiology and treatment of glaucoma: A review. JAMA 2014;311(18):1901-11. http://dx.doi.org/10.1001/jama.2014.3192.
Saccà SC, Centofanti M, Izzotti A. New proteins as vascular biomarkers in primary open angle glaucomatous aqueous humor. Invest Ophthalmol Vis Sci 2012;53(7):4242-53. http://dx.doi.org/10.1167/iovs.11-8902.
Saccà SC, Pulliero A, Izzotti A. The dysfunction of the trabecular meshwork during glaucoma course. J Cell Physiol 2015;230(3):510-25. http://dx.doi.org/10.1002/jcp.24826.
Mi XS, Yuan TF, So KF. The current research status of normal tension glaucoma. Clin Interv Aging 2014;9:1563-71.
Pinazo-Durán MD, Gallego-Pinazo R, García-Medina JJ, Zanón-Moreno V, Nucci C, Dolz-Marco R, et al. Oxidative stress and its downstream signaling in aging eyes. Clin Interv Aging 2014;9:637-52. http://dx.doi.org/10.2147/CIA.S52662.
Nitta E, Hirooka K, Tenkumo K, Fujita T, Nishiyama A, Nakamura T, et al. Aldosterone: A mediator of retinal ganglion cell death and the potential role in the pathogenesis in normal-tension glaucoma. Cell Death Dis 2013;4:e711. http://dx.doi.org/10.1038/cddis.2013.240.
Schlötzer-Schrehardt U, Naumann GO. Ocular and systemic pseudo exfoliation syndrome. Am J Ophthalmol 2006;141(5):921-37. http://dx.doi.org/10.1016/j.ajo.2006.01.047.
Gartaganis SP, Patsoukis NE, Nikolopoulos DK, Georgiou CD. Evidence for oxidative stress in lens epithelial cells in pseudoexfoliation syndrome. Eye (Lond) 2007;21(11):1406-11. http://dx.doi.org/10.1038/sj.eye.6702596.
Koliakos GG, Befani CD, Mikropoulos D, Ziakas NG, Konstas AG. Pro-oxidant-antioxidant balance, peroxide and catalase activity in the aqueous humour and serum of patients with exfoliation syndrome or exfoliative glaucoma. Graefes Arch Clin Exp Ophthalmol 2008;246(10):1477-83. http://dx.doi.org/10.1007/s00417-008-0871-y.
Borazan M, Karalezli A, Kucukerdonmez C, Bayraktar N, Kulaksizoglu S, Akman A, et al. Aqueous humor and plasma levels of vascular endothelial growth factor and nitric oxide in patients with pseudoexfoliation syndrome and pseudo exfoliation glaucoma. J Glaucoma 2010;19(3):207-11. http://dx.doi.org/10.1097/IJG.0b013e3181aae93e.
Tanito M, Kaidzu S, Takai Y, Ohira A. Status of systemic oxidative stresses in patients with primary open-angle glaucoma and pseudoexfoliation syndrome. PLoS One 2012;7(11):e49680. http://dx.doi.org/10.1371/journal.pone.0049680.
Demirdögen BC, Ceylan OM, Isikoglu S, Mumcuoglu T, Erel O. Evaluation of oxidative stress and paraoxonase phenotypes in pseudoexfoliation syndrome and pseudoexfoliation glaucoma. Clin Lab 2014;60(1):79-86.
Yilmaz N. Relationship between paraoxonase and homocysteine: Crossroads of oxidative diseases. Arch Med Sci 2012;8(1):138-53. http://dx.doi.org/10.5114/aoms.2012.27294.
Mackness M, Mackness B. Human paraoxonase-1 (PON1): Gene structure and expression, promiscuous activities and multiple physiological roles. Gene 2015;567(1):12-21. http://dx.doi.org/10.1016/j.gene.2015.04.088.
Rozenberg O, Shih DM, Aviram M. Paraoxonase 1 (PON1) attenuates macrophage oxidative status: Studies in PON1 transfected cells and in PON1 transgenic mice. Atherosclerosis 2005;181(1):9-18. http://dx.doi.org/10.1016/j.atherosclerosis.2004.12.030.
Guns PJ, Van Assche T, Verreth W, Fransen P, Mackness B, Mackness M, et al. Paraoxonase 1 gene transfer lowers vascular oxidative stress and improves vasomotor function in apolipoprotein E-deficient mice with pre-existing atherosclerosis. Br J Pharmacol 2008;153(3):508-16. http://dx.doi.org/10.1038/sj.bjp.0707585.
Eren E, Ellidag HY, Aydin O, Yilmaz N. HDL functionality and crystal-based sterile inflammation in atherosclerosis. Clin Chim Acta 2015;439:18-23. http://dx.doi.org/10.1016/j.cca.2014.09.024.
Eren E, Yilmaz N, Aydin O, Ellidag HY. Anticipatory role of high density lipoprotein and endothelial dysfunction: An overview. Open Biochem J 2014;8:100-6. http://dx.doi.org/10.2174/1874091X01408010100.
Eren E, Ellidag HY, Aydin O, Yilmaz N. Homocysteine, paraoxonase-1 and vascular endothelial dysfunction: Omnibus viis romam pervenitur. J Clin Diagn Res 2014;8(9):CE01-4. http://dx.doi.org/10.7860/jcdr/2014/7827.4773.
Aviram M, Hardak E, Vaya J, Mahmood S, Milo S, Hoffman A, et al. Human serum paraoxonases (PON1) Q and R selectively decrease lipid peroxides in human coronary and carotid atherosclerotic lesions: PON1 esterase and peroxidase-like activities. Circulation 2000;101(21):2510-7. http://dx.doi.org/10.1161/01.CIR.101.21.2510.
Eckerson HW, Romson J, Wyte C, La Du BN. The human serum paraoxonase polymorphism: Identification of phenotypes by their response to salts. Am J Hum Genet 1983;35(2):214-27.
Richter RJ, Furlong CE. Determination of paraoxonase (PON1) status requires more than genotyping. Pharmacogenetics 1999;9(6):745-53. http://dx.doi.org/10.1097/01213011-199912000-00009, http://dx.doi.org/10.1097/00008571-199912000-00009.
Mackness B, Davies GK, Turkie W, Lee E, Roberts DH, Hill E, et al. Paraoxonase status in coronary heart disease: Are activity and concentration more important than genotype? Arterioscler Thromb Vasc Biol 2001;21(9):1451-7. http://dx.doi.org/10.1161/hq0901.094247.
Eckerson HW, Wyte CM, La Du BN. The human serum paraoxonase/arylesterase polymorphism. Am J Hum Genet 1983;35(6):1126-38.
Haagen L, Brock A. A new automated method for phenotyping arylesterase (EC 3.1.1.2) based upon inhibition of enzymatic hydrolysis of 4-nitrophenyl acetate by phenyl acetate. Eur J Clin Chem Clin Biochem 1992;30(7):391-5. http://dx.doi.org/10.1515/cclm.1992.30.7.391.
Erel O. A new automated colorimetric method for measuring total oxidant status. Clin Biochem 2005;38(12):1103-11. http://dx.doi.org/10.1016/j.clinbiochem.2005.08.008.
Erel O. A novel automated direct measurement method for total antioxidant capacity using a new generation, more stable ABTS radical cation. Clin Biochem 2004;37(4):277-85. http://dx.doi.org/10.1016/j.clinbiochem.2003.11.015.
Kosecik M, Erel O, Sevinc E, Selek S. Increased oxidative stress in children exposed to passive smoking. Int J Cardiol 2005;100(1):61-4. http://dx.doi.org/10.1016/j.ijcard.2004.05.069.
Mackness B, Mackness MI, Arrol S, Turkie W, Durrington PN. Effect of the human serum paraoxonase 55 and 192 genetic polymorphisms on the protection by high density lipoprotein against low density lipoprotein oxidative modification. FEBS Lett 1998;423(1):57-60. http://dx.doi.org/10.1016/S0014-5793(98)00064-7.
Zhou G, Liu B. Single nucleotide polymorphisms of metabolic syndrome-related genes in primary open angle glaucoma. Int J Ophthalmol 2010;3(1):36-42.
Inagaki Y, Mashima Y, Funayama T, Ohtake Y, Fuse N, Yasuda N, et al. Paraoxonase 1 gene polymorphisms influence clinical features of open-angle glaucoma. Graefes Arch Clin Exp Ophthalmol 2006;244(8):984-90. http://dx.doi.org/10.1007/s00417-005-0200-7.
Eren E, Yilmaz N, Aydin O. High density lipoprotein and it's dysfunction. Open Biochem J 2012;6:78-93. http://dx.doi.org/10.2174/1874091X01206010078.
Shah AS, Tan L, Long JL, Davidson WS. Proteomic diversity of high density lipoproteins: Our emerging understanding of its importance in lipid transport and beyond. J Lipid Res 2013;54(10):2575-85. http://dx.doi.org/10.1194/jlr.R035725.
Pavljasevic S, Asceric M. Primary open-angle glaucoma and serum lipids. Bosn J Basic Med Sci 2009;9(1):85-8.
Kim MJ, Kim MJ, Kim HS, Jeoung JW, Park KH. Risk factors for open-angle glaucoma with normal baseline intraocular pressure in a young population: The Korea National Health and Nutrition Examination Survey. Clin Experiment Ophthalmol 2014;42(9):825-32. http://dx.doi.org/10.1111/ceo.12347.
Modrzejewska M, Grzesiak W, Zaborski D, Modrzejewska A. The role of lipid dysregulation and vascular risk factors in glaucomatous retrobulbar circulation. Bosn J Basic Med Sci 2015;15(2):50-6. http://dx.doi.org/10.17305/bjbms.2015.299.
Kim YH, Jung SW, Nam GE, Do Han K, Bok AR, Baek SJ, et al. High intraocular pressure is associated with cardiometabolic risk factors in South Korean men: Korean National Health and Nutrition Examination Survey, 2008-2010. Eye (Lond) 2014;28(6):672-9. http://dx.doi.org/10.1038/eye.2014.43.
Marcus MW, Müskens RP, Ramdas WD, Wolfs RC, De Jong PT, Vingerling JR, et al. Cholesterol-lowering drugs and incident open-angle glaucoma: A population-based cohort study. PLoS One 2012;7(1):e29724. http://dx.doi.org/10.1371/journal.pone.0029724.
Stein JD, Newman-Casey PA, Talwar N, Nan B, Richards JE, Musch DC. The relationship between statin use and open-angle glaucoma. Ophthalmology 2012;119(10):2074-81. http://dx.doi.org/10.1016/j.ophtha.2012.04.029.