Dear Editor,
Case Presentation
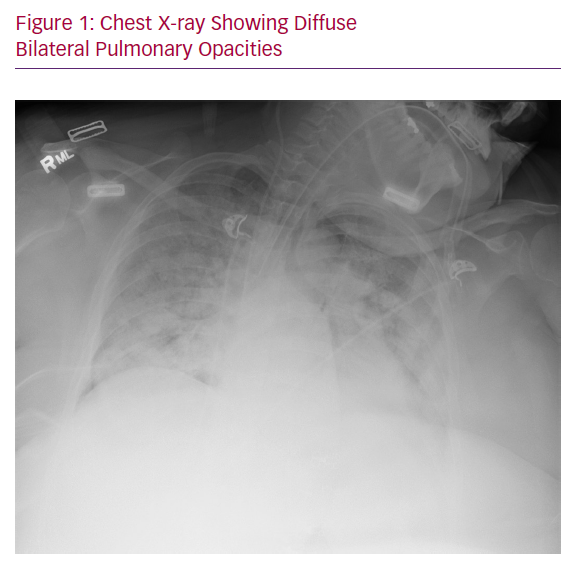
A 50-year old female presented to the emergency department with a 6-day history of fever, progressively worsening cough and shortness of breath. The patient did not report any contact with anyone who had been recently unwell or had been travelling. Upon arrival to the emergency room, the patient was noted to be severely hypoxaemic by pulse oximetry (66%) and in impeding respiratory failure, so she was emergently intubated for mechanical ventilatory support. Immediately post-intubation, arterial blood gas was as follows: pH 7.34, pCO2 31 mmHg, pO2 60 mmHg, O2 saturation 90%, calculated HCO3 16 mmol/l on FiO2 of 100% and PaO2/FIO2 ratio of 60. Her ventilatory mode was set at controlled minute ventilation, with a respiratory rate of 24, tidal volume of 300 cc (6 cc/ideal body weight), positive end-expiratory pressure (PEEP) of 20 cmH2O and FiO2 of 100%. The patient’s chest X-ray at the time of admission showed diffuse bilateral pulmonary opacities consistent with multifocal pneumonia or pulmonary oedema (Figure 1). Polymerase chain reaction (PCR) testing for severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) was sent and came back positive after 48 hours.
The patient was diagnosed with severe acute respiratory distress syndrome (ARDS), so was treated with inhaled pulmonary vasodilators, neuromuscular blockade and prone-position ventilation. In addition, she was evaluated for extracorporeal membrane oxygenation (ECMO) support. Her respiratory ECMO survival prediction score was 5, which classified her as risk class II, with an expected in-hospital survival of 76%. Cardiac biomarkers of brain natriuretic peptide (BNP) and troponin were 150 pg/ml and w0.26 ng/ml, respectively, on admission. Therefore, the critical care team deemed that the patient would benefit from ECMO. However, her underlying cardiovascular comorbidities raised concerns, such as the evaluation of volume status, cardiac function, lung and pleura evaluation, reassessment of lung recruitment with high PEEP and decision-making with regard to ECMO support. Furthermore, the results of the SARS–CoV2 test were still pending, thus the exact aetiology of her ARDS remained unclear.
Medical History
Her medical history was significant for morbid obesity (BMI of 54), type 2 diabetes, hypertension, non-alcoholic steatohepatitis, bipolar disorder and anxiety.
Our current diagnostic options for COVID-19 suspected/confirmed patients include supine transthoracic echocardiography, supine transthoracic echocardiography, prone transthoracic echocardiography and prone transoesophageal echocardiography. Forty-eight hours after initial presentation, the patient’s PCR testing for SARS-CoV-2 returned positive, confirming the diagnosis of COVID-19.
Diagnosis and Treatment
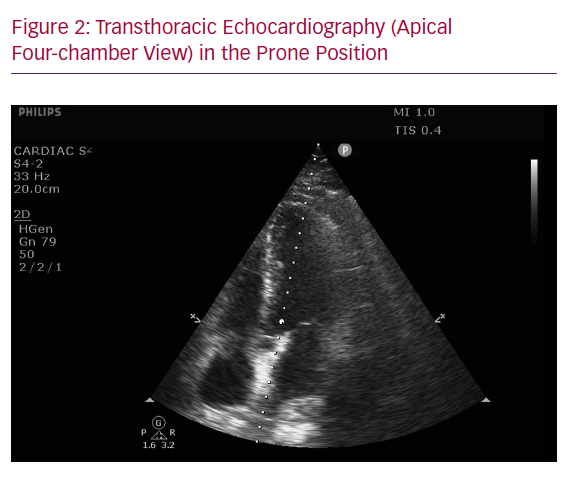
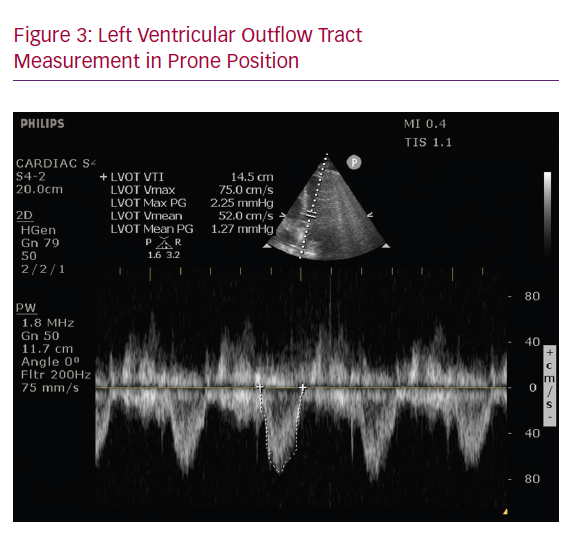
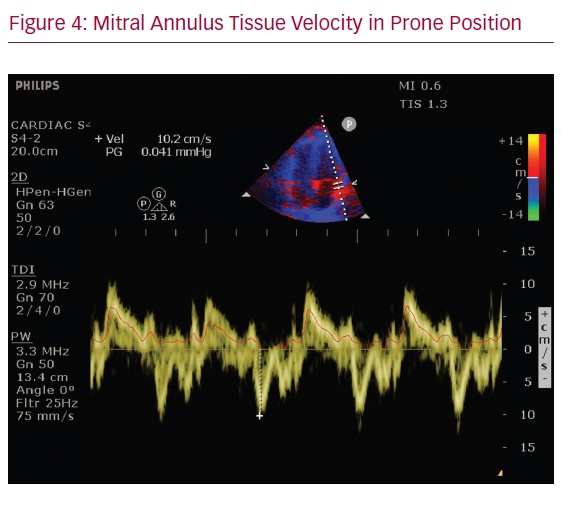
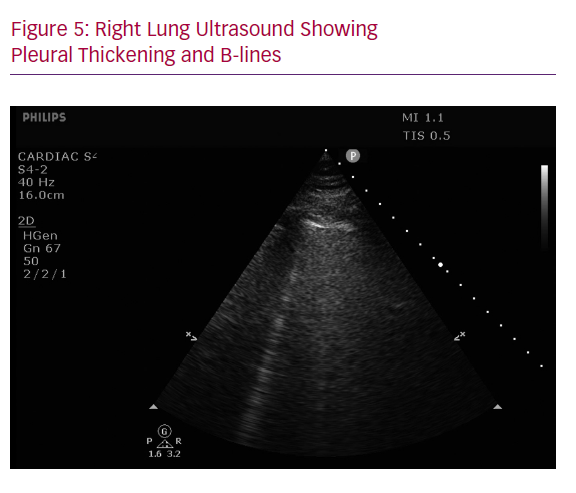
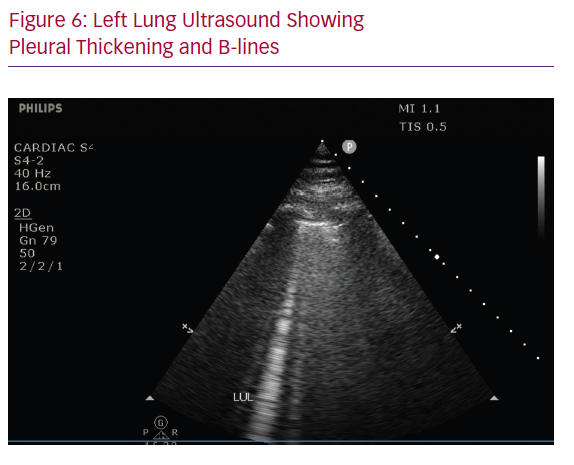
The key to the correct diagnosis, monitoring and management in this case of a patient presenting in severe acute hypoxic respiratory failure with multiple cardiac risk factors and elevated biomarkers is an appropriate utilisation of the point-of-care assessment of cardiopulmonary ultrasound. Transthoracic echocardiography (apical four-chamber view) in the prone position was performed and revealed normal right ventricular function by visual estimation (Figure 2). The left ventricular function appeared mildly decreased (estimated left ventricular ejection fraction 45–50%), which was also reflected in a left ventricular outflow tract velocity time integral of 14.5 cm and mitral annulus tissue velocity 10.2 cm/second (Figures 3 and 4). The lung ultrasonography findings included bilateral normal lung sliding, thickening of pleural lines, absence of pleural effusions and presence of 1–2 B-lines (Figures 5 and 6). The patient’s respiratory failure was not in proportion to the mild degree of left ventricular failure, and thus ARDS remained the most likely diagnosis. The decision was made to continue monitoring the patient’s clinical course with current medical therapy, and in the setting of further decompensation, transition to VV ECMO.
Lung ultrasonography has been utilised in evaluation of COVID-19 patients, and the characteristic findings have included thickening of the pleural line with pleural line irregularity; B lines in a variety of patterns, including multifocal and confluent; consolidations in a variety of patterns, including multifocal small, non-translobar and translobar with occasional mobile air bronchograms; appearance of A lines during recovery phase; and pleural effusions being uncommon.1 Our patient’s point of care (POC) lung ultrasonography demonstrated several of these features, making COVID-19 a probable aetiology of her ARDS. While lung ultrasonography may not be able to detect lesions deep in the lung parenchyma, the peripheral lung involvement noted in COVID-19 lends itself to ultrasonography evaluation.
Cardiogenic pulmonary oedema (CPE) is a known cause of acute respiratory failure (ARF). Although most frequently encountered in patients with reduced ejection fraction, CPE is increasingly attributed to heart failure with preserved ejection fraction, especially among patients with known cardiovascular risk factors.2 In patients with suspected ARDS, as in the case of our patient, it is important to rule out cardiac failure or acute fluid overload as the aetiology of ARF.3 POC echocardiography is ideally suited for evaluating intravascular fluid status, as well as cardiac function.4 However, prone-position ventilation (PPV) is often considered a hindrance in obtaining transthoracic cardiac ultrasound. While technically difficult, transthoracic echocardiogram in the prone position has been previously described.5 It is performed with the patient in the left prone position, with the left arm raised above the head. This technique allows for all apical views and for related measurements to be obtained. In the case of our patient, prone-position echocardiography was critical in establishing a non-cardiac cause of her ARF, and also helping decide the type of ECMO (VV versus VA).
Conclusion
Prone-position echocardiography is an extremely useful diagnostic modality in caring for ARDS patients undergoing PPV. In the hands of a trained operator, it can provide a reliable evaluation of biventricular function, valvular abnormalities and intravascular volume status. Especially in COVID-19 patients, where limiting the exposure of healthcare workers and the contamination of diagnostic equipment is important, prone-position echocardiography serves as a relatively quick, bedside and non-invasive diagnostic modality that can help guide time-sensitive clinical care. Characteristic pulmonary findings on POC ultrasound can help in the diagnosis of COVID-19 while awaiting confirmatory testing. Prone-position echocardiography is an extremely useful diagnostic modality in caring for ARDS patients undergoing prone-positioning ventilation.