Abstract
The complex interaction between hematopoietic stem cells (HSCs) and their microenvironment in the human bone marrow ensures a life-long blood production by balancing stem cell maintenance and differentiation. This so-called HSC niche can be disturbed by malignant diseases. Investigating their consequences on hematopoiesis requires a deep understanding of how the niches function in health and disease. To facilitate this, biomimetic models of the bone marrow are needed to analyze HSC maintenance and hematopoiesis under steady state and diseased conditions. Here, 3D bone marrow models, their fabrication methods (including 3D bioprinting), and implementations recapturing bone marrow functions in health and diseases are presented.





Similar content being viewed by others
References
G.M. Crane, E. Jeffery, and S.J. Morrison: Adult haematopoietic stem cell niches. Nat. Rev. Immunol. 17, 573 (2017).
H. Yoshihara, F. Arai, K. Hosokawa, T. Hagiwara, K. Takubo, Y. Nakamura, Y. Gomei, H. Iwasaki, S. Matsuoka, K. Miyamoto, H. Miyazaki, T. Takahashi, and T. Suda: Thrombopoietin/MPL signaling regulates hematopoietic stem cell quiescence and interaction with the osteoblastic niche. Cell Stem Cell 1, 685 (2007).
L.M. Calvi, G.B. Adams, K.W. Weibrecht, J.M. Weber, D.P. Olson, M.C. Knight, R.P. Martin, E. Schipani, P. Divieti, F.R. Bringhurst, L.A. Milner, H.M. Kronenberg, and D.T. Scadden: Osteoblastic cells regulate the haematopoietic stem cell niche. Nature 425, 841 (2003).
Y. Kunisaki, I. Bruns, C. Scheiermann, J. Ahmed, S. Pinho, D. Zhang, T. Mizoguchi, Q. Wei, D. Lucas, K. Ito, J.C. Mar, A. Bergman, and P.S. Frenette: Arteriolar niches maintain haematopoietic stem cell quiescence. Nature 502, 637 (2013).
M. Acar, K.S. Kocherlakota, M.M. Murphy, J.G. Peyer, H. Oguro, C.N. Inra, C. Jaiyeola, Z. Zhao, K. Luby-Phelps, and S.J. Morrison: Deep imaging of bone marrow shows non-dividing stem cells are mainly peri-sinusoidal. Nature 526, 126 (2015).
I.G. Winkler, V. Barbier, B. Nowlan, R.N. Jacobsen, C.E. Forristal, J.T. Pattern, J.L. Magnani, and J.P. Levesque: Vascular niche E-selectin regulates hematopoietic stem cell dormancy, self renewal and chemore-sistance. Nat. Med. 18, 1651 (2012).
M.J. Kiel, O.H. Yilmaz, T. Iwashita, O.H. Yilmaz, C. Terhorst, and S.J. Morrison: SLAM family receptors distinguish hematopoietic stem and progenitor cells and reveal endothelial niches for stem cells. Cell 121, 1109 (2005).
J. Fujisaki, J. Wu, A.L. Carlson, L. Silberstein, P. Putheti, R. Larocca, W. Gao, T.I. Saito, C. Lo Celso, H. Tsuyuzaki, T. Sato, D. Cote, M. Sykes, T.B. Strom, D.T. Scadden, and C.P. Lin: In vivo imaging of Treg cells providing immune privilege to the haematopoietic stem-cell niche. Nature 474, 216 (2011).
A. Chow, D. Lucas, A. Hidalgo, S. Mendez-Ferrer, D. Hashimoto, C. Scheiermann, M. Battista, M. Leboeuf, C. Prophete, N. van Rooijen, M. Tanaka, M. Merad, and P.S. Frenette: Bone marrow CD169 + macrophages promote the retention of hematopoietic stem and progenitor cells in the mesenchymal stem cell niche. J. Exp. Med. 208, 261 (2011).
F. Arai, K. Hosokawa, H. Toyama, Y. Matsumoto, and T. Suda: Role of N-cadherin in the regulation of hematopoietic stem cells in the bone marrow niche. Ann. N. Y. Acad. Sci. 1266, 72 (2012).
M.A. Schroeder and J.F. DiPersio: Mobilization of hematopoietic stem and leukemia cells. J. Leukocyte Biol. 91, 47 (2012).
G. Klein: The extracellular matrix of the hematopoietic microenvironment. Experientia 51, 914 (1995).
S.K. Nilsson, M.E. Debatis, M.S. Dooner, J.A. Madri, P.J. Quesenberry, and P.S. Becker: Immunofluorescence characterization of key extracellular matrix proteins in murine bone marrow in situ. J. Histochem. Cytochem. 46, 371 (1998).
K.D. Rodgers, J.D. San Antonio, and O. Jacenko: Heparan sulfate proteoglycans: a GAGgle of skeletal-hematopoietic regulators. Dev. Dyn. 237, 2622 (2008).
V. Goncharova, N. Serobyan, S. lizuka, I. Schraufstatter, A. de Ridder, T. Povaliy, V. Wacker, N. Itano, K. Kimata, L.A. Orlovskaja, Y. Yamaguchi, and S. Khaldoyanidi: Hyaluronan expressed by the hematopoietic microenvironment is required for bone marrow hematopoiesis. J. Biol. Chem. 287, 25419 (2012).
L. Coulombel, I. Auffray, M.H. Gaugler, and M. Rosemblatt: Expression and function of integrins on hematopoietic progenitor cells. Acta Haematol. 97, 13 (1997).
C. Lee-Thedieck and J.P. Spatz: Biophysical regulation of hematopoietic stem cells. Biomater. Sci. 2, 1548 (2014).
M.R. Nelson and K. Roy: Bone-marrow mimicking biomaterial niches for studying hematopoietic stem and progenitor cells. J. Mater. Chem. 64, 3490 (2016).
M.A. Walasek, R. van Os, and G. de Haan: Hematopoietic stem cell expansion: challenges and opportunities. Ann. N. Y. Acad. Sci. 1266, 138 (2012).
H. Dombret and C. Gardin: An update of current treatments for adult acute myeloid leukemia. Blood 127, 53 (2016).
C. Nombela-Arrieta and S. Isringhausen: The role of the bone marrow stromal compartment in the hematopoietic response to microbial infections. Front. Immunol. 7, 689 (2016).
A. Knight: Animal experiments scrutinised: systematic reviews demonstrate poor human clinical and toxicological utility. Altex 24, 320 (2007).
E. Törnqvist, A. Annas, B. Granath, E. Jalkesten, I. Cotgreave, and M. Oberg: Strategic focus on 3R principles reveals major reductions in the use of animals in pharmaceutical toxicity testing. PLoS ONE 9, e101638 (2014).
J.S. Choi, B.P. Mahadik, and B.A.C. Harley: Engineering the hematopoietic stem cell niche: frontiers in biomaterial science. Biotechnol. J. 10, 1529 (2015).
S. Mendez-Ferrer, T.V. Michurina, F. Ferraro, A.R. Mazloom, B.D. Macarthur, S.A. Lira, D.T. Scadden, A. Ma’ayan, G.N. Enikolopov, and P.S. Frenette: Mesenchymal and haematopoietic stem cells form a unique bone marrow niche. Nature 466, 829 (2010).
J. Kiernan, P. Damien, M. Monaghan, R. Shorr, L. Mclntyre, D. Fergusson, A. Tinmouth, and D. Allan: Clinical studies of ex vivo expansion to accelerate engraftment after umbilical cord blood transplantation: a systematic review. Transfus. Med. Rev. 31, 173 (2017).
N. Pineault and A. Abu-Khader: Advances in umbilical cord blood stem cell expansion and clinical translation. Exp. Hematol. 43, 498 (2015).
J. Brandrup, E.H. Immergut, and E.A. Grulke: Polymer Handbook, 4th ed. John Wiley and Sons: New York, 1999).
C.A. Muth, C. Steinl, G. Klein, and C. Lee-Thedieck: Regulation of hematopoietic stem cell behavior by the nanostructured presentation of extracellular matrix components. PLoS ONE 8, e54778 (2013).
A.J. Engler, S. Sen, H.L. Sweeney, and D.E. Discher: Matrix elasticity directs stem cell lineage specification. Cell 126, 677 (2006).
C. Lee-Thedieck and J.P. Spatz: Artificial niches: biomimetic materials for hematopoietic stem cell culture. Macromol. Rapid Commun. 33, 1432 (2012).
S.S. Kumar, J.H. Hsiao, Q.D. Ling, I. Dulinska-Molak, G. Chen, Y. Chang, Y. Chang, Y.H. Chen, D.C. Chen, S.T. Hsu, and A. Higuchi: The combined influence of substrate elasticity and surface-grafted molecules on the ex vivo expansion of hematopoietic stem and progenitor cells. Biomaterials 34, 7632 (2013).
C.C. Zhang and H.F. Lodish: Murine hematopoietic stem cells change their surface phenotype during ex vivo expansion. Blood 105, 4314 (2005).
Y. Zhou, H. Chen, H. Li, and Y. Wu: 3D culture increases pluripotent gene expression in mesenchymal stem cells through relaxation of cytoskele-ton tension. J. Cell. Mol. Med. 21, 1073 (2017).
L. Rodling, I. Schwedhelm, S. Kraus, K. Bieback, J. Hansmann, and C. Lee-Thedieck: 3D models of the hematopoietic stem cell niche under steady-state and active conditions. Sci. Rep. 7, 4625 (2017).
M.M. Cook, K. Futrega, M. Osiecki, M. Kabiri, A. Rice, K. Atkinson, G. Brooke, and M. Doran: Micromarrows—three-dimensional coculture of hematopoietic stem cells and mesenchymal stromal cells. Tissue Eng. Part C 18, 319 (2012).
E.C. Costa, D. de Melo-Diogo, A.F. Moreira, M.P. Carvalho, and I.J. Correia: Spheroids formation on non-adhesive surfaces by liquid overlay technique: considerations and practical approaches. Biotechnol. J. 13, 1–12 (2018).
F. Salamanna, D. Contartese, M. Maglio, and M. Fini: A systematic review on in vitro 3D bone metastases models: a new horizon to recapitulate the native clinical scenario? Oncotarget 7, 44803–44820 (2016).
A.M. Sitarski, H. Fairfield, C. Falank, and M.R. Reagan: 3d tissue engineered in vitro models of cancer in bone. ACS. Biomater. Sci. Eng. 4, 324 (2018).
J. Necas, L. Bartosikova, P. Brauner, and J. Kolar: Hyaluronic acid (hya-luronan): a review. Vet. Med. 53, 397 (2008).
B.D. Fairbanks, S.P. Singh, C.N. Bowman, and K.S. Anseth: Photodegradable, photoadaptable hydrogels via radical-mediated disulfide fragmentation reaction. Macromolecules 44, 2444 (2011).
J. Zhang, A. Skardal, and G.D. Prestwich: Engineered extracellular matrices with cleavable crosslinkers for cell expansion and easy cell recovery. Biomaterials 29, 4521 (2008).
P.M. Kharkar, K.L. Kiick, and A.M. Kloxin: Designing degradable hydro-gels for orthogonal control of cell microenvironments. Chem. Soc. Rev. 42, 7335 (2013).
F.R. Cheng, T. Su, J. Cao, X.L. Luo, L. Li, Y. Pu, and B. He: Environment-stimulated nanocarriers enabling multi-active sites for high drug encapsulation as an “on demand” drug release system. J. Mater. Chem. B 6, 2258 (2018).
C.M. Madl, B.L. LeSavage, R.E. Dewi, C.B. Dinh, R.S. Stowers, M. Khariton, K.J. Lampe, D. Nguyen, O. Chaudhuri, A. Enejder, and S.C. Heilshorn: Maintenance of neural progenitor cell sternness in 3D hydrogels requires matrix remodelling. Nat. Mater. 16, 1233 (2017).
T.M.A. Henderson, K. Ladewig, D.N. Haylock, K.M. McLean, and A. J. O’Connor: Cryogels for biomedical applications. J. Mater. Chem. B 1, 2682 (2013).
A. Raic, L. Rodling, H. Kalbacher, and C. Lee-Thedieck: Biomimetic mac-roporous PEG hydrogels as 3D scaffolds forthe multiplication of human hematopoietic stem and progenitor cells. Biomaterials 35, 929 (2014).
M.S. Ferreira, W. Jahnen-Dechent, N. Labude, M. Bovi, T. Hieronymus, M. Zenke, R.K. Schneider, and S. Neuss: Cord blood-hematopoietic stem cell expansion in 3D fibrin scaffolds with stromal support. Biomaterials 33, 6987 (2012).
S.S. Kotha, B.J. Hayes, K.T. Phong, M.A. Redd, K. Bomsztyk, A. Ramakrishnan, B. Torok-Storb, and Y. Zheng: Engineering a multicellular vascular niche to model hematopoietic cell trafficking. Stem Cell. Res. Ther. 9, 77 (2018).
S. Sieh, A.A. Lubik, J.A. Clements, C.C. Nelson, and D.W. Hutmacher: Interactions between human osteoblasts and prostate cancer cells in a novel 3D in vitro model. Organogenesis 6, 181 (2010).
A.B. Bello, H. Park, and S.H. Lee: Current approaches in biomaterial-based hematopoietic stem cell niches. Acta Biomater. 72, 1 (2018).
Y.S. Torisawa, C.S. Spina, T. Mammoto, A. Mammoto, J.C. Weaver, T. Tat, J.J. Collins, and D.E. Ingber: Bone marrow-on-a-chip replicates hematopoietic niche physiology in vitro. Nat. Methods 11, 663 (2014).
A. Reinisch, D.C. Hernandez, K. Schallmoser, and R. Majeti: Generation and use of a humanized bone-marrow-ossicle niche for hematopoietic xenotransplantation into mice. Nat. Protoc. 12, 2169 (2017).
C. Riether, C.M. Schurch, and A.F. Ochsenbein: Regulation of hematopoietic and leukemic stem cells by the immune system. Cell Death Differ. 22, 187 (2015).
E. Stieglitz and M.L. Loh: Genetic predispositions to childhood leukemia. Ther. Adv. Hematol. 4, 270 (2013).
T. Lapidot, C. Sirard, J. Vormoor, B. Murdoch, T. Hoang, J. Caceres-Cortes, M. Minden, B. Paterson, M.A. Caligiuri, and J.E. Dick: A cell initiating human acute myeloid leukaemia after transplantation into SCID mice. Nature 367, 645 (1994).
A.K. Brenner, I. Nepstad, and O. Bruserud: Mesenchymal stem cells support survival and proliferation of primary human acute myeloid leukemia cells through heterogeneous molecular mechanisms. Front. Immunol. 8, 106 (2017).
K. Schepers, E.M. Pietras, D. Reynaud, J. Flach, M. Binnewies, T. Garg, A.J. Wagers, E.C. Hsiao, and E. Passegue: Myeloproliferative neoplasia remodels the endosteal bone marrow niche into a self-reinforcing leukemic niche. Cell Stem Cell 13, 285 (2013).
R. Jacamo, Y. Chen, Z. Wang, W. Ma, M. Zhang, E.L. Spaeth, Y. Wang, V.L. Battula, P.Y. Mak, K. Schallmoser, P. Ruvolo, W.D. Schober, E.J. Shpall, M.H. Nguyen, D. Strunk, C.E. Bueso-Ramos, S. Konoplev, R.E. Davis, M. Konopleva, and M. Andreeff: Reciprocal leukemia-stroma VCAM-1/VLA-4-dependent activation of NF-kappaB mediates chemore-sistance. Blood 123, 2691 (2014).
Y. Saito, N. Uchida, S. Tanaka, N. Suzuki, M. Tomizawa-Murasawa, A. Sone, Y. Najima, S. Takagi, Y. Aoki, A. Wake, S. Taniguchi, L.D. Shultz, and F. Ishikawa: Induction of cell cycle entry eliminates human leukemia stem cells in a mouse model of AML. Nat. Biotechnol. 28, 275 (2010).
G.J. Cook, and T.S. Pardee: Animal models of leukemia: any closerto the real thing? Cancer Metastasis Rev. 32, 63 (2013).
M. de Jong, and T. Maina: Of mice and humans: are they the same?-Implications in cancertranslational research. J. Nucl. Med. 51, 501 (2010).
L. Demetrius: Of mice and men. EMBO Rep. 6, S39 (2005).
F. Ishikawa, S. Yoshida, Y. Saito, A. Hijikata, H. Kitamura, S. Tanaka, R. Nakamura, T. Tanaka, H. Tomiyama, N. Saito, M. Fukata, T. Miyamoto, B. Lyons, K. Ohshima, N. Uchida, S. Taniguchi, O. Ohara, K. Akashi, M. Harada, and L.D. Shultz: Chemotherapy-resistant human AML stem cells home to and engraft within the bone-marrow endosteal region. Nat. Biotechnol. 25, 1315 (2007).
C.R. Cogle, D.C. Goldman, G.J. Madlambayan, R.P. Leon, A.A. Masri, H.A. Clark, S.A. Asbaghi, J.W. Tyner, J. Dunlap, G. Fan, T. Kovacsovics, Q. Liu, A. Meacham, K.L. Hamlin, R.A. Hromas, E.W. Scott, and W.H. Fleming: Functional Integration of Acute Myeloid Leukemia into the Vascular Niche. Leukemia 28, 1978 (2014).
L.J. Bray, M. Binner, Y. Korner, M. von Bonin, M. Bornhauser, and C. Werner: A three-dimensional ex vivo tri-cultu re model mimics cell-cell interactions between acute myeloid leukemia and the vascular niche. Haematologica 102, 1215 (2017).
A. Bruce, R. Evans, R. Mezan, L. Shi, B.S. Moses, K.H. Martin, L.F. Gibson, and Y. Yang: Three-dimensional microfluidic tri-culture model of the bone marrow microenvironment for study of acute lymphoblastic leukemia. PLoS ONE 10, e0140506 (2015).
V. Trimarco, E. Ave, M. Facco, G. Chiodin, F. Frezzato, V. Martini, C. Gattazzo, F. Lessi, C.A. Giorgi, A. Visentin, M. Castelli, F. Severin, R. Zambello, F. Piazza, G. Semenzato, and L. Trentin: Cross-talk between chronic lymphocytic leukemia (CLL) tumor B cells and mesenchymal stromal cells (MSCs): implications for neoplastic cell survival. Oncotarget 6, 42130 (2015).
S. Tavor, I. Petit, S. Porozov, A. Avigdor, A. Dar, L. Leider-Trejo, N. Shemtov, V. Deutsch, E. Naparstek, A. Nagler, and T. Lapidot: CXCR4 regulates migration and development of human acute myelogenous leukemia stem cells in transplanted NOD/SCID mice. Cancer Res. 64, 2817 (2004).
S.C. Mills, P.H. Goh, J. Kudatsih, S. Ncube, R. Gurung, W. Maxwell, and A. Mueller: Cell migration towards CXCL12 in leukemic cells compared to breast cancer cells. Cell. Signal. 28, 316 (2016).
B.-S. Cho, H.-J. Kim, and M. Konopleva: Targeting the CXCL12/CXCR4 axis in acute myeloid leukemia: from bench to bedside. Korean J. Intern. Med. 32, 248 (2017).
A. Liou, C. Delgado-Martin, D.T. Teachey, and M.L. Hermiston: The CXCR4/CXCL12 axis mediates chemotaxis, survival, and chemoresist-ance in t-cell acute lymphoblastic leukemia. Stood 124, 3629 (2014).
E. Weisberg, A.K. Azab, P.W. Manley, A.L. Kung, A.L. Christie, R. Branson, I.M. Ghobrial, and J.D. Griffin: Inhibition of CXCR4 in CML cells disrupts their interaction with the bone marrow microenvironment and sensitizes them to nilotinib: potentiation of nilotinib by CXCR4 antagonist. Leukemia 26, 985 (2012).
E.L. Weisberg, M. Sattler, A.K. Azab, D. Eulberg, A. Kruschinski, P.W. Manley, R. Stone, and J.D. Griffin: Inhibition of SDF-1-induced migration of oncogene-driven myeloid leukemia by the L-RNA aptamer (Spiegelmer), N0X-A12, and potentiation of tyrosine kinase inhibition. Oncotarget 8, 109973 (2017).
Z.H. Shen, D.F. Zeng, X.Y. Wang, Y.Y. Ma, X. Zhang, and P.Y. Kong: Targeting of the leukemia microenvironment by c(RGDfV) overcomes the resistance to chemotherapy in acute myeloid leukemia in biomimetic polystyrene scaffolds. Oncol. Lett. 12, 3278 (2016).
T.M. Blanco, A. Mantalaris, A. Bismarck, and N. Panoskaltsis: The development of a three-dimensional scaffold for ex vivo biomimicry of human acute myeloid leukaemia. Biomaterials 31, 2243 (2010).
A.J. Favreau, C.P.H. Vary, P.C. Brooks, and P. Sathyanarayana: Cryptic collagen IV promotes cell migration and adhesion in myeloid leukemia. Cancer Med. 3, 265 (2014).
J.W. Shin and D.J. Mooney: Extracellular matrix stiffness causes systematic variations in proliferation and chemosensitivity in myeloid leuke-mias. Proc. Natl. Acad. Sci. USA 113, 12126 (2016).
T.T. Vu, C. Urn, and M. Lim: Characterization of leukemic cell behaviors in a soft marrow mimetic alginate hydrogel. J. Biomed. Mater. Res. B Appl. Biomater 100, 1980 (2012).
G.P. Gupta and J. Massagué: Cancer metastasis: building a framework. Cell 127, 679 (2006).
I.J. Fidler: The pathogenesis of cancer metastasis: the “seed and soil” hypothesis revisited. Nat Rev. Cancer 3, 453 (2003).
F. Macedo, K. Ladeira, F. Pinho, N. Saraiva, N. Bonito, L. Pinto, and F. Goncalves: Bone metastases: an overview. Oncol. Rev. 11, 321 (2017).
J. Massagué and A.C. Obenauf: Metastatic colonization by circulating tumour cells. Nature 529, 298 (2016).
C. Peitzsch, A. Tyutyunnykova, K. Pantel, and A. Dubrovska: Cancerstem cells: the root of tumor recurrence and metastases, Semin. Cancer Biol. 44, 10 (2017).
A.C. Obenauf and J. Massagué: Surviving at a distance: organ-specific metastasis. Trends. Cancer. 1, 76 (2015).
A. Chambers, A. Groom, and I. MacDonald: Dissemination and growth of cancer cells in metastatic sites. Nat. Rev. Cancer 2, 563a (2002).
G.D. Roodman and R. Silbermann: Mechanisms of osteolytic and osteoblastic skeletal lesions. Bonekey. Rep. 4, 1 (2015).
A.M. Sitarski, H. Fairfield, C. Falank, and M.R. Reagan: 3D tissue engineered in vitro models of cancer in bone. ACS BAGS Biomater Sci. Eng. 4, 324 (2017).
D.T. Butcher, T. Alliston, and V.M. Weaver: A tense situation: forcing tumour progression. Nat Rev. Cancer 9, 108 (2009).
Y. Kang, P.M. Siegel, W. Shu, M. Drobnjak, S.M. Kakonen, C. Cordón-Cardo, T.A. Guise, and J. Massagué: A multigenic program mediating breast cancer metastasis to bone. Cancer Cell 3, 537 (2003).
Y. Shiozawa, E.A. Pedersen, A.M. Havens, Y. Jung, A. Mishra, J. Joseph, J.K. Kim, L.R. Patel, C. Ying, A.M. Ziegler, M.J. Pienta, J. Song, J. Wang, R.D. Loberg, P.H. Krebsbach, K.J. Pienta, and R.S. Taichman: Human prostate cancer metastases target the hematopoietic stem cell niche to establish footholds in mouse bone marrow. J. Clin. Invest. 121, 1298 (2011).
J. Insua-Rodrfguez, and T. Oskarsson: The extracellular matrix in breast cancer. Adv. Drug Del. Rev. 97, 41 (2016).
S. Nath and G.R. Devi: Three-dimensional culture systems in cancer research: focus on tumor spheroid model. Pharmacol. Ther. 163, 94 (2016).
X. Xu, M.C. Farach-Carson, and X. Jia: Three-dimensional in vitro tumor models for cancer research and drug evaluation. Biotechnol. Adv. 32, 1256 (2014).
T. Pan, E.L. Fong, M. Martinez, D.A. Harrington, S.-H. Lin, M. C. Farach-Carson, and R.L. Satcher: Three-dimensional (3D) culture of bone-derived human 786-0 renal cell carcinoma retains relevant clinical characteristics of bone metastases. Cancer Lett. 365, 89 (2015).
H. Kwon, H.J. Kim, W.L. Rice, B. Subramanian, S.H. Park, I. Georgakoudi, and D.L. Kaplan: Development of an in vitro model to study the impact of BMP-2 on metastasis to bone. J. Tissue Eng. Regen. Med. 4, 590 (2010).
R.F. Cox, A. Jenkinson, K. Pohl, F.J. O’Brien, and M.P. Morgan: Osteomimicry of mammary adenocarcinoma cells in vitro; increased expression of bone matrix proteins and proliferation within a 3D collagen environment. PLoS ONE 7, e41679 (2012).
K.A. Fitzgerald, J. Guo, R.M. Raftery, I.M. Castano, C.M. Curtin, M. Gooding, R. Darcy, F.J. O’Brien, and C.M. O’Driscoll: Nanoparticle-mediated siRNA delivery assessed in a 3D co-culture model simulating prostate cancer bone metastasis. Int. J. Pharm. 511, 1058 (2016).
R. Marlow and G. Dontu: Modeling the breast cancer bone metastatic niche in complex three-dimensional cocultures. In Mammary Stem Cells, Maria del Mar Vivanco, ed., Humana Press: New York, 2015; p. 213.
R. Dhurjati, V. Krishnan, LA. Shuman, A.M. Mastro, and E.A. Vogler: Metastatic breast cancer cells colonize and degrade three-dimensional osteoblastic tissue in vitro. Clin. Exp. Metastasis 25, 741 (2008).
V. Krishnan, E.A. Vogler, D.M. Sosnoski. and A.M. Mastro: In vitro mimics of bone remodeling and the vicious cycle of cancer in bone. J. Cell. Physiol. 229, 453 (2014).
S. Bersini, J.S. Jeon, G. Dubini, C. Arrigoni, S. Chung, J.L. Charest, M. Moretti, and R.D. Kamm: A microfluidic 3D in vitro model for specificity of breast cancer metastasis to bone. Biomaterials 35, 2454 (2014).
T. Campbell, C. Williams, O. Ivanova, and B. Garrett: Could 3D printing change the world. Technologies, Potential, and Implications of Additive Manufacturing, Atlantic Council, Washington, DC (2011).
S. Patra and V. Young: A review of 3D printing techniques and the future in biofabrication of bioprinted tissue. Cell Biochem. Biophys. 74, 93 (2016).
C. Arrigoni, M. Gilardi, S. Bersini, C. Candrian, and M. Moretti: Bioprinting and organ-on-chip applications towards personalized medicine for bone diseases. Stem Cell Rev. 13, 407 (2017).
J.P. Temple, D.L. Hutton, B.P. Hung, P.Y. Huri, C.A. Cook, R. Kondragunta, X. Jia, and W.L. Grayson: Engineering anatomically shaped vascularized bone grafts with hASCs and 3D-printed PCL scaffolds. J. Biomed. Mater. Res. A 102, 4317 (2014).
H.N. Chia and B.M. Wu: Recent advances in 3D printing of biomaterials. J. Biol. Eng. 9, 4 (2015).
J. Groll, T. Boland, T. Blunk, J.A. Burdick, D.-W. Cho, P.D. Dalton, B. Derby, G. Forgacs, Q. Li, and V.A. Mironov: Biofabrication: reappraising the definition of an evolving field. Biofabrication. 8, 013001 (2016).
G. Gao, A.F. Schilling, T. Yonezawa, J. Wang, G. Dai, and X. Cui: Bioactive nanoparticles stimulate bone tissue formation in bioprinted three-dimensional scaffold and human mesenchymal stem cells. Biotechnol. J. 9, 1304 (2014).
S. Catros, J.-C. Fricain, B. Guillotin, B. Pippenger, R. Bareille, M. Remy, E. Lebraud, B. Desbat, J. Amédée, and F. Guillemot: Laser-assisted bioprinting for creating on-demand patterns of human osteoprogenitor cells and nano-hydroxyapatite. Biofabrication. 3, 025001 (2011).
C-H. Chang, C.-Y. Lin, F.-H. Liu, M.H.-C. Chen, C.-P. Lin, H.-N. Ho, and Y.-S. Liao: 3D printing bioceramic porous scaffolds with good mechanical property and cell affinity. PLoS CNE 10, e0143713 (2015).
S. Wiist, M.E. Godla, R. Müller, and S. Hofmann: Tunable hydrogel composite with two-step processing in combination with innovative hardware upgrade for cell-based three-dimensional bioprinting. Acta Biomater. 10, 630 (2014).
K.-S. Hwang, J.-W. Choi, J.-H. Kim, H.Y. Chung, S. Jin, J.-H. Shim, W.-S. Yun, C.-M. Jeong, and J.-B. Huh: Comparative efficacies of collagen-based 3D printed PCL/PLGA/β-TCP composite block bone grafts and biphasic calcium phosphate bone substitute for bone regeneration. Materials (Basel) 10, 421 (2017).
R. Alluri, A. Jakus, S. Bougioukli, W. Pannell, O. Sugiyama, A. Tang, R. Shah, and J.R. Lieberman: 3D printed hyperelastic “bone” scaffolds and regional gene therapy: a novel approach to bone healing. J. Biomed. Mater. Res. A 106, 1104 (2018).
W. Zhang, Q. Lian, D. Li, K. Wang, D. Hao, W. Bian, J. He, and Z. Jin: Cartilage repair and subchondral bone migration using 3D printing osteochondral composites: a one-year-period study in rabbit trochlea. BioMed Res. Int. 2014, 1 (2014).
W. Zhu, C. Xu, B.-P. Ma, Z.-B. Zheng, Y.-L Li, Q. Ma, G.-L. Wu, and X.-S. Weng: Three-dimensional printed scaffolds with gelatin and platelets enhance in vitro preosteoblast growth behavior and the sustained-release effect of growth factors. Chin. Med. J. 129, 2576 (2016).
S.V. Murphy and A. Atala: 3D bioprinting of tissues and organs. Nat. Biotechnol. 32, 773 (2014).
S. Adepu, N. Dhiman, A. Laha, C.S. Sharma, S. Ramakrishna, and M. Khandelwal: Three-dimensional bioprinting for bone tissue regeneration. Curr. Opin. Biomed. Eng. 2, 22 (2017).
W. Peng, D. Unutmaz, and I.T. Ozbolat: Bioprinting towards physiologically relevant tissue models for pharmaceutics. Trends Biotechnol. 34, 722 (2016).
P.S. Gungor-Ozkerim, I. Inci, Y.S. Zhang, A. Khademhosseini, and M.R. Dokmeci: Bioinks for 3D bioprinting: an overview. Biomater. Sci 6, 915 (2018).
H. Cui, W. Zhu, M. Nowicki, X. Zhou, A. Khademhosseini, and L.G. Zhang: Hierarchical fabrication of engineered vascularized bone biphasic constructs via dual 3D bioprinting: integrating regional bioac-tive factors into architectural design. Adv. Healthc. Mater. 5, 2174 (2016).
M. Hospodiuk, M. Dey, D. Sosnoski, and I.T. Ozbolat: The bioink:acom-prehensive review on bioprintable materials. Biotechnol. Adv. 35, 217 (2017).
T. Jungst, W. Smolan, K. Schacht, T. Scheibel, and J. Groll: Strategies and molecular design criteria for 3D printable hydrogels. Chem. Rev. 116, 1496 (2016).
H.W. Kang, S.J. Lee, I.K. Ko, C. Kengla, J.J. Yoo, and A. Atala: A 3D bioprinting system to produce human-scale tissue constructs with structural integrity. Nat. Biotechnol. 34, 312 (2016).
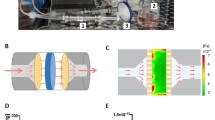
W. Liu, Y.S. Zhang, M.A. Heinrich, F. De Ferrari, H.I. Jang, S.M. Bakht, M.M. Alvarez, J. Yang, Y.-C. Li, G. Trujillo-de Santiago, A.K. Miri, K. Zhu, P. Khoshakhlagh, G. Prakash, H. Cheng, X. Guan, Z. Zhong, J. Ju, G.H. Zhu, X. Jin, S.R. Shin, M.R. Dokmeci, and A. Khademhosseini: Rapid continuous multimaterial extrusion bioprinting. Adv. Mater. 29, 1604630 (2017).
X. Zhou, N.J. Castro, W. Zhu, H. Cui, M. Aliabouzar, K. Sarkar, and L.G. Zhang: Improved human bone marrow mesenchymal stem cell osteogenesis in 3D bioprinted tissue scaffolds with low intensity pulsed ultrasound stimulation. Sci. Rep. 6, 1 (2016).
M.V. Braham, T. Ahlfeld, A.R. Akkineni, M.C. Minnema, W.J. Dhert, F.C. Oner, C. Robin, A. Lode, M. Gelinsky, and J. Alblas: Endosteal and perivascular subniches in a 3D bone marrow model for multiple myeloma. Tissue Eng. Part C. Methods 24, 300 (2018).
Acknowledgments
We thank the publishers Elsevier, Taylor and Francis Ltd., BioMed Central, Springer Nature, John Wiley and Sons for the permission to reprint published data shown in Figs. 3(a)[47], 3 (b)[49], 3(c)[50], Figs. 4(a), 4(b)[124], 4(c)[121], 4(d), 4(e)[125]. This project has received funding from the European Research Council (ERC) under the European Union’ s Horizon 2020 research and innovation programme (grant agreement No 757490). C.L.-T. and A.R. acknowledge funding from the BMBFNanoMatFutur programme (FKZ 13N12968)andthepro-gramme BioInterfaces in Technology and Medicine (BIFTM) by the Helmholtz Association.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Raic, A., Naolou, T., Mohra, A. et al. 3D models of the bone marrow in health and disease: yesterday, today, and tomorrow. MRS Communications 9, 37–52 (2019). https://doi.org/10.1557/mrc.2018.203
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1557/mrc.2018.203