Abstract
Objective
Being overweight or obese comprises a significant risk factor for atherosclerosis. Fat tissue also generates factors stimulating angiogenesis, the process by which new blood vessels form. The purpose of this paper is to assess concentrations of the vascular endothelial growth factor A (VEGF-A) and its soluble type-1 and type-2 receptors (sVEGFR-1 and sVEGFR-2) in plasma of patients with peripheral arterial disease (PAD) depending on the level of nutrition according to body mass index (BMI).
Methods
The study group included patients suffering from symptomatic PAD (n=46) in Fontaine classes IIa–IV without any history of neoplastic disease and who have a normal BMI (n=15), are overweight (n=21) or are obese (n=10). The control group (n=30) consisted of healthy non-smoking volunteers who were neither overweight nor obese. Venous blood plasma samples were collected from both groups at rest in the morning to determine plasma concentrations of VEGF-A, sVEGFR-1, and sVEGFR-2 using the enzymelinked immunosorbent assay (ELISA) method.
Results
The group of patients with PAD co-existent with being overweight or obese tended to have higher mean concentration levels of VEGF-A and sVEGFR-2 when compared with patients suffering from PAD with normal BMI. A statistically significant positive correlation was obtained between BMI and average plasma concentrations of sVEGFR-2 (R=0.37, P=0.0103). However, no significant correlation was noticed between BMI and VEGF-A or sVEGFR-1 concentrations.
Conclusions
A positive correlation determined between the level of antiangiogenic factor and BMI value may be indicative of the linearly growing prevalence of some antiangiogenic factors in patients with metabolic disorders, which may be one of numerous factors contributing to incomplete efficiency of collateral circulation development in patients with PAD.
中文概要
目 的
研究外周动脉疾病(PAD) 患者血浆中血管内皮 生长因子A(VEGF-A) 和它的可溶性1 型和2 型受体(sVEGFR-1 和sVEGFR-2) 的浓度与营 养水平的关系, 同时根据身体质量指数(BMI) 来评估营养水平。
创新点
将血管生成与超重和肥胖及下肢局部缺血联系起 来, 并根据BMI 评估了它们之间的关系。
方 法
研究组包括46 名Fontaine 等级IIa 至IV 且没有 任何肿瘤疾病史的PAD 症状患者, 其中15 名 BMI 正常, 21 名超重, 10 名肥胖。对照组由30 名不超重且不肥胖的健康非吸烟志愿者组成。试 验在上午休息时间采集两组静脉血的血浆标本, 用酶联免疫吸附(ELISA) 方法确定血浆中的 VEGF-A、sVEGFR-1 和sVEGFR-2 浓度。
结 论
如果PAD 患者同时伴随着超重或者肥胖, 会影 响血管再生的过程。sVEGFR-2 水平和BMI 值之 间有正相关关系, 这说明代谢紊乱患者中的一些 抗血管生成因子患病率的线性增长的原因, 同时 这可能是导致PAD 患者侧支循环发展效率不完 全的众多因素之一。
Similar content being viewed by others

1 Introduction
The incidence of overweight people (according to the World Health Organization: body mass index (BMI)=25.0–29.9 kg/m2) and obesity (BMI≥30 kg/m2) is rapidly growing. According to the WOBASZ study of 2005, obesity was identified in 20.2% of women and 20.6% of men in Poland (Biela et al., 2005). In addition, an increased rate of atherosclerosis including lower limb chronic ischemia and peripheral arterial disease (PAD) can be observed, which remains the leading cause of lower limb amputation (Tendera et al., 2011). Obesity is conducive to early development of atherosclerosis and is one of the main risk factors for cardiovascular diseases. Patients with PAD revealed increasing angiogenesis: the formation of new blood vessels from pre-existing ones, which is a compensation mechanism in response to ischemia and hypoxia. Vascular endothelial growth factor A (VEGF-A) is a key proangiogenic factor, whereas its soluble type-1 and type-2 receptors (sVEGFR-1 and sVEGFR-2, respectively) are considered to be angiogenic inhibitors (Proczka et al., 2003; Barańska et al., 2005). The main angiogenesis activators include hypoxia, cytokines, and oncogenes. Fat tissue is the source of many substances such as hormones and cytokines (e.g. interleukin-6) responsible for producing VEGF-A (Lijnen, 2008).
Atherosclerosis-related complications are the leading cause of death in numerous countries including Poland. Being overweight or obese is a proven risk factor for thromboembolic events, in the case of which haemostatic abnormalities play a crucial role (Swiatkowska-Stodulska et al., 2007). A number of studies have revealed deterioration in the balance between coagulation and fibrinolysis in overweight or obese people; however, there are only few studies concerning the issue of angiogenesis in relation to obese or overweight people and critical lower limb ischemia. The role of angiogenesis is emphasized in many physiological conditions (ulcer healing, monthly cycle, implantation and foetal development) as well as pathological states (tumour development, diabetic retinopathy) (Kajdaniuk et al., 2011). In addition, angiogenesis has been proven to contribute to the development of fat tissue and obesity (Bouloumié et al., 1998).
It appears that being overweight or obese may have a significant influence on the individual stages of angiogenesis due to the endocrine role of fat cells as the source of many cytokines and tissue hormones. There have already been attempts to apply proangiogenic factors (e.g. VEGF-A) in patients with limb ischemia for therapeutic purposes (Isner et al., 1996; Skóra et al., 2013), yet the full effectiveness of such a treatment is not clear. Therefore, researchers constantly seek factors to improve the efficiency of so-called “therapeutic angiogenesis”. It can be assumed that being overweight or obese may affect the healing processes of ischemic ulcers.
The aim of this study was to assess the concentrations of VEGF-A, sVEGFR-1, and sVEGFR-2 in plasma of patients with symptomatic PAD depending on the level of nutrition according to BMI, and to analyse the ratio of the concentrations of the angiogenic inhibitory factor to pro-angiogenic factor (sVEGFR-1 and VEGF-A, respectively).
2 Materials and methods
The study group included patients suffering from symptomatic PAD (n=46), including 18 females and 28 males, with average age (63±8.5) years, and with average BMI=(26.5±4.2) kg/m2, without any history of neoplastic disease. The control group consisted of 30 healthy non-smoking volunteers (15 females and 15 males, average age (55.9±5.7) years) who were neither overweight nor obese. Within the group of patients with PAD, three subgroups were determined according to BMI: those with normal body mass (BMI=18.5–24.9 kg/m2, n=15), those who were overweig ht (BMI=25.0–29.9 kg/m2, n=21), and those with obesity (BMI≥30 kg/m2, n=10).
The inclusion criteria were: confirmed by written consent for participation in the study; symptomatic PAD in the form of intermittent claudication or rest pain, also co-existent with ulceration or ischemic necrosis (in case of critical limb ischemia); confirmed by additional testing using the walking test, the ankle brachial index (ABI), and arterial duplex ultrasound. The exclusion criteria were: lack of consent to participate in the study, surgical invasion performed within the last month, venous thromboembolism within the last month, diabetic retinopathy, administration of oral antimetabolites of vitamin K (acenocoumarol, warfarin) or the so-called new oral anti-coagulants (dabigatran etexilate mesilate, rivaroxaban), co-existent diagnosed cancer or pregnancy.
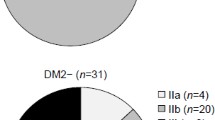
Venous blood plasma samples were collected from the experimental group and the control group at rest in the morning in order to measure concentrations of VEGF-A, sVEGFR-1, and sVEGFR-2 using the enzyme-linked immunosorbent assay (ELISA) method (R & D Systems, USA). Besides this, patients were classified into one of the stages of disease severity according to the Fontaine classification. One of the above-mentioned classification criteria is intermittent claudication (i.e. the distance a patient can walk before the onset of claudication pain related to ischemia preventing walking: over 200 m for class IIa; less than 200 m for class IIb), rest pain (class III) or ischemic ulceration (class IV). The characterization of the study group is shown in Table 1.
Laboratory tests were carried out on patients hospitalized at the Clinic of Vascular and Internal Medicine of Dr. Jan Biziel University Hospital No. 2 in Bydgoszcz (Poland), who were subject to diagnostic procedures towards PAD and qualified for further treatment. The consent of the Bioethics Commission of Ludwik Rydygier Collegium Medicum in Bydgoszcz, Nicolaus Copernicus University in Torun (CM UMK, Poland; document No. 509/2011) was obtained to conduct the tests, and the clinical investigations were carried out in accordance with the Helsinki Declaration. Participation in the study was voluntary and relied on additional collection of venous blood upon expressing free informed consent in writing with a relevant form.
All statistical calculations were performed using Statistica Version 10.0 software (StatSoft Inc., USA). Statistical analysis of the groups and subgroups was conducted using the Kruskal-Wallis test, and correlation was assessed by means of the Pearson and/or Spearman ratio; a significance level of P=0.05 was assumed.
3 Results
The subgroup of patients with PAD and normal BMI had 2 people classified into IIa, 7 into IIb and 6 into IV class according to the Fontaine classification. In the subgroup of patients with PAD who were overweight there were 3 persons classified into IIa, 13 into IIb, 3 into III, and 2 into IV class according to the Fontaine classification. Ten patients were classified into the IIb class according to the Fontaine classification, and accounted for the subgroup of people suffering from PAD co-existent with obesity.
Table 2 shows average plasma levels of VEGF-A, sVEGFR-1, and sVEGFR-2 in the control group and the subgroups of patients according to BMI.
The patients with PAD and normal BMI revealed higher mean VEGF-A levels in comparison to the control group ((76.3±103.6) vs. (18.0±7.7) pg/ml, P=0.002). The subgroups of patients with PAD co-existent with being overweight or obesity, respectively, were found to have higher average plasma concentrations of VEGF-A when compared to healthy people ((86.5±49.0) vs. (18.0±7.7) pg/ml, P=0.0001 and (92.0±80.4) vs. (18.0±7.7) pg/ml, P=0.00009, respectively).
No statistically significant differences were found in VEGF-A levels between the subgroup with PAD and normal BMI and the subgroups with PAD and high BMI values. However, an increasing trend in VEGF-A levels was observed within the study group in line with BMI growth.
No statistically significant differences were observed within mean plasma levels of sVEGFR-1 between the control group and the subgroups with PAD according to different BMI values. Likewise, the differences in sVEGFR-1 levels between individual subgroups of patients with PAD and normal BMI, overweight or obesity, respectively, were insignificant.
Table 2 also demonstrates mean plasma levels of sVEGFR-2 in the study group and the control group. The plasma levels of sVEGFR-2 in the subgroup of patients with PAD and normal BMI are significantly lower than those in the control group ((8329.0±2658.5) vs. (14 481.5±3669.9) pg/ml, P=0.000001). Lower than control group concentration levels were also observed in the subgroups of patients with PAD co-existent with being overweight or obese ((9731.8±2142.1) vs. (14 481.5±3669.9) pg/ml, P=0.0004 and (10 688.3±4141.5) vs. (14 481.5±3669.9) pg/ml, P=0.048, respectively). Besides this, the group of patients with PAD tended to have higher average plasma levels of sVEGFR-2 in line with an increasing BMI value. No statistically significant difference was observed within sVEGFR-2 concentration between the subgroup of patients with PAD and normal BMI and the subgroups of patients with PAD and high BMI.
Fig. 1 presents a statistically significant positive correlation between mean plasma levels of sVEGFR-2 and BMI values within the PAD group (R=0.37; P=0.0103).
No significant correlations were found, though, between BMI and VEGF-A levels or between BMI and sVEGFR-1 levels.
Table 3 shows the plasma sVEGFR-1 to VEGF-A ratio within the subjects who suffered from PAD and the control group.
As far as the control group is concerned, the average value of this rate was 10.00±7.49, while in the subgroup of patients with PAD and normal BMI the ratio was 4.16±4.10 and appeared to be significantly lower in comparison with the control group (P=0.014); in the subgroup with PAD co-existent with being overweight it was 1.91±1.05 and was also lower than in the control group (P=0.0001); while in the subgroup with PAD co-existent with obesity it was 2.57±2.22 and was proved to be significantly lower when compared to healthy counterparts (P=0.0005).
No statistically significant difference was observed as regards the value of this ratio between the subgroup of patients with PAD and normal BMI and the patients with PAD and higher BMI values.
4 Discussion
The study conducted showed that the patients with PAD and normal BMI had over 4-fold higher VEGF-A levels than healthy people, with accompanying lower levels of sVEGFR-2. The patients with PAD who were also overweight or obese were observed to have slightly increased VEGF-A concentrations when compared to the patients with PAD and normal BMI; higher levels of sVEGFR-2 were also observed.
An essential factor affecting increased VEGF-A levels in patients with PAD in comparison with healthy people, as also revealed in this study, is the presence of ischemia and hypoxia. This is the result of reduced blood flow through affected arterial vessels. Such observations can be found in relevant available publications (Findley et al., 2008; Stehr et al., 2010) and our own surveys (Wieczór et al., 2015a; 2015b). Nevertheless, the present study relied on assessing the possible effect of weight-related disorders on angiogenesis parameters in patients suffering from PAD. Higher VEGF-A levels were observed in overweight or obese patients suffering from PAD, and in patients with PAD and normal BMI when compared to healthy people with normal BMI. This is because arteriosclerosis, leading to narrowing of the lower extremity arteries, is a factor responsible for endomysial ischemia.
Oxygen deficiency in tissues is a strong stimulus that releases VEGF-A, the source of which is probably thrombocytes, inflammatory cells, and endothelial cells. The ischemic stimulus is very strong, as evidenced by a 4-fold higher level of VEGF-A in patients with PAD and normal body weight.
Patients with symptomatic PAD who were also overweight or obese tended to have higher average concentrations of the proangiogenic factor (VEGF-A). Findings concerning statistically insignificant higher VEGF-A levels in obese people, similar to the ones presented in this paper, were obtained by Rehman et al. (2003); however, that study was not concerned with patients with arteriosclerosis. Increased VEGF-A levels may be related to the intensification of angiogenic and hypoxia processes in patients with metabolic disorders. The influence of angiogenesis was proved in chronic inflammatory and neoplastic illnesses (Mizia-Malarz et al., 2008). However, numerous factors contributing to angiogenesis (placenta growth factor (PlGF), fibroblast growth factor (FGF), leptin, osteonectin, adiponectin, resistin, tissue factor (TF), tumor necrosis factor (TNF)-α, insulin-like growth factor (IGF), hepatocyte growth factor (HGF)) were identified in fat tissue. Yet, in vitro tests and studies in animals indicate that VEGF-A synthesized by fat cells has the largest impact on the angiogenic activity of fat tissue (Lijnen, 2008). In the present study there was a strong upward trend observed in VEGF-A concentration levels in patients with PAD in line with growing BMI values, suggesting that fat tissue is the source of such a concentration. Miyazawa-Hoshimoto et al. (2003) observed significantly higher levels of VEGF-A in overweight and obese people. Likewise, Silha et al. (2005) found increased VEGF-A levels in the blood of overweight or obese people, but no statistical significance was observed. Their study was also concerned with the issue of worse prognosis in patients with cancer as well as a higher risk of metastases in obese patients.
The literature we analyzed did not provide any studies on VEGF-A levels in patients with PAD who were also overweight or obese. Yet, the papers concerning the analysis of VEGF-A levels and selected risk factors of cardiovascular diseases also cover the assessment of BMI. Namely, two studies performed with large subject populations, the SAPHIR study (Salzburg Atherosclerosis Prevention Program in Subjects at High Individual Risk) in a group of 909 people and the Wada et al. (2011) study involving 423 subjects in the Health Evaluation Centre, investigated VEGF-A levels against BMI values among other things (Sandhofer et al., 2009). In the SAPHIR study, VEGF-A levels revealed a positive correlation with BMI values as opposed to the present study, presumably due to the small number of subjects. In their study, Wada et al. (2011) obtained similar findings to those in the SAPHIR study. Likewise, Loebig et al. (2010), when examining the phenomenon of insulin resistance, observed a positive correlation between VEGF-A levels and BMI values, but only considered the parameters of hormonal balance without taking account of the presence of atherosclerosis.
The sVEGFR-1 is a recognized angiogenic inhibitor. There were no substantial differences found in average sVEGFR-1 levels between patients with PAD and normal BMI and the subgroups with PAD and high BMI values in this study. This is in line with our previous observations in which no significant difference was found between sVEGFR-1 levels in patients with PAD in comparison with healthy people; it is also in line with the relevant literature (Findley et al., 2008; Wieczór et al., 2015b).
We observed significantly lower sVEGFR-2 levels in the blood of patients with PAD and differential BMI. According to the studies conducted before as well as the recent ones, sVEGFR-2 is a factor forming complexes with it, leading to a reduction in proangiogenic activity by decreasing the bioavailability of VEGF-A to receptors located on the surface of endothelial cells (Kou et al., 2004; Ahmadvand et al., 2010; Liu et al., 2014). Therefore, decreased levels of sVEGFR-2 result from the fact that this factor has been already used in this process.
In addition, the present study revealed that sVEGFR-2 levels increased in line with higher BMI in patients with PAD, and there was a statistically significant positive correlation between sVEGFR-2 levels and BMI. Therefore, this suggests that fat cells or/and endothelial cells, the number of which increases with increased BMI value (that is, with higher body weight), are probably the source of sVEGFR-2. Like in our study, Silha et al. (2005) obtained significantly higher sVEGFR-2 levels in overweight or obese people as well as a positive correlation between the levels of sVEGFR-2 and BMI without the presence of atherosclerosis.
In the present study we did not obtain significant correlations between BMI and VEGF-A levels or between BMI and sVEGFR-1 levels. However, in the SAPHIR study referred to above, the concentrations of sVEGFR-1 were determined and a positive correlation with BMI was achieved, but no statistical significance was obtained after adjusting the results with the age of subjects and the presence or lack of atherosclerotic lesions in the carotid arteries in the study group (Sandhofer et al., 2009).
As the available literature suggests, sVEGFR-1 is a recognized antiangiogenic factor. Therefore, the ratio of sVEGFR-1/VEGFR-A levels was applied as a measure of VEGF-A bioavailability in blood. The analysis of this rate conducted in the control group revealed a 10-fold antiangiogenic prevalence expressed by the ratio of sVEGFR-1 to VEGF-A levels. This prevalence was considerably lower (the ratio was 4.16; P=0.014) in the group of patients with PAD and normal BMI. Overweight and obesity co-existent with PAD led to a further decrease in the ratio to 1.91 in patients with PAD co-existent with being overweight (P=0.0001) and 2.57 in the patients with PAD and obesity (P=0.0005). Research into the sVEGFR-1 inhibitory mechanisms in relation to the angiogenic process suggests that the main direction of inhibition concerns blocking of VEGFR-2 present on the cell membrane and thus decreased availability of this receptor for VEGF-A (Liu et al., 2014). Yet, in this study no significant differences were observed within sVEGFR-1 levels between the control group and the study group with PAD and differential BMI. This suggests that a very strong growth in VEGF-A levels is the main cause of the reduced antiangiogenic potential (Rość et al., 2014).
The findings obtained in this study confirm the complex nature and contribution of numerous factors in the angiogenic process in patients suffering from atherosclerosis in the context of metabolic disorders, including the phenomena occurring in fat tissue (Lijnen, 2008). This surely requires further study in large populations of patients with PAD, with consideration of the participation of other angiogenic factors.
5 Conclusions
Co-existence of being overweight or obese in patients with symptomatic PAD probably affects increased angiogenic processes. Irrespective of BMI value and metabolic disorders, lower extremity artery disease remains the basic factor of ischaemia and hypoxy of peripheral tissues. The determined positive correlation of the angiogenic inhibitor concentrations (sVEGFR-2) and BMI may suggest that some factors inhibiting the angiogenic processes tend to prevail in patients with atherosclerosis co-existent with being overweight or obese and emphasizes the role of fat tissues next to endothelial cells in producing sVEGFR-2.
Compliance with ethics guidelines
Radoslaw WIECZÓR, Anna Maria WIECZÓR, Grazyna GADOMSKA, Katarzyna STANKOWSKA, Jacek FABISIAK, Karol SUPPAN, Grzegorz PULKOWSKI, Jacek BUDZYŃSKI, and Danuta ROŚĆ declare that they have no conflict of interest.
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008. Informed consent was obtained from all patients included in the study. Additional informed consent was obtained from all patients for whom identifying information is included in this article.
References
Ahmadvand, D., Rahbarizadeh, F., Iri-Sofla, F.J., et al., 2010. Inhibition of angiogenesis by recombinant VEGF receptor fragments. Lab. Med., 41(7):417–422. http://dx.doi.org/10.1309/lmmh2wyrlp7b3hjn
Barańska, P., Jerczynska, H., Pawlowska, Z., 2005. Vascular endothelial growth factor-structure and functions. Postepy Biochem., 51(1):12–21 (in Polish).
Biela, U., Pajak, A., Kaczmarczyk-Chalas, K., et al., 2005. Incidence of overweight and obesity in women and men between the ages of 20–74. Results of the WOBASZ program. Kardiol. Pol., 63(6 Suppl. 4):s632–s635 (in Polish).
Bouloumié, A., Drexler, H., Lafontan, M., et al., 1998. Leptin, the product of Ob gene, promotes angiogenesis. Circ. Res., 83(10):1059–1066. http://dx.doi.org/10.1161/01.res.83.10.1059
Findley, C.M., Mitchell, R.G., Duscha, B.D., et al., 2008. Plasma levels of soluble Tie2 and vascular endothelial growth factor distinguish critical limb ischemia from intermittent claudication in patients with peripheral arterial disease. J. Am. Coll. Cardiol., 52(5):387–393. http://dx.doi.org/10.1016/j.jacc.2008.02.045
Isner, J.M., Pieczek, A., Shainfeld, R., et al., 1996. Clinical evidence of angiogenesis after arterial gene transfer of phVEGF165 in patient with ischaemic limb. Lancet, 348(9024):370–374. http://dx.doi.org/10.1016/s0140-6736(96)03361-2
Kajdaniuk, D., Marek, B., Foltyn, W., et al., 2011. Vascular endothelial growth factor (VEGF) in endocrinology and oncology. Endokrynol. Pol., 62(Suppl. 3):14–22 (in Polish).
Kou, B., Li, Y., Zhang, L., et al., 2004. In vivo inhibition of tumor angiogenesis by a soluble VEGFR-2 fragment. Exp. Mol. Pathol., 76(2):129–137. http://dx.doi.org/10.1016/j.yexmp.2003.10.010
Lijnen, H.R., 2008. Angiogenesis and obesity. Cardiovasc. Res., 78(2):286–293. http://dx.doi.org/10.1093/cvr/cvm007
Liu, W., Zhang, X., Song, C., et al., 2014. Expression and characterization of a soluble VEGF receptor 2 protein. Cell Biosci., 4(1):14. http://dx.doi.org/10.1186/2045-3701-4-14
Loebig, M., Klement, J., Schmoller, A., et al., 2010. Evidence for relationship between VEGF and BMI independent of insulin sensitivity by glucose clamp procedure in a homogenous group healthy young men. PLOS ONE, 5(9): e12610. http://dx.doi.org/10.1371/journal.pone.0012610
Miyazawa-Hoshimoto, S., Takahashi, K., Bujo, H., et al., 2003. Elevated serum vascular endothelial growth factor is associated with visceral fat accumulation in human obese subjects. Diabetologia, 46(11):1483–1488. http://dx.doi.org/10.1007/s00125-003-1221-6
Mizia-Malarz, A., Sobol, G., Wos, H., 2008. Angiogenesis in the chronic inflammatory diseases and malignancies. Pol. Merkur. Lekarski, 24(141):185–189 (in Polish).
Proczka, R., Polanski, J., Malecki, M., et al., 2003. The significance of vascular endothelial growth factor in the neoangiogenesis process. The role of hypoxia in the endothelial cells proliferation process and in the formation of collateral circulation. Acta Angiol., 9(4):143–149 (in Polish).
Rehman, J., Considine, R.V., Bovenkerk, J.E., et al., 2003. Obesity is associated with increased levels of circulating hepatocyte growth factor. J. Am. Coll. Cardiol., 41(8): 1408–1413. http://dx.doi.org/10.1016/s0735-1097(03)00231-6
Rość, D., Wieczór, R., Stankowska, K., et al., 2014. Plasma VEGF-A/SVEGFR-1 ratio as a potential ischemic marker in patients with symptomatic peripheral arterial disease-preliminary report. Thromb Res., 133(Suppl. 3):S95. http://dx.doi.org/10.1016/s0049-3848(14)50305-2
Sandhofer, A., Tatarczyk, T., Kirchmair, R., et al., 2009. Are plasma VEGF and its soluble receptor sFlt-1 atherogenic risk factors? Cross-sectional data from the SAPHIR study. Atherosclerosis, 206(1):265–269. http://dx.doi.org/10.1016/j.atherosclerosis.2009.01.031
Silha, J.V., Krsek, M., Sucharda, P., et al., 2005. Angiogenic factors are elevated in overweight and obese individuals. Int. J. Obesity (Lond.), 29(11):1308–1314. http://dx.doi.org/10.1038/sj.ijo.0802987
Skóra, J., Barc, P., Pupka, A., et al., 2013. Transplantation of autologous bone marrow mononuclear cells with VEGF gene improves diabetic critical limb ischaemia. Endokrynol. Pol., 64(2):129–138. http://dx.doi.org/10.5114/aoms.2013.39935
Stehr, A., Töpel, I., Müller, S., et al., 2010. VEGF: a surrogate marker for peripheral vascular disease. Eur. J. Vasc. Endovasc., 39(3):330–332. http://dx.doi.org/10.1016/j.ejvs.2009.09.025
Swiatkowska-Stodulska, R., Kazimierska, E., Sworczak, K., et al., 2007. Hemostatic disturbances in obesity. Wiad. Lek., 60(3–4):185–188 (in Polish).
Tendera, M., Aboyans, V., Bartrelink, M.L., et al., 2011. ESC Guidelines on the diagnosis and treatment of peripheral artery diseases: document covering atherosclerotic disease of extracranial carotid and vertebral, mesenteric, renal, upper and lower extremity arteries. The task force on the diagnosis and treatment of peripheral artery diseases of the European Society of Cardiology (ESC). Eur. Heart J., 32(22):2851–2906. http://dx.doi.org/10.1093/eurheartj/ehr211
Wada, H., Ura, S., Kitaoka, S., et al., 2011. Distinct characteristics of circulating vascular endothelial growth factor-A and C levels in human subjects. PLOS ONE, 6(12): e29351. http://dx.doi.org/10.1371/journal.pone.0029351
Wieczór, R., Gadomska, G., Ruszkowska-Ciastek, B., et al., 2015a. Impact of type 2 diabetes on the plasma levels of vascular endothelial growth factor and its soluble receptors type 1 and type 2 in patients with peripheral arterial disease. J. Zhejiang Univ.-Sci. B (Biomed. & Biotechnol.), 16(11):948–956. http://dx.doi.org/10.1631/jzus.B1500076
Wieczór, R., Gadomska, G., Góralczyk, B., et al., 2015b. Selected angiogenic factors in plasma of patients with lower limb symptomatic peripheral arterial disease—preliminary report. Int. Angiol., 34(6):545–551.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Wieczór, R., Wieczór, A.M., Gadomska, G. et al. Overweight and obesity versus concentrations of VEGF-A, sVEGFR-1, and sVEGFR-2 in plasma of patients with lower limb chronic ischemia. J. Zhejiang Univ. Sci. B 17, 842–849 (2016). https://doi.org/10.1631/jzus.B1600009
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1631/jzus.B1600009
Keywords
- Overweight
- Obesity
- Angiogenesis
- Vascular endothelial growth factor
- Soluble type-1 and type-2 receptors
- Peripheral arterial disease