Abstract
Objectives
Few are the longitudinal studies on the changes in moderate or severe symptoms of anxiety or depression (MSS-ANXDEP) from before to during the COVID-19 pandemic in Canada. The aim was to study the change in MSS-ANXDEP and associated sociodemographic, economic, psychosocial, health behaviour and lifestyle, and clinical factors.
Methods
The current sample includes 59,997 adults aged ≥ 35 years participating in the 2018 and 2020 health surveys of the 5 established cohorts of the Canadian Partnership for Tomorrow’s Health (CanPath). MSS-ANXDEP was based on a cutoff score ≥ 10 on the 7-item Generalized Anxiety Disorder Scale and Patient Health Questionnaire (PHQ-8). Change in MSS-ANXDEP was categorized as follows: no MSS-ANXDEP, remitted, incident, and persistent. Multinomial regressions were used to study MSS-ANXDEP as a function of sociodemographic, economic, psychosocial, health behaviours and lifestyle, and clinical factors.
Results
Sociodemographic and economic (i.e. age, gender, cohort, race/ethnicity, lower income, decreased in income, work status, being an essential worker), lifestyle and health behaviours (i.e. smoking, cannabis and alcohol use, drinking more alcohol), psychosocial (i.e. provide help to others, information and instrumental support, and change in relationships with friends, family, and partner) and clinical factors (i.e. lifetime mental disorder and multimorbidity) were associated with remitted, incident, and persistent MSS-ANXDEP.
Conclusion
Health and socio-economic factors were associated with changes in symptoms of anxiety and depression during the pandemic, further increasing inequities in mental health needs. Public health campaigns on the importance of healthy behaviours should continue and health policies should reduce economic and social barriers to integrated substance use and mental health care.
Résumé
Objectifs
Les études longitudinales sur l’évolution des symptômes modérés ou sévères d’anxiété ou de dépression (SMS-ANXDEP) avant et pendant la pandémie de COVID-19 au Canada sont rares. L’objectif était d’étudier l’association entre l’évolution des SMS-ANXDEP et les facteurs sociodémographiques, économiques, psychosociaux, cliniques et liés aux comportements et au mode de vie, avant et pendant la pandémie.
Méthodes
Ce grand échantillon comprend 59 997 adultes âgés de ≥ 35 ans qui ont participé aux enquêtes de santé 2018 et 2020 des 5 cohortes établies du Partenariat canadien pour la santé de demain (CanPath). La présence de SMS-ANXDEP a été définie par un résultat ≥ 10 sur les échelles Generalized Anxiety Disorder Scale à 7 items (GAD-7) et Patient Health Questionnaire (PHQ-8). Les changements dans les SMS-ANXDEP ont été catégorisés selon les patrons temporels suivants : absence, rémission, incidence et persistance de SMS-ANXDEP. Des régressions multinomiales multivariées ont été utilisées pour étudier les patrons temporels de SMS-ANXDEP en fonction, des facteurs socio-démographiques, économiques, associés au style de vie et aux comportements de santé, psychosociaux et cliniques.
Résultats
Les facteurs socio-démographiques et économiques (âge, genre, cohorte, race/ethnie, revenu inférieur, diminution du revenu, statut d’emploi, être un travailleur essentiel), associés au style de vie et aux comportements de santé (tabagisme, consommation de cannabis et d’alcool, consommation accrue d’alcool), psychosociaux (offrir de l’aide pendant la pandémie, soutien en information et instrumental, changement dans les relations avec les amis, la famille et la personne partenaire) et cliniques (trouble mental au cours de la vie, multimorbidité) étaient associés à la présence de SMS-ANXDEP en rémission, incident et persistant.
Conclusion
Les patrons temporels des SMS-ANXDEP pendant la pandémie étaient associés aux facteurs socio-économiques et de santé, suggérant des inégalités accrues en matière de besoins de santé mentale. Les campagnes de santé publique sur l’importance d’adopter des comportements sains devraient continuer et les politiques de santé devraient réduire les barrières économiques et sociales aux soins intégrés de santé mentale et de toxicomanie.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Mental health needs increased in the context of the COVID-19 pandemic (World Health Organization, 2022). SARS-CoV-2 infection rates and decreased mobility due to public health physical distancing mandates were associated with major depressive and anxiety disorders (COVID-19 Mental Disorders Collaborators, 2021). Higher prevalence in self-reported anxiety and depression in general population studies during the pandemic as compared to pre-pandemic periods was observed across 49 countries, with meta-regression prevalence differences estimated at 27.6% and 25.6%, respectively (COVID-19 Mental Disorders Collaborators, 2021). Data from a recent Dutch population–based study showed an increase in overall prevalence of mental and substance use disorders between 2010–2012 and 2016–2018, which continued to increase in 2019–2022 (Ten Have et al., 2023). In Canada, in comparison to the month before the pandemic, a cross-sectional survey showed a 12% and 29% increase in reported mild to severe symptoms of generalized anxiety and depression in individuals without a history of mental illness (Robillard et al., 2021). In one of the rare longitudinal studies on pre-post COVID changes amid the same population sampled, the Canadian Longitudinal Study on Aging (CLSA) showed an increase in moderate to severe symptoms of depression from 16.4% during the pre-COVID-19 phase to 22.0% during the first pandemic wave in older adults (Raina et al., 2021).
Studies also reported on the factors associated with anxiety and depression during the COVID-19 pandemic. Gender, racial, and socio-economic inequities related to mental health status were observed (Chen & Wang, 2021; Public Health Agency of Canada, 2021). Descriptive statistics in Canada showed that identifying as a woman, Indigenous, or a healthcare worker, as well as reporting decreased income due to the pandemic, lifetime traumatic events, or chronic conditions, were associated with a higher prevalence of anxiety and depression at the start of the pandemic (Public Health Agency of Canada, 2020; Statistics Canada, 2021). Individuals infected with the SARS-CoV-2 virus (Inchausti et al., 2020) were also more likely to report anxiety and depression.
Social and economic disruptions related to the COVID-19 pandemic posed a risk to marital satisfaction (Carrese-Chacra et al., 2023) and the well-being of families and communities (Prime et al., 2020). A recent study on Dutch older adults aged 55 years and over showed that regardless of pre-pandemic mental health, size of network was associated with symptoms of anxiety during the pandemic (Holwerda et al., 2023). A study during the COVID-19 pandemic focusing on the change in quality of relationships between married adults with children also showed a steeper decline in satisfaction with the relationship in women and in individuals with symptoms of depression (James et al., 2022).
Depression and anxiety disorders are associated with increased functional limitations and decreased quality of life and loss in productivity (Chisholm et al., 2016; COVID-19 Mental Disorders Collaborators, 2021; Hohls et al., 2021). Given that mental health unmet needs increased in the past decade (Ten Have et al., 2023) and in the context of the COVID-19 pandemic (World Health Organization, 2022), it is important to identify individuals at risk for new and persistent symptoms of anxiety and depression as well as the factors associated with the course of depression and anxiety symptoms (i.e., persistence, incidence, remission) to inform on better treatment plans. Scarce are the longitudinal studies that have assessed the factors associated with the course of depression and anxiety in general populations while accounting for income prior to the pandemic and changes in socio-economic, employment, and psychosocial factors and health behaviours during the pandemic, in Canada and elsewhere. Further, although the importance to report sex- and age-specific results has been highlighted (Institute of Medicine (US) Board on Population Health and Public Health Practice, 2012; Dannefer, 2001; Abramson & Portacolone, 2017), studies have not reported age- and sex-specific factors associated with temporal patterns of depression and anxiety disorders, which can inform on the social and structural inequities leading to anxiety and depression.
The current study objectives aimed to fill this gap by assessing the temporal patterns (absence, remission, incidence, persistence) of moderate to severe symptoms of anxiety and depression in adults and older adults from before to during the first two waves of the COVID-19 pandemic across Canada. The COVID-19 pandemic had an impact on the risk of infection and the health of populations, on psychological and behavioural factors, as well as on socio-economic factors. The biopsychosocial model was therefore used as a guiding framework to study the distinct contributions of social determinants of health, psychological factors, and medical and health-related behaviours on the temporal patterns of anxiety and depression. Also identified in a conceptual framework for public mental health (Dykxhoorn et al., 2022), the roles of a range of socio-economic, psychological, and health and lifestyle behaviour correlates associated with the temporal patterns of anxiety and depression will be studied. This can be useful in informing population and public health (Bolton & Gillett, 2019; Frazier, 2020). Therefore, as a second aim, the roles of a range of sociodemographic, economic, employment, psychosocial, health behaviour, and lifestyle factors, as well as clinical factors as correlates, will be studied. Although the pandemic has evolved, recent data show that improvements in mental health have stagnated and are still at much higher levels than pre-pandemic (Mental Health Research Canada, 2023). As the effect of the pandemic on mental health is proving to be persistent, the current study focusing on the first two waves of the pandemic captures an important period where we can identify at-risk individuals whose mental health worsened and assess the factors that may further disadvantage these individuals following pandemic peaks. This period was associated with intense public health and physical distancing restrictions without effective vaccines, potentially contributing to changes in mental health. The equitable distribution of health is a priority for population health and value-based health systems (Teisberg et al., 2020; Smith et al., 2021). This study will aim to characterize at-risk individuals with persistent and onset of new symptoms of anxiety and depression. The findings can inform public health programs to ameliorate mental health in better tailoring healthier lifestyle promotion campaigns. Further, the findings can inform health policies aimed at improving the efficient allocation of resources for equitable access to integrated substance use and mental health care to adequately address population mental health needs.
Methods
Study population and procedures
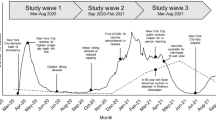
The current study draws on harmonized survey data made available by CanPath—the Canadian Partnership for Tomorrow’s Health (formerly Canadian Partnership for Tomorrow Project, CPTP), and its 5 established regional cohorts, namely the British Columbia Generations Project (BCGP), Alberta’s Tomorrow Project (ATP), Ontario Health Study (OHS), Quebec’s CARTaGENE (CaG), and Atlantic Partnership for Tomorrow’s Health (Atlantic PATH). The recruitment and profile of CanPath participants have been described elsewhere (Dummer et al., 2018). In general, CanPath participants were more likely to be female, report higher income and education, be retired, and self-report as White than the general Canadian population (Dummer et al., 2018). The current study relied on data from 69,143 participants who had responded to both the 2018 CanPath and the COVID-19 follow-up questionnaire (May–December 2020) (https://canpath.ca/en/covid-19-initiatives). The temporal patterns of moderate or severe symptoms of anxiety or depression were assessed at both surveys, while all the other independent study variables were assessed during the pandemic 2020 survey, except for race/ethnicity, which was ascertained in the survey prior to the pandemic. The present study sample includes n = 59,997 (86.8%) participants (22.6% from BCGP, 12.5% from ATP, 40.6% from OHS, 8.9% from CaG, 15.4% from PATH) with complete data. The study was approved by the institutional research ethics board of the CISSS Montérégie-Centre (#2021-563).
Measures
Dependent variables of interest
Temporal patterns of moderate or severe symptoms of either anxiety or depression (MSS-ANXDEP) during the pandemic
Anxiety was assessed at both surveys with the 7-item Generalized Anxiety Disorder Scale (GAD-7) (score range 0–21) (Spitzer et al., 2006). A cutoff score of ≥ 10 has been recommended as a positive screen for anxiety representing moderate and severe symptoms. Depression was based on a cutoff score of ≥ 10 on 8 items of the Patient Health Questionnaire (PHQ-8) (score range 0–24), representing moderate to severe depressive symptoms (Kroenke et al., 2009). Information from both 2018 and 2020 (May–Dec 2020) surveys was considered to create a four-level mutually exclusive dummy variable that would summarize the presence of moderate or severe symptoms of either anxiety or depression (MSS-ANXDEP) at each survey: no MSS at either survey; remitted (MSS present in 2018, pre-COVID, but not present in 2020); incident (MSS not present in 2018 but was present in 2020); or persistent (MSS present in both 2018 and 2020).
Independent variables
Sociodemographic and economic factors
Sociodemographic factors assessed included age categorized into four groups (35–44 years, 45–54 years, 55–64 years, ≥ 65 years), gender (male, female, other gender diverse groups), and race/ethnicity (yes, self-identified as White, or no, self-identified as Arab, Black, East Asian, Filipino, Jewish, Latin American/Hispanic, South Asian, South-East Asian, West-Asian, Other). The CanPath regional cohort that individuals belonged to was also considered. Economic factors assessed total household income before taxes in the previous year (categorized as < $24,999, $25,000–$49,999, $50,000–$74,999, $75,000–$99,999, $100,000–$149,999, ≥ $150,000; or prefer not to respond, doesn’t know/missing); decrease in income during the pandemic (yes/no); loss of job during the pandemic (yes/no); and work status (categorized as full-time or part-time employed/self-employed, retired, looking after home and/or family/doing unpaid or voluntary work/student, unable to work because of sickness or disability, unemployed, prefer not to answer/missing data). Respondents were also asked whether they worked as a medical professional, as well as category of professional with exposure to patients (e.g., physician, nurse, hospital employee, first responder, pharmacist) (yes/no) and whether they worked as an essential service provider with regular exposure to members of the public (e.g., grocery store attendant, public transit, police, security) (yes/no).
Lifestyle and health behaviour factors
Lifestyle habits included past-month smoking (occasionally/daily or not at all), the presence of past-year cannabis use (yes or no), and past-year average weekly alcohol consumption (never, less than daily (≤ 5 times a week), or almost daily (6–7 times a week)).
Psychosocial factors
Factors included providing since March 2020 any kind of help to others (e.g., emotional/psychological, medical, informational, financial, practical, other) because of the pandemic (yes/no); receipt of informational, financial, or practical support (e.g., housing, childcare, food delivery, material goods furniture, clothing; yes/no); and change in relationship with friends, family, and partner (categorized as follows: more distant or strained than before the pandemic, about the same as before the pandemic, has become closer than before the pandemic, prefer not to respond/missing data).
Clinical factors
Self-reported lifetime diagnosis of a mental disorder was based on whether a doctor had ever told the respondent that they had a mental health condition and categorized as yes, no, or not answered/not reported. Physical multimorbidity was based on self-reported lifetime physician diagnosis of physical disorders (e.g., cancer, diabetes, heart and circulatory conditions, cardiovascular disorder, respiratory system conditions, gastrointestinal diseases, liver or pancreatic conditions, renal disease, kidney conditions, neurological conditions, bone and joint conditions, and immune system conditions) and categorized as no (0) chronic physical or neurologic condition, 1 to 2 chronic conditions, or ≥ 3 chronic conditions.
Data analyses
Descriptive statistics and group comparisons were based on chi-square statistics. Multivariable multinomial regression analyses were carried out to study the outcome change of anxiety and depression as a function of sociodemographic and economic, lifestyle and health behaviour, psychosocial, and clinical factors. Analyses were stratified according to gender (female, male) and age group (< 65 years, ≥ 65 years). Multicollinearity between variables was not observed. Adjusted odds ratios (AOR) and 95% confidence intervals (CI) were computed to determine the strength of associations. Differences observed in stratified analyses were considered significant if 95% confidence intervals did not overlap. Analyses were carried out using SAS version 9.4 (SAS Institute 2013).
Results
Most of the sample identified as White (93.6%) and female (65.0%), and were aged 65 years and older (47.9%) (Table 1). Characteristics of the study sample according to the temporal patterns in MSS-ANXDEP are presented in Table 1. The proportion of participants reporting the absence of MSS-ANXDEP at either survey was 85.7% and of those reporting remitted, incident, and persistent MSS-ANXDEP was 5.2%, 5.7%, and 3.4%, respectively.
Results from the multivariable analyses in the overall sample are presented in Table 2. Overall, as compared to older adults aged ≥ 65 years, individuals aged 35–44 years, those aged 45–54 years, and those aged 55–64 years were more likely to experience remitted, incident, and persistent MSS-ANXDEP. As compared to males, females and other gender diverse groups also experienced a change in symptoms and had remitted, incident, and persistent MSS-ANXDEP. Individuals self-declaring as White were less likely to experience remission in MSS-ANXDEP.
As compared to individuals reporting pre-pandemic income in the ≥ $150,000 bracket, those reporting income in all other lower income brackets were more likely to experience remitted and persistent MSS-ANXDEP, whereas those reporting pre-pandemic income in the < $25,000 and $25,000–$49,999 brackets were more likely to experience incident MSS-ANXDEP. A decrease in income during the pandemic was associated with change in MSS-ANXDEP, whereas loss of employment during the pandemic was not.
Individuals who were unable to work due to illness or disability were more likely to experience remitted, incident, and persistent MSS-ANXDEP. Individuals who reported being unemployed were also more likely to experience remitted MSS-ANXDEP. Individuals looking after home and/or family, doing unpaid or voluntary work, or being a student did not experience changes in MSS-ANXDEP. Essential workers who reported contact with the public were more likely to experience remitted, incident, and persistent MSS-ANXDEP. Medical professionals did not experience a change in MSS-ANXDEP.
Individuals reporting current smoking, past-year cannabis use, and drinking alcohol more often since the pandemic were more likely to experience remitted, incident, and persistent MSS-ANXDEP.
Individuals providing help to others because of the pandemic were less likely to experience persistent MSS-ANXDEP. Individuals receiving informational, financial, or practical support during the pandemic were more likely to report incident MSS-ANXDEP. Individuals reporting a more distant or strained relationship than before the pandemic with friends, family, and partner experienced remitted, incident, and persistent MSS-ANXDEP.
Individuals reporting a lifetime physician diagnosis of a mental disorder and multimorbidity were more likely to experience remitted, incident, and persistent MSS-ANXDEP.
Results from the multivariable analyses restricted to participants aged < 65 years and ≥ 65 years are presented in Supplementary Tables 1 and 2. In general, the temporal patterns of MSS-ANXDEP observed in the overall sample are similar in individuals aged < 65 years and those ≥ 65 years with few exceptions. Older adults aged ≥ 65 years also reporting a lifetime physician diagnosis of a mental disorder were more likely to experience incident MSS-ANXDEP and multimorbidity than adults aged < 65 years. Results from the multivariable analyses restricted to females and males are presented in Supplementary Tables 3 and 4. In general, the factors associated with the temporal patterns of MSS-ANXDEP observed in the overall sample are similar in females and males. Of interest, females who reported current smoking were more likely to experience MSS-ANXDEP.
Discussion
This study contributes to the present literature by documenting the temporal patterns of MSS of either anxiety or depression in a large sample of adults and older adults across Canada from before to during the first two waves of the pandemic and reporting on associated factors in the overall sample and restricted by age groups and gender. The prevalence of absent, remitted, incident, and persistent MSS of either anxiety or depression in the current study was 85.7%, 5.2%, 5.7%, and 3.4%, respectively. A Norwegian cohort study similarly showed pre-pandemic prevalence of mental disorders of 15.4% and ranging from 9.0% to 14.3% during the early phases of the pandemic (March to September 2020) (Knudsen et al., 2022). Our study findings are also similar to a longitudinal German cohort study which highlights that among those who screened positive for depression in 2019, 33.6% and 21.9% also screened positive for depression and anxiety in 2021, whereas among those who did not screen positive for depression in 2019, 9.8% and 6.5% screened positive for depression and anxiety in 2021 (Benke et al., 2022). Longitudinal studies with increased number of follow-ups including measures before and during the pandemic are needed to better describe the temporal patterns of anxiety and depression.
Priorities for value-based health systems include equitable distribution of health regardless of ethnicity, income, or place of residence (Smith et al., 2021). Older adults in the current study were less likely to experience MSS-ANXDEP, which has been similarly reported elsewhere (Public Health Agency of Canada, 2022). However, the stratified analyses showed that older adults with a lifetime physician diagnosis of a mental disorder were more likely to experience MSS-ANXDEP during the pandemic than younger adults aged < 65 years. Factors such as increased isolation during the pandemic in older adults may in part explain this finding (Lara et al., 2023). The current study highlighted potential socio-economic inequities in the temporal patterns of anxiety and depression, even after considering health status and sociodemographic factors and health and lifestyle behaviours. Findings showed that individuals experiencing persistent MSS-ANXDEP had lower income levels and reported a decrease in income during the pandemic. These findings may hint at the links between financial insecurity and mental health status (Hertz-Palmor et al., 2021) and the effect on perpetuating pre-existing social and economic inequities (Asmundson et al., 2020). Findings related to income (i.e., income prior to the pandemic and reporting a decrease in income since the pandemic) and its influence on incident and/or persistent MSS-ANXDEP are important to consider in the context of public health practice and policy. They can encourage practitioners to ask about changes in socio-economic factors during consultation, as well as inform decision- and policy-makers on allocation to mental health services and social security nets.
Findings from the current study also showed that essential workers experienced remitted, incident, and persistent MSS-ANXDEP. These findings suggest that the population of essential workers, which included professions working in direct contact with the public, may have been at greater risk of new anxiety and depression symptoms during the pandemic context, which encourages the need for access to mental health interventions for this specific population of workers.
Individuals experiencing MSS-ANXDEP also reported current smoking, cannabis use in the past year, and an increase in alcohol consumption since the pandemic, and this was similarly observed in adults and older adults, and females and males. To our knowledge, rare are the studies that have assessed age and gender differences in anxiety or depression in the context of the COVID-19 pandemic. Similar to our findings, one of the rare studies identified showed that smoking was associated with recurrent depression in females (Tibubos et al., 2019). A recent Canadian study showed a relationship between burnout and dependency to alcohol and/or cannabis suggesting their use as potential coping mechanisms (Mental Health Research Canada, 2023). Public health campaigns should reiterate the negative health effects of behaviours such as smoking, cannabis use, and alcohol consumption on health and mental health and provide access to integrated mental health support programs aimed at addressing multifaceted mental health needs.
In the current study, individuals experiencing incident MSS-ANXDEP also reported receiving informational, financial, and practical support from community. Individuals with no moderate or severe symptoms of anxiety provided help to others because of the pandemic. Research has shown that the majority of informal caregivers during the pandemic had experienced burden with more than one in four also experiencing symptoms of depression (Rajovic et al., 2021). Future research should also focus on the long-term mental health of individuals who gave support to their community and assess changes in patterns of anxiety or depression.
In the current study, strained relationships with friends, family, and partners during the first waves of pandemic were also associated with worse temporal patterns of anxiety and depression. Similar findings have been reported for symptoms of depression (James et al., 2022). The presence of quality relationships has been shown to protect against symptoms of depression during the pandemic (Pieh et al., 2020). An association between satisfaction with marital relationship and support for different family policies has also been shown (James et al., 2022). Family policies aimed at reducing the effect of the pandemic on family well-being include paid family leave, flexible payment plans for bills, unemployment benefits, accessibility to counseling and elder care, and housing assistance (Ben Brik, 2020). Government policy-makers in Canada lent financial and economic support to counteract the impact of COVID-19 pandemic on families with various recovery benefits (Chartered Professional Accountants (CPA) Canada, 2021). Future federal policies could also aim at increasing in all provinces accessibility to counseling (marital, parenting, mental health support), external resources for generating potential meaningful relationships in the community, and elder care to mitigate the negative impact of the pandemic on the mental health of Canadians and growing inequities in access to mental health care (Vasiliadis et al., 2021).
The current study has several strengths. It included a large sample of adults and older adults across Canada who contributed information before and during the pandemic, limiting the potential for recall and social desirability bias in the measurement of changes in symptoms of anxiety and depression. Study limitations also need to be considered. In addition to the sampling biases mentioned above, participants who completed the COVID-19 survey were more likely to report MSS-ANXDEP and to be females, older adults, and individuals reporting higher income, compared to those who only completed the 2018 survey. The potential effect on study results is difficult to predict as, on one hand, females are more likely than males to report symptoms of anxiety and depression, while on the other, older adults are less likely to report symptoms than adults, as are those with higher socio-economic status (Mosier et al., 2010; Yeretzian et al., 2023). As we looked at individual changes from prior to the pandemic, we expect the bias to be non-differential. Several independent variables that focused on capturing changes from before to during the pandemic were assessed during the 2020 pandemic survey and therefore may be subject to recall bias. Further, the measure of these variables overlapped with the follow-up measure of MSS-ANXDEP during the pandemic. Interpretation of findings and conclusions are therefore limited to the presence of associations. The study period included the first two waves of the pandemic, and therefore, findings on the temporal patterns may be generalizable to this period of the pandemic. The symptoms of anxiety and depression during the later waves of the pandemic need further study to assess the long-term association and effects of socio-economic and health behaviours on temporal patterns of anxiety and depression. Factors associated with balancing work and childcare obligations due to school closures were not ascertained in this study. Finally, the sample did not include individuals in institutions who may present with more complex mental health problems, and therefore, results may be generalizable to community-living adults and older adults insured under public health systems.
Conclusion
The present study showed the presence of health and socio-economic inequities associated with persistent, incident, and remitted MSS-ANXDEP from before to during the COVID-19 pandemic. This highlights the need for renewed, coordinated, and interdisciplinary efforts around public health campaigns targeting the promotion of healthy behaviours, as well as the development and implementation of health policies that aim to reduce barriers and improve access to integrated substance use and mental health care within primary and community-based settings.
Contributions to knowledge
What does this study add to existing literature?
-
The current study highlights the presence of sociodemographic and economic factors associated with persistent and incident cases of moderate or severe symptoms of either anxiety or depression, which may increase gaps further with respect to mental health needs.
-
The worsening of the quality of relationships with friends, family, and partners during the pandemic was associated with changes in moderate or severe symptoms of either anxiety or depression.
-
Health behaviours such as smoking, cannabis use, and drinking more alcohol were associated with changes in moderate or severe symptoms of either anxiety or depression.
What are the key implications for public health interventions, practice, or policy?
-
Priorities for population health and value-based health systems include equitable distribution of health. Increased focus should therefore be on those reporting lower income and reduced income from prior to the pandemic, females and gender diverse populations, and essential workers.
-
Public health campaigns should reiterate the negative health effects of smoking, cannabis use, and alcohol consumption and provide access to integrated substance and mental health programs.
-
Public health policies should be tailored to meet the mental health and service needs of populations that may be more at risk in the aftermath of the pandemic such as those with loss of income, reporting worsening of relationships since the pandemic, and females and gender diverse populations. Reducing economic and social barriers to mental health should be considered.
Data availability
The authors are not legally authorized to share or publicly publish CanPath data. Participants were not requested to give informed consent for data sharing. Requests for access to the data should be addressed to CanPath.
Change history
12 February 2024
A Correction to this paper has been published: https://doi.org/10.17269/s41997-024-00864-y
References
Abramson, C. M., & Portacolone, E. (2017). What is new with old? What old age teaches us about inequality and stratification. Sociol Compass, 11(3). https://doi.org/10.1111/soc4.12450
Asmundson, G. J. G., Blackstock, C., Bourque, M. C., Brimacombe, G., Crawford, A., Deacon, S. H., et al. (2020). Easing the disruption of COVID-19: Supporting the mental health of the people of Canada—October 2020—an RSC Policy Briefing. FACETS, 5(1), 1071–1098. https://doi.org/10.1139/facets-2020-0082
Ben Brik, A. (2020). International study on the impact of COVID 19 on family life across cultures. https://doi.org/10.17605/OSF.IO/DTCF7
Benke, C., Asselmann, E., Entringer, T. M., & Pané-Farré, C. A. (2022). The role of pre-pandemic depression for changes in depression, anxiety, and loneliness during the COVID-19 pandemic: Results from a longitudinal probability sample of adults from Germany. Eur Psychiatry, 65(1), e76. https://doi.org/10.1192/j.eurpsy.2022.2339
Bolton, D., & Gillett, G. (2019). The biopsychosocial model of health and disease: New philosophical and scientific developments. Springer Nature.
Carrese-Chacra, E., Hollett, K., Erdem, G., Miller, S., & Gouin, J.-P. (2023). Longitudinal effects of pandemic stressors and dyadic coping on relationship satisfaction during the COVID-19 pandemic. Family Relations, 72(3), 645–664. https://doi.org/10.1111/fare.12885
Chartered Professional Accountants (CPA) Canada. (2021). Financial and economic support during COVID-19 pandemic: Federal updates. https://www.cpacanada.ca/en/public-interest/public-policy-government-relations/federal-updates-covid19-financial-economic-support. Accessed 2 Aug 2023
Chen, D. T., & Wang, Y. J. (2021). Inequality-related health and social factors and their impact on well-being during the COVID-19 pandemic: Findings from a national survey in the UK. Int J Environ Res Public Health, 18(3). https://doi.org/10.3390/ijerph18031014
Chisholm, D., Sweeny, K., Sheehan, P., Rasmussen, B., Smit, F., Cuijpers, P., et al. (2016). Scaling-up treatment of depression and anxiety: A global return on investment analysis. The Lancet Psychiatry, 3(5), 415–424. https://doi.org/10.1016/S2215-0366(16)30024-4
COVID-19 Mental Disorders Collaborators. (2021). Global prevalence and burden of depressive and anxiety disorders in 204 countries and territories in 2020 due to the COVID-19 pandemic. Lancet, 398(10312), 1700–1712. https://doi.org/10.1016/s0140-6736(21)02143-7
Dannefer, D. (2001). Age stratification. In N. J. Smelser & P. B. Baltes (Eds.), International encyclopedia of the social & behavioral sciences (pp. 278–283). Pergamon.
Dummer, T. J. B., Awadalla, P., Boileau, C., Craig, C., Fortier, I., Goel, V., et al. (2018). The Canadian Partnership for Tomorrow Project: A pan-Canadian platform for research on chronic disease prevention. Canadian Medical Association Journal, 190(23), E710–E717. https://doi.org/10.1503/cmaj.170292
Dykxhoorn, J., Fischer, L., Bayliss, B., Brayne, C., Crosby, L., Galvin, B., et al. (2022). Conceptualising public mental health: Development of a conceptual framework for public mental health. BMC Public Health, 22(1), 1407. https://doi.org/10.1186/s12889-022-13775-9
Frazier, L. D. (2020). The past, present, and future of the biopsychosocial model: A review of The Biopsychosocial Model of Health and Disease: New philosophical and scientific developments by Derek Bolton and Grant Gillett. New Ideas in Psychology, 57, 100755. https://doi.org/10.1016/j.newideapsych.2019.100755
Hertz-Palmor, N., Moore, T. M., Gothelf, D., DiDomenico, G. E., Dekel, I., Greenberg, D. M., et al. (2021). Association among income loss, financial strain and depressive symptoms during COVID-19: Evidence from two longitudinal studies. J Affect Disord, 291, 1–8. https://doi.org/10.1016/j.jad.2021.04.054
Hohls, J. K., König, H. H., Quirke, E., & Hajek, A. (2021). Anxiety, depression and quality of life-A systematic review of evidence from longitudinal observational studies. Int J Environ Res Public Health, 18(22). https://doi.org/10.3390/ijerph182212022
Holwerda, T. J., Jaarsma, E., van Zutphen, E. M., Beekman, A. T. F., Pan, K. Y., van Vliet, M., Stringa, N., van den Besselaar, J. H., MacNeil-Vroomen, J. L., Hoogendijk, E. O., & Kok, A. A. L. (2023). The impact of COVID-19 related adversity on the course of mental health during the pandemic and the role of protective factors: A longitudinal study among older adults in The Netherlands. Social Psychiatry and Psychiatric Epidemiology, 58(7), 1109–1120. https://doi.org/10.1007/s00127-023-02457-5
Inchausti, F., MacBeth, A., Hasson-Ohayon, I., & Dimaggio, G. (2020). Telepsychotherapy in the age of COVID-19: A commentary (Vol. 30, pp. 394–405). Educational Publishing Foundation.
Institute of Medicine (US) Board on Population Health and Public Health Practice. (2012). Sex-specific reporting of scientific research: A workshop summary. Washington (DC): National Academies Press (US).
James, S., Ben Brik, A., Jorgensen-Wells, M., Esteinou, R., Acero, I. D. M., Mesurado, B., Debeljuh, P., Orellana, O. N. (2022). Relationship quality and support for family policy during the COVID-19 pandemic. Family Relations. https://doi.org/10.1111/fare.12705
Knudsen, A. K. S., Skogen, J. C., Stene-Larsen, K., Gustavson, K., & Reneflot, A. (2022). Met and unmet need for mental health care before and during the COVID-19 pandemic. Eur J Public Health, 32(1), 49–51. https://doi.org/10.1093/eurpub/ckab183
Kroenke, K., Strine, T. W., Spitzer, R. L., Williams, J. B., Berry, J. T., & Mokdad, A. H. (2009). The PHQ-8 as a measure of current depression in the general population. J Affect Disord, 114(1-3), 163-173. https://doi.org/10.1016/j.jad.2008.06.026.
Lara, E., Matovic, S., Vasiliadis, H. M., Grenier, S., Berbiche, D., de la Torre-Luque, A., et al. (2023). Correlates and trajectories of loneliness among community-dwelling older adults during the COVID-19 pandemic: A Canadian longitudinal study. Arch Gerontol Geriatr, 115, 105133. https://doi.org/10.1016/j.archger.2023.105133
Mental Health Research Canada. (2023). Understanding the mental health of Canadians through COVID-19 and beyond: Poll #16. MHRC. https://static1.squarespace.com/static/5f31a311d93d0f2e28aaf04a/t/646f6a54935f355d45369256/1685023317959/2022May25_MHRC+Poll+16+Full+Report.pdf. Accessed August 3, 2023.
Mosier, K. E., Vasiliadis, H. M., Lepnurm, M., Puchala, C., Pekrul, C., & Tempier, R. (2010). Prevalence of mental disorders and service utilization in seniors: Results from the Canadian community health survey cycle 1.2. Int J Geriatr Psychiatry, 25(10), 960–967. https://doi.org/10.1002/gps.2434
Pieh, C., O’Rourke, T., Budimir, S., & Probst, T. (2020). Relationship quality and mental health during COVID-19 lockdown. PLoS One, 15(9), e0238906. https://doi.org/10.1371/journal.pone.0238906
Prime, H., Wade, M., & Browne, D. T. (2020). Risk and resilience in family well-being during the COVID-19 pandemic. Am Psychol, 75(5), 631–643. https://doi.org/10.1037/amp0000660
Public Health Agency of Canada. (2020). People who are at high risk for severe illness from COVID-19. Public Health Agency of Canada. https://www.canada.ca/en/public-health/services/publications/diseases-conditions/people-high-risk-for-severe-illness-covid-19.html. Accessed 20 Apr 2020
Public Health Agency of Canada. (2021). Symptoms of anxiety and depression during the COVID-19 pandemic. https://www.canada.ca/content/dam/hc-sc/documents/services/publications/diseases-conditions/symptoms-anxiety-depression-covid-19-pandemic/symptoms-anxiety-depression-covid-19-pandemic-en.pdf. Accessed 20 Apr 2022
Public Health Agency of Canada. (2022). What did Canadians do for their mental health during the COVID-19 pandemic? Public Health Agency of Canada. https://www.canada.ca/en/public-health/services/publications/diseases-conditions/what-did-canadians-do-for-mental-health-during-covid-19.html. Accessed July 2022.
Raina, P., Wolfson, C., Griffith, L., Kirkland, S., McMillan, J., Basta, N., et al. (2021). A longitudinal analysis of the impact of the COVID-19 pandemic on the mental health of middle-aged and older adults from the Canadian Longitudinal Study on Aging. Nature Aging, 1(12), 1137–1147. https://doi.org/10.1038/s43587-021-00128-1
Rajovic, T., Todorovic, N., Vracevic, M., Rajovic, N., Pavlovic, A., Pavlovic, V., et al. (2021). From burden to depressive symptoms in informal caregivers during the COVID-19 pandemic: A path analysis. Int J Environ Res Public Health, 18(18). https://doi.org/10.3390/ijerph18189577
Robillard, R., Daros, A. R., Phillips, J. L., Porteous, M., Saad, M., Pennestri, M. H., et al. (2021). Emerging new psychiatric symptoms and the worsening of pre-existing mental disorders during the COVID-19 pandemic: A Canadian multisite study: Nouveaux symptômes psychiatriques émergents et détérioration des troubles mentaux préexistants durant la pandémie de la COVID-19: une étude canadienne multisite. Can J Psychiatry, 66(9), 815–826. https://doi.org/10.1177/0706743720986786
SAS Institute. (2013). The SAS system for Windows (version 9.4). SAS Institute.
Smith, P. C., Sagan, A., Siciliani, L., Panteli, D., McKee, M., Soucat, A., et al. (2021). Building on value-based health care: Towards a health system perspective. Copenhagen, Danemark: WHO.
Spitzer, R. L., Kroenke, K., Williams, J. B. W., & Löwe, B. (2006). A brief measure for assessing Generalized Anxiety Disorder: The GAD-7. Arch Intern Med, 166(10), 1092–1097. https://doi.org/10.1001/archinte.166.10.1092
Statistics Canada. (2021). COVID-19 in Canada: A one-year update on social and economic impacts. Statistics Canada.
Teisberg, E., Wallace, S., & O’Hara, S. (2020). Defining and implementing value-based health care: A strategic framework. Acad Med, 95(5), 682–685. https://doi.org/10.1097/acm.0000000000003122
Ten Have, M., Tuithof, M., van Dorsselaer, S., Schouten, F., Luik, A. I., & de Graaf, R. (2023). Prevalence and trends of common mental disorders from 2007-2009 to 2019-2022: Results from the Netherlands Mental Health Survey and Incidence Studies (NEMESIS), including comparison of prevalence rates before vs. during the COVID-19 pandemic. World Psychiatry, 22(2), 275–285. https://doi.org/10.1002/wps.21087
Tibubos, A. N., Brähler, E., Ernst, M., Baumgarten, C., Wiltink, J., Burghardt, J., et al. (2019). Course of depressive symptoms in men and women: Differential effects of social, psychological, behavioral and somatic predictors. Scientific Reports, 9(1), 18929. https://doi.org/10.1038/s41598-019-55342-0
Vasiliadis, H. M., Spagnolo, J., & Lesage, A. (2021). Public funding of evidence-based psychotherapy for common mental disorders: Increasing calls for action in Canadian provinces. Healthc Policy, 16(3), 16-25. https://doi.org/10.12927/hcpol.2021.26437.
World Health Organization. (2022). COVID-19 pandemic triggers 25% increase in prevalence of anxiety and depression worldwide. WHO. https://www.who.int/news/item/02-03-2022-covid-19-pandemic-triggers-25-increase-in-prevalence-of-anxiety-and-depression-worldwide. Accessed October 19, 2022.
Yeretzian, S. T., Sahakyan, Y., Kozloff, N., & Abrahamyan, L. (2023). Sex differences in the prevalence and factors associated with anxiety disorders in Canada: A population-based study. J Psychiatr Res, 164, 125–132. https://doi.org/10.1016/j.jpsychires.2023.06.018
Acknowledgements
The data used in this research were made available by CanPath—Canadian Partnership for Tomorrow’s Health (formerly the Canadian Partnership for Tomorrow Project), and the 5 regional cohorts of the British Columbia Generations Project, Alberta’s Tomorrow Project, Ontario Health Study, CARTaGENE, and Atlantic Partnership for Tomorrow’s Health. CanPath is supported by the Canadian Partnership Against Cancer and Health Canada, BC Cancer, Genome Quebec, Centre Hospitalier Universitaire (CHU) Sainte-Justine, Dalhousie University, Ontario Institute for Cancer Research, Alberta Health, Alberta Cancer Foundation, and Alberta Health Services. The views expressed herein represent the views of the authors and not of CanPath, the regional cohorts, or its funders. The authors would like to thank Nolwenn Noisel for her collaboration in obtaining funding for the study and Djamal Berbiche, PhD, for statistical support.
Funding
The current project was funded by a Canadian Institutes of Health Research (CIHR) grant (grant #02211-000). The funder had no role in the study design, data collection, analysis and interpretation, and draft and revision of the paper nor in the decision to submit for publication.
Author information
Authors and Affiliations
Contributions
Conceptualization, obtaining of funding: HMV, JS, MJF, JPG, PR, SG, JL; analysis: HMV; writing of the first draft: HMV; critical review of manuscript: HMV, JS, MJF, JPG, PR, MB, SG, GST, JEV, CLL, JL
Corresponding author
Ethics declarations
Ethics approval
The study was approved by the institutional research ethics board of the CISSS Montérégie-Centre (#2021-563). All procedures performed involving human participants were in accordance with the ethical standards of the 1964 Helsinki Declaration and its later amendments.
Consent to participate
All participants gave informed consent to participate in this study.
Consent for publication
Not applicable
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article was updated to correct Table 1. The last line of the table (≥3 chronic physical conditions) was omitted from the original publication.
Supplementary information
ESM 1
(DOCX 112 kb)
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Vasiliadis, HM., Spagnolo, J., Bartram, M. et al. Factors associated with change in moderate or severe symptoms of anxiety and depression in community-living adults and older adults during the COVID-19 pandemic. Can J Public Health 115, 230–243 (2024). https://doi.org/10.17269/s41997-023-00832-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.17269/s41997-023-00832-y
Keywords
- Depression
- Anxiety
- Change in symptoms
- Temporal patterns
- Socio-economic, health and lifestyle behaviours
- Psychosocial
- COVID-19
- Pandemic