-
PDF
- Split View
-
Views
-
Cite
Cite
Joel K. Durand, Monte S. Willis, Karl Landsteiner, MD: Transfusion Medicine, Laboratory Medicine, Volume 41, Issue 1, January 2010, Pages 53–55, https://doi.org/10.1309/LM0MICLH4GG3QNDC
Close - Share Icon Share
Karl Landsteiner (1868–1943)
Karl Landsteiner, born June 14, 1868, in Vienna, Austria, was the only child of Fanny Hess and Leopold Landsteiner. Even as a child, Dr. Landsteiner displayed an extraordinary aptitude for academics. Dr. Landsteiner completed primary school and the first part of secondary school before attending the Staatsgymnasium in Linz in 1880 as an honors student. Here he developed his burgeoning interest in mathematics and the natural sciences.1 He subsequently attended the University of Vienna, starting in 1885, where he studied under several of the prominent scientists in the fields of anatomy, zoology, hematological chemistry, and organic chemistry. His early experimental work in chemistry foretold of his subsequent interest and achievement in the field of serology. In 1891, Dr. Landsteiner completed his medical degree and began his work in the laboratory of the medical clinic where he studied multiple myeloma (cancer of the cells secreting antibodies). He spent the next 5 years in the laboratories of Hantzsch at Zurich, Emil Fischer at Wurzburg, and E. Bamberger at Munich, publishing on a number of topics investigating the interface between chemistry and biology by focusing on antigen–antibody reactions.2,3,4
In 1896, Dr. Landsteiner returned to Vienna to resume his studies at the Vienna General Hospital as assistant to Dr. Max von Gruber at the Institute of Hygiene at Vienna. Dr. Gruber was known for his discovery of the serological test for typhoid. Dr. Landsteiner was fascinated by the Gruber-Widal reaction, which provided evidence for the serological differentiation between typhoid and non-typhoid bacilli. He believed this differentiation reflected particular chemical differences between the bacilli recognized by antibodies. Under Dr. Gruber, Dr. Landsteiner’s interest in the mechanisms of immunity and in the nature of antibodies intensified, and Dr. Landsteiner published his first papers on agglutination and immunology.5 In the fall of 1897, he transferred to the Institute of Pathological Anatomy as assistant to the director, Professor Anton Weichselbaum. Here, he performed more than 3,639 post–mortems and published 75 articles over the next 10 years. Of the 75 manuscripts, 52 addressed serological issues, 23 were in microbiology, and 11 were in anatomical anatomy. It was during this time that Dr. Landsteiner performed his seminal work on the interactions between red cells and serum in different healthy individuals.
Dr. Landsteiner published his initial observations on the agglutination reactions occurring between the red blood cells and serum of different healthy individuals in 1900. This initial observation was no more than a footnote in his 1900 manuscript.6 He elaborated on this initial observation the following year in his manuscript entitled, “Agglutination of Normal Human Blood.”7 In the 1900 manuscript, Dr. Landsteiner’s footnote states that “the sera of healthy humans has an agglutinating effect, not only upon animal blood cells, but frequently upon blood cells from other individuals as well; the question is whether this phenomenon is due to inherent individual differences or to the effect of influenced damages, (eg, bacterial nature).”6,8 In a more detailed subsequent paper, Dr. Landsteiner observed sera and red cells from 22 healthy people, including himself and his colleagues.7 At the time, several parallel studies had investigated agglutination in sick patients, which likely represented antibody reactions to pathogens.9 Dr. Landsteiner’s studies were unique because they investigated antibody reactions between healthy individuals, making the case that distinct patterns of serum reactivity could be identified. He proposed that these reactions, which he classified by group, could be used as a basis for transfusing blood based on serological compatibility.
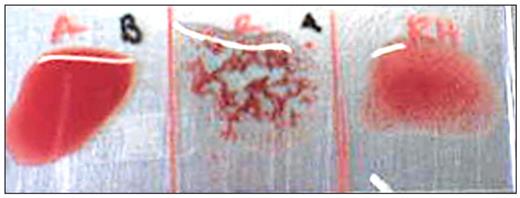
Using methodologies still in use today in transfusion medicine laboratories, serum was tested against red cells to identify agglutination (Table 1, Image 1). What is immediately evident in these studies is that a patient’s serum does not react against his of her own cells, and that the reactivity of groups of patients (Patient 3 and Patient 4, for example in Table 1) follows specific patterns. Dr. Landsteiner observed that “the sera in most cases could be separated into 3 groups.” The serum of group A reacts with the red blood cells of group B but not with those of group A. On the other hand, the red cells of group A are agglutinated in the same way by the serum of group B. The red cells of the third group, C, are not affected by the sera from groups A, B, or C, but the serum of group C agglutinates red cells of groups A and B. Naturally, Dr. Landsteiner concluded that red blood cells are inert to the serum agglutinins (antibodies) from the same patient.7 He recognized 2 antigens (agglutinogens A and B) and 2 antibodies (agglutinins and anti-A, anti-B) which would explain the 3 groups he identified, the third group lacking A or B antigens. The following year, Dr. Landsteiner’s pupil identified patient red blood cells that reacted with both anti-A and anti-B (now known as the much rarer AB blood type).10 Patients with sera containing both anti-A and anti-B were identified as group C until 1911, when von Dungen and Hirzfeld first used the term O.11 They also used AB to describe the group of red blood cells reacting with anti–A and anti–B, which was designated as “no particular type” by von Decastello and Sturli years earlier. Jansky (1907) and Moss (1910) classified the blood groups (A, B, AB, O) as I, II, III, and IV.12,13 While groups II and III were the same, I and IV were reversed causing confusion. This lead to the Health Committee of the League of Nations to recommend the A, B, AB, and O classification, which gradually came into common use.14 This became the Landsteiner nomenclature, in honor of the man who discovered the blood groups, and is the classification used today.
Although Dr. Landsteiner described the ABO blood grouping in 1901, its practical application to prevent major incompatibility reactions was not realized for several years.15–17 Blood typing to match blood was first reported by Ottenberg in 1907. However, it was not until citrate anticoagulant (citric acid) was developed to prevent clotting in 1914–1915 that the use of transfusions became routine therapy in medicine, just in time for World War I.18
Hapten: A small molecule that enables the elicitation of an immune response to the attached larger carrier (generally a protein). Many haptens are modifications of biological proteins due to chemical reactions. Examples include the rare penicillin and hydrazaline induction of autoimmune disease (hemolytic anemia and lupus, respectively).
Agglutination of Sera and Red Cell in Apparently Healthy Men
| Sera . | Blood Corpuscles . | |||||
|---|---|---|---|---|---|---|
| Patient 1¶ . | Patient 2* . | Patient 3§ . | Patient 4§ . | Patient 5* . | Patient 6¶ . | |
| Patient 1 | − | + | + | + | + | − |
| Patient 2 | − | − | + | + | − | − |
| Patient 3 | − | + | − | − | + | − |
| Patient 4 | − | + | − | − | + | − |
| Patient 5 | − | − | + | + | − | − |
| Patient 6 | − | + | + | + | + | − |
| Sera . | Blood Corpuscles . | |||||
|---|---|---|---|---|---|---|
| Patient 1¶ . | Patient 2* . | Patient 3§ . | Patient 4§ . | Patient 5* . | Patient 6¶ . | |
| Patient 1 | − | + | + | + | + | − |
| Patient 2 | − | − | + | + | − | − |
| Patient 3 | − | + | − | − | + | − |
| Patient 4 | − | + | − | − | + | − |
| Patient 5 | − | − | + | + | − | − |
| Patient 6 | − | + | + | + | + | − |
Adapted from Landsteiner, 1901.7
*, §, ¶Matching patterns.
Agglutination of Sera and Red Cell in Apparently Healthy Men
| Sera . | Blood Corpuscles . | |||||
|---|---|---|---|---|---|---|
| Patient 1¶ . | Patient 2* . | Patient 3§ . | Patient 4§ . | Patient 5* . | Patient 6¶ . | |
| Patient 1 | − | + | + | + | + | − |
| Patient 2 | − | − | + | + | − | − |
| Patient 3 | − | + | − | − | + | − |
| Patient 4 | − | + | − | − | + | − |
| Patient 5 | − | − | + | + | − | − |
| Patient 6 | − | + | + | + | + | − |
| Sera . | Blood Corpuscles . | |||||
|---|---|---|---|---|---|---|
| Patient 1¶ . | Patient 2* . | Patient 3§ . | Patient 4§ . | Patient 5* . | Patient 6¶ . | |
| Patient 1 | − | + | + | + | + | − |
| Patient 2 | − | − | + | + | − | − |
| Patient 3 | − | + | − | − | + | − |
| Patient 4 | − | + | − | − | + | − |
| Patient 5 | − | − | + | + | − | − |
| Patient 6 | − | + | + | + | + | − |
Adapted from Landsteiner, 1901.7
*, §, ¶Matching patterns.
In 1908, Dr. Landsteiner was appointed the Head of the Prosectorate of the Imperial Wilhelminen Hospital in Vienna. In 1916 he married Helen Wlasto; their only son, Ernest Karl Landsteiner, was born on April 8, 1917, and later became a distinguished surgeon in Providence, RI.19 By 1919, amid the financial and social crisis following the Austro–Hungarian monarchy collapse and World War I, Vienna had become a difficult place for Dr. Landsteiner to continue his work. Unable to see a future in Austria, he moved to Holland and found work as a prosector at the Catholic R.K. Hospital in Den Haag. From 1919 through 1922, he published 12 manuscripts on novel haptens he had discovered, on conjugates with proteins which were capable of inducing anaphylaxis, and on the serological specificity of the hemoglobin of different species of animals. In 1923, Dr. Landsteiner took a position at the Rockefeller Institute for Medical Research in New York. Dr. Landsteiner continued his serological work describing additional blood groups including M, N, and P, which were initially applied to paternity identification and criminal cases.20 Dr. Landsteiner was awarded the Nobel Prize for Medicine on December 10, 1930, for his discovery of the human blood groups published in 1901.
Agglutination: The clumping of bacteria, red blood cells (see insert, middle panel), or other cells due to the introduction of an antibody which recognizes specific antigens. (Panel from: Public Domain, http://en.wikipedia.org/wiki/File:RhB-.JPG)
Dr. Landsteiner became an emeritus professor at the Rockefeller Institute, officially retiring in 1939 at the age of 71, but he continued working. In collaboration with Philip Levine and Alexander Wiener, he continued to discover additional, medically relevant blood groups. In 1940, Dr. Landsteiner identified another important blood group used in transfusion medicine: the Rh factor.21 Despite matching blood groups for A, B, and O, occasional transfusion incompatibilities still occurred at this time. The discovery of the Rh factor, either as positive (+) or negative (−), completed the blood grouping strategy which transfusions are based on today (eg, A+, O+, AB−). The eventual application of giving transfusions with matched Rh factor typing reduced transfusion incompatibilities and reactions. The discovery of the Rh factors also led to the understanding of etiology of hemolytic disease of the newborn, which can occur when an Rh-mother has a second Rh+ baby.22
Dr. Landsteiner’s later life was focused on his concern for his wife, who suffered from thyroid cancer. He changed his research focus to malignant tumors in the hopes of helping his wife.19 At the age of 75 he had a heart attack in his laboratory in the Rockefeller Institute and died two days later on June 26, 1943. Dr. Landsteiner’s work extended far beyond his serological work with ABO blood grouping (Table 2). However, his discovery of ABO blood groups that made safe blood transfusions possible clearly makes him one of the great luminaries in laboratory medicine.
Dr Landsteiner’s Major Contributions to Laboratory Medicine and Science
| Discovered the major blood groups (1901). |
| Discovered that the pathogenesis of paroxysmal nocturnal hematuria is caused by cold–antibodies (with Donath, 1904). |
| Introduced dark-field microscopy for the detection of T. pallidum to diagnose syphilis (1906). |
| Successfully infected monkeys with syphilis, making experimentation with syphilis possible (1905–1906). |
| Elucidated the previously unknown mechanism occurring in the Wassermann reaction, the test which detected syphilis by agglutination of antibodies that reacted with phospholipids (anti–phospholipid antibodies) (1907). |
| Determined the etiology of poliomyelitis by injecting a homogenate of brain and spinal cord of an affected individual (at autopsy) into the abdominal cavity of monkeys which subsequently demonstrated signs of paralysis like polio patients (1908). |
| Demonstrated proof that the pathogenic agent of poliomyelitis is a virus of very small size (1910). |
| Began his investigation of haptens (see text box), which are responsible for numerous allergic and autoimmune responses involved in clinically relevant pathophysiolgoic processes (see suggested reading for more information) (1921). |
| Discovered the major blood groups (1901). |
| Discovered that the pathogenesis of paroxysmal nocturnal hematuria is caused by cold–antibodies (with Donath, 1904). |
| Introduced dark-field microscopy for the detection of T. pallidum to diagnose syphilis (1906). |
| Successfully infected monkeys with syphilis, making experimentation with syphilis possible (1905–1906). |
| Elucidated the previously unknown mechanism occurring in the Wassermann reaction, the test which detected syphilis by agglutination of antibodies that reacted with phospholipids (anti–phospholipid antibodies) (1907). |
| Determined the etiology of poliomyelitis by injecting a homogenate of brain and spinal cord of an affected individual (at autopsy) into the abdominal cavity of monkeys which subsequently demonstrated signs of paralysis like polio patients (1908). |
| Demonstrated proof that the pathogenic agent of poliomyelitis is a virus of very small size (1910). |
| Began his investigation of haptens (see text box), which are responsible for numerous allergic and autoimmune responses involved in clinically relevant pathophysiolgoic processes (see suggested reading for more information) (1921). |
Dr Landsteiner’s Major Contributions to Laboratory Medicine and Science
| Discovered the major blood groups (1901). |
| Discovered that the pathogenesis of paroxysmal nocturnal hematuria is caused by cold–antibodies (with Donath, 1904). |
| Introduced dark-field microscopy for the detection of T. pallidum to diagnose syphilis (1906). |
| Successfully infected monkeys with syphilis, making experimentation with syphilis possible (1905–1906). |
| Elucidated the previously unknown mechanism occurring in the Wassermann reaction, the test which detected syphilis by agglutination of antibodies that reacted with phospholipids (anti–phospholipid antibodies) (1907). |
| Determined the etiology of poliomyelitis by injecting a homogenate of brain and spinal cord of an affected individual (at autopsy) into the abdominal cavity of monkeys which subsequently demonstrated signs of paralysis like polio patients (1908). |
| Demonstrated proof that the pathogenic agent of poliomyelitis is a virus of very small size (1910). |
| Began his investigation of haptens (see text box), which are responsible for numerous allergic and autoimmune responses involved in clinically relevant pathophysiolgoic processes (see suggested reading for more information) (1921). |
| Discovered the major blood groups (1901). |
| Discovered that the pathogenesis of paroxysmal nocturnal hematuria is caused by cold–antibodies (with Donath, 1904). |
| Introduced dark-field microscopy for the detection of T. pallidum to diagnose syphilis (1906). |
| Successfully infected monkeys with syphilis, making experimentation with syphilis possible (1905–1906). |
| Elucidated the previously unknown mechanism occurring in the Wassermann reaction, the test which detected syphilis by agglutination of antibodies that reacted with phospholipids (anti–phospholipid antibodies) (1907). |
| Determined the etiology of poliomyelitis by injecting a homogenate of brain and spinal cord of an affected individual (at autopsy) into the abdominal cavity of monkeys which subsequently demonstrated signs of paralysis like polio patients (1908). |
| Demonstrated proof that the pathogenic agent of poliomyelitis is a virus of very small size (1910). |
| Began his investigation of haptens (see text box), which are responsible for numerous allergic and autoimmune responses involved in clinically relevant pathophysiolgoic processes (see suggested reading for more information) (1921). |
Suggested Reading
Mazumdar PMH. Species and Specificity: An Interpretation of the History of Immunology. New York: Cambridge University Press; 1995.
References