Published online Aug 26, 2020. doi: 10.12998/wjcc.v8.i16.3560
Peer-review started: April 21, 2020
First decision: May 21, 2020
Revised: June 2, 2020
Accepted: July 22, 2020
Article in press: July 22, 2020
Published online: August 26, 2020
D-dimer, a soluble degradation product of cross-linked fibrin, is commonly used as an important marker for the diagnosis of disseminated intravascular coagulation and differential diagnosis of thrombosis. Herein, we present a geriatric case with an unusually elevated D-dimer level.
An 82-year-old woman, admitted to the ward with a diagnosis of chronic heart failure, was noted to have a remarkably elevated D-dimer level, beyond the qualified range (> 100 mg/L), utilizing the Innovating D-dimer for Sysmex CS-5100 System™. However, no evidence, including clinical symptoms, radiographic evidence of thromboembolic disease, and parallel fibrinogen degradation product values, suggested that this patient was at high risk of thrombopenia. To confirm the discrepancy, a series of approaches including sample dilution, re-analysis via alternative methods, and sample treatment with blockage of specific heterophilic antibodies were performed. A remarkable disappearance of the elevated D-dimer values was observed in the samples after they were subjected to these approaches (4.49, 9.42, 9.06, and 12.58 mg/L, respectively). This confirmed the presence of heterophilic antibodies in this case. In addition, a reduction in cardiac output due to the presence of cardiac failure could also be responsible for the existence of a hypercoagulable state in this case.
In conclusion, the presence of heterophilic antibodies should be considered when an elevated D-dimer value is not in conformity with the clinical evidence, and a viral infection should be considered when interference by a heterophilic antibody exists.
Core tip: Heterophilic antibodies should be considered while elevated D-dimer value is not in conformity with clinical evidence. We will keep on doing subsequent serial monitoring of D-dimer values with anti-virus therapy and more research needs to be done to verify the exact fragment to improve the D-dimer test in the near future.
- Citation: Sun HX, Ge H, Xu ZQ, Sheng HM. Clinical laboratory investigation of a patient with an extremely high D-dimer level: A case report. World J Clin Cases 2020; 8(16): 3560-3566
- URL: https://www.wjgnet.com/2307-8960/full/v8/i16/3560.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v8.i16.3560
D-dimer, a soluble degradation product of cross-linked fibrin, is commonly used for the diagnosis of disseminated intravascular coagulation and thromboembolic diseases, such as deep vein thrombosis (DVT) and pulmonary embolism (PE). In comparison with other assays that have adopted methods such as whole-blood agglutination assays and enzyme-linked immunosorbent assays, immunofluorescence or latex agglutination assays have become the mostly widely used methods for the examination of D-dimers, as they combine the advantages of convenience and relatively high sensitivity and specificity[1]. The methodology of immunofluorescence has been optimized and established as the gold standard for D-dimer testing. However, it has been suggested by numerous researchers that heterophilic antibodies could interfere with the interpretation of D-dimer testing. In addition, other factors could also interfere with the results of coagulation tests, such as cardiac failure, infections, and usage of anti-coagulant drugs.
Heterophilic antibody is a substantial player among the factors interfering with the determination of the absolute value of D-dimer levels. Herein, we report a case with an extremely elevated level of D-dimers but with no relevant symptoms related to thrombosis. We concluded that the D-dimer test results were due to her cardiac factors and interference from her heterophilic antibodies against Epstein-Barr virus (EBV).
An 82-year-old woman complaining of weakness, dyspnoea, and chest tightness was admitted to the Department of General Practice of our hospital.
Physical examination revealed an elderly woman without agitation. Her lungs were clear without moist crackles on auscultation. Her cardiac rhythm was also regular, with a heart rate of 65beats per minute. There was no oedema in her lower limbs.
To exclude the possibility of pulmonary embolism (PE), her levels of fibrinogen degradation product (FDP) and D-dimers were tested. However, her level of D-dimers was remarkably elevated in comparison to the qualified range (> 100 mg/L; reference interval: < 0.55 mg/L) while her level of FDP was elevated only slightly at 10.4 μg/mL (reference interval: 0–5).
In our laboratory, the D-dimer parameter was evaluated on citrated plasma samples utilizing the Innovance D-dimer for Sysmex CS-5100 System (Siemens Healthcare Diagnostics, Erlangen, Germany), a particle-enhanced, immunoturbidometric assay with a sensitivity and specificity of 97% and 91%, respectively[2]. Her D-dimer test was repeated in the following 2 wk, and the extremely high value was (> 100 mg/L) consistently present using the same testing method, excluding analytical errors such as inaccurate pipetting, washing insufficiency, tracer aggregation, or other contamination[3]. She also continued to have an only modestly elevated FDP.
We investigated the cause of the remarkable results of her D-dimer test. Further imaging workup including chest computed tomography (CT) and contrast-enhanced CT pulmonary angiography was performed; however, the results did not show any obvious abnormality. Duplex ultrasound of the lower limbs was also conducted to rule out the existence of potential deep vein thrombosis (DVT), along with a large panel of laboratory tests including homocysteine, lupus anticoagulant, and anticardiolipin, but the results of these laboratory and imaging tests were all negative.
She was diagnosed with chronic heart failure.
She was treated with diuretics and angiotensin receptor enzymes. However, the value of her D-dimers always remained far above the diagnostic threshold for venous thrombosis or pulmonary embolism.
Four days after admission, her chest tightness was alleviated and her BNP value turned out to be normal after the diagnosis of chronic plus acute heart failure was established.
Patient characteristics and disorders, such as ageing; pregnancy; a recent injury, surgery, or trauma; sepsis; cancer; and some liver or renal diseases[1] are also associated with increased levels of D-dimers. To exclude effects originating from any of these comorbidities, we confirmed her medical history and performed a series of serum tests. The results of all tests were within the normal reference range, taking into account her age and sex, and her relevant medical history was negative (Table 1).
| Patient results | Reference range | ||
| At admission (June 11) | Follow-up (June 15-26) | ||
| Leucocytes (× 109/L) | 8.28 | 7.16 | 3.5-9.5 |
| Red blood cells (× 1012/L) | 4.08 | 3.77 | 3.8-5.1 |
| Haemoglobin (g/L) | 119 | 108 | 115-1 |
| Haematocrit | 0.37 | 0.34 | 0.35-0.45 |
| Platelets (× 109/L) | 237 | 293 | 125-350 |
| Prothrombin time (s) | 11.6 | 13.2 | 9-13 |
| Prothrombin time (INR) | 1.01 | 1.16 | — |
| Activate partial thromboplastin time (s) | 27.3 | 31.7 | 20-40 |
| Thrombin time (seconds) | 16.2 | 19.6 | 14-21 |
| Fibrinogen (g/L) | 3.4 | 4 | 2-4 |
| Fibrinogen degradation product (µg/mL) | 9.29 | 5.7 | 0-5 |
| D-dimer (mg/L) | > 100 | > 100 | < 0.55 |
| Antithrombin-III (%) | 91 | 94 | 83-128 |
| Creatine kinase-MB (ng/mL) | 0.63 | ND | 0-5 |
| Myoglobin (ng/mL) | 50.44 | ND | 0-110 |
| Cardiac troponin-I (ng/mL) | 0.017 | ND | 0-0.04 |
| B-type natriuretic peptide (pg/mL) | 321.48 | 73.83 | 0-100 |
| C-reactive protein (mg/L) | 13 | 6.9 | 0-5 |
| Triiodothyronine (nmol/L) | 1.05 | ND | 0.92-2.79 |
| Thyroxine (nmol/L) | 93.46 | ND | 55.3-160.8 |
| Free triiodothyronine (pmol/L) | 3.46 | ND | 3.5-6.5 |
| Free thyroxine (pmol/L) | 18.63 | ND | 11.5-22.7 |
| Thyroid-stimulating hormone (µIU/mL) | 2.688 | ND | 0.55-4.78 |
| Human chorionic gonadotropin (mIU/mL) | 2.18 | ND | 0-10 |
| Squamous cell carcinoma antigen (ng/mL) | 1.1 | ND | 0-1.5 |
| Alpha-fetoprotein (ng/mL) | 6.37 | ND | 0-8.1 |
| Carcinoembryonic antigen (ng/mL) | 1.33 | ND | 0-5 |
| Carbohydrate antigen 50 (IU/mL) | 4.63 | ND | 0-25 |
| Carbohydrate antigen 242 (IU/mL) | 1.35 | ND | 0-20 |
| Carbohydrate antigen 19-9 (U/mL) | 17.77 | ND | 0-37 |
| Carbohydrate antigen 125 (U/mL) | 6.14 | ND | 0-35 |
| Carbohydrate antigen 15-3 (U/mL) | 5.09 | ND | 0-32.4 |
| Carbohydrate antigen 72-4 (U/mL) | 4.01 | ND | 0-8.2 |
| Immunoglobulin A(g/L) | ND | 2.83 | 0.7-4 |
| Immunoglobulin G(g/L) | ND | 12.9 | 7-16 |
| Immunoglobulin M(g/L) | ND | 0.62 | 0.4-2.3 |
| Immunoglobulin E(IU/mL) | ND | 19.1 | < 100 |
| Anti-streptolysin O (IU/mL) | ND | 50 | 0-408 |
| Rheumatoid factor (IU/mL) | ND | 12.5 | 0-15.9 |
| Anti-cyclic citrullinated peptide antibodies (U/mL) | ND | 7 | 0-17 |
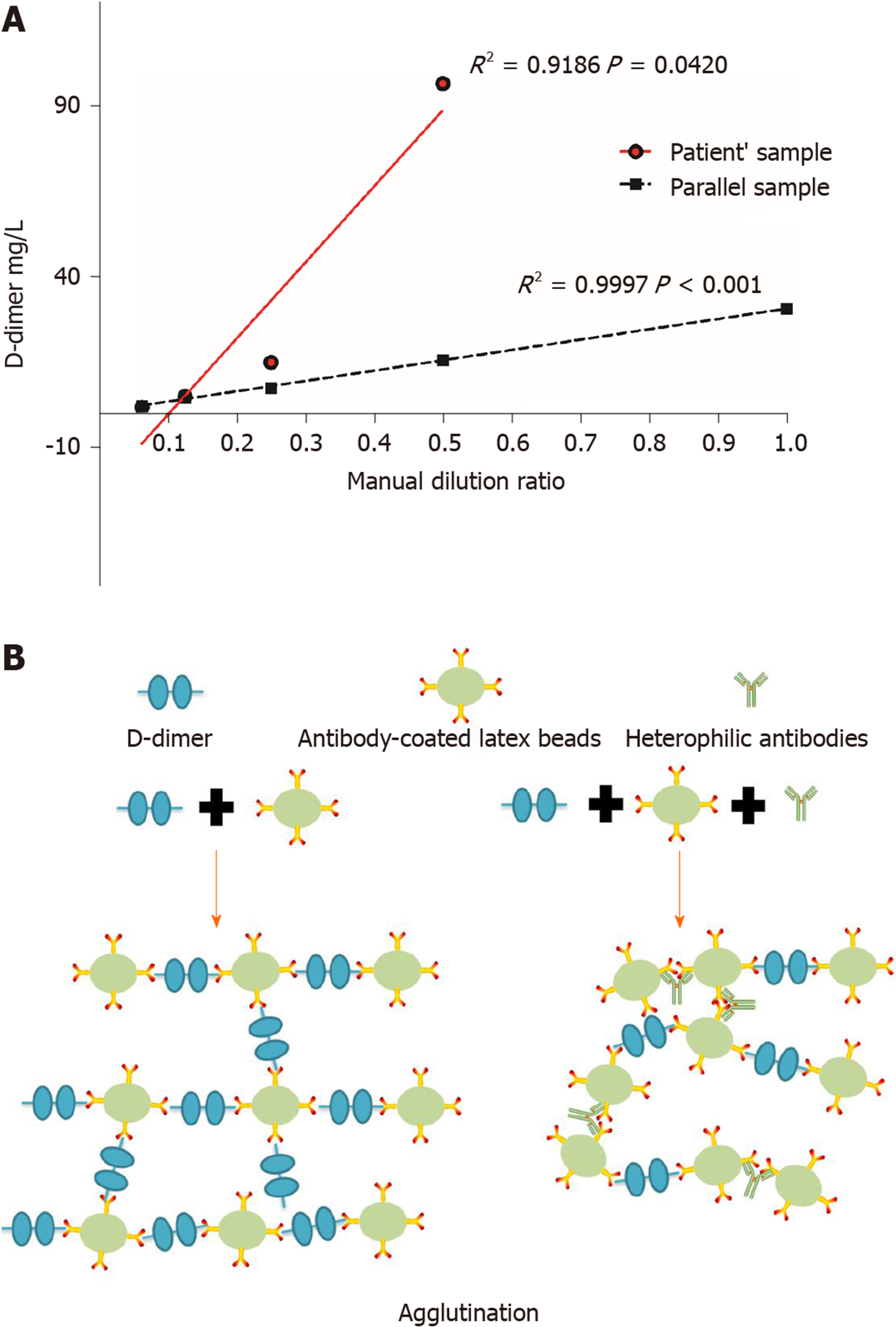
In this case, repeated testing confirmed that her D-dimer levels were remarkably elevated above the qualified range. Nevertheless, the patient had no relevant clinical symptoms or radiographic evidence of abnormalities in parallel FDP values and other coagulation parameters indicating thrombosis, and therefore the possibility of interference arose. As an initial step in the diagnostic workshop, the sample was manually diluted to various levels and then calibrated using Innovaccer D-dimer assays. The patient’s results yielded a weak linear response (R2 = 0.9186) upon dilution, while the parallel sample was similar to the standard curve (R2 = 0.9997, Figure 1A). Dilution is an approach used to verify interference when the test result is remarkable high; however, weaker linear responses or nonlinear responses can result in false confirmation of suspected interference[3].
In the next step, a sample was sent for confirmation to another laboratory where they use HamosIL D-dimer HS for ACL TOP (Instrumentation Laboratory, Bedford, MA, United States), which is also a latex-enhanced turbidimetric immunoassay. The cut-off value is 0.242 mg/L, and her sample D-dimer value was 4.49 mg/L, which was substantially lower than the results from our laboratory. This confirmed that there was some interference in the sample.
Heterophilic antibody (HA) interference is still a threat in immunoassays, and D-dimer testing is not exempted from interference. Although the Innovance reagent additive could neutralize some interfering substances such as bilirubin, rheumatoid factors, and blood clotting, it was hypothesized that HA might play a critical role in this case. Thus, a blocking experiment was conducted to further investigate this controversial phenomenon. The sample was treated with three kinds of specific heterophilic antibody blocking reagents (HBT antibodies Laboratory Inc., Santee, CA, United States) and then measured with Innovance D-dimer. The testing presented a remarkable discrepancy of values, that is, 9.42, 9.06, and 12.58 mg/L vs > 100 mg/L, which is highly indicative of the presence of HAs in the sample that were interfering with the immunoturbidimetric assay used in our laboratory for routine measurement of D-dimers.
Interestingly, both the Innovance and HamosIL D-dimer assays are latex-enhanced turbidimetric immunoassays, and the monoclonal antibodies chosen to coat the beads are both clone 8D3 according to the user manuals. Thus, we propose that the HAs in this case could have impressive affinity to the Fc-region of the 8D3antibodiesand could bridge the beads independently of D-dimers, resulting in increased agglutination (Figure 1B). The results of the HBT-treated samples confirmed the presence of HAs in the sample. To rule out false elevation of endocrine tests and cardiac injury markers[4] in this case, we then reanalysed her testing results and found that the results were in the normal range (Table 1). Thus, the D-dimer test is the only one affected by HAs in this case.
It has been reported that HAs may be induced after exposure to animals such as cats and mice, mouse products, immune cells, blood transfusion, dialysis and maternal transfer, among others[3,4], but we did not find any apparent causes based on her medical history. Some screening tests were applied to identify the source. Different kinds of viral infections have also been reported to induce HAs[5,6]. Epstein-Barr virus infection is an example reported previously[7]. Therefore, real-time PCR and serum antibodies against EBV were tested at the same time. The EBV-DNA load measured in her peripheral blood mononuclear cells was 3.4E04 copies/mL (Epstein-Barr Virus DNA Quantitative Fluorescence Diagnostic Kit, Changsha, Hunan Province, China), while all of her immunoglobulin G antibodies against EBV viral capsid antigen (VCA), early antigen (EA), and nuclear antigen (NA) were positive except for immunoglobulin M against VCA. This patient was then diagnosed with an EBV infection. Heterophilic antibodies tend to peak 2–5 wk after symptom onset and may only rarely persist for 6-12 mo[8], so we confirmed that her EBV infection was contributing to the phenomenon. However, how many D-dimer tests could be underestimated due to heterophilic antibodies against Epstein-Barr virus needs further investigation.
Caused by SARS-CoV-2, COVID-19 has become a global pandemic. Unfortunately, in this case, the understanding of the immunologic characteristics of SARS-COV-2 was still relatively scarce. A variety of serological assays were established for detecting SARS-COV-2, such as chemiluminescence assay (CLIA) and colloidal gold immunochromatographic assay (GICA), through immunoassay. Moreover, some COVID-19 patients demonstrated abnormal antiphospholipid antibodies and coagulopathy consistently[9]. Therefore, heterophilic antibody should be cautious as one of the factors that contribute to interference even to false-positive results.
In summary, heterophilic antibodies should be considered when an elevated D-dimer value does not conform with the clinical evidence. It is believed that it could be a better method if there is standardization of D-dimer reagents[10]. But for now, using different instruments and heterophilic antibody blockers could rule out most of the interference. We will subsequently do serial monitoring of D-dimer values during anti-viral therapy, and more research needs to be done to verify the exact interfering fragment to improve the D-dimer test in the near future.
We are grateful for the instructive discussion with Professor Qian Shen and her generous reagent donations.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Berezin AE S-Editor: Liu JH L-Editor: Wang TQ P-Editor: Liu JH
| 1. | Weitz JI, Fredenburgh JC, Eikelboom JW. A Test in Context: D-Dimer. J Am CollCardiol. 2017;70:2411-2420. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 202] [Cited by in F6Publishing: 268] [Article Influence: 38.3] [Reference Citation Analysis (0)] |
| 2. | Salvagno GL, Lippi G, Manzato F, Giavarina D, Montagnana M, Poli G, Guidi GC. Analytical comparison of AxSYM, HemosIL DD HS and Innovance D-dimer immunoassays with the Vidas D-dimer. Int J Lab Hematol. 2009;31:475-477. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 5] [Cited by in F6Publishing: 7] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 3. | Bolstad N, Warren DJ, Nustad K. Heterophilic antibody interference in immunometric assays. Best Pract Res ClinEndocrinolMetab. 2013;27:647-661. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 135] [Cited by in F6Publishing: 123] [Article Influence: 11.2] [Reference Citation Analysis (0)] |
| 4. | Morton A. When lab tests lie … heterophile antibodies. Aust Fam Physician. 2014;43:391-393. [PubMed] [Cited in This Article: ] |
| 5. | Lippi G, Ippolito L, Tondelli MT, Favaloro EJ. Interference from heterophilic antibodies in D-dimer assessment. A case report. Blood Coagul Fibrinolysis. 2014;25:277-279. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 15] [Cited by in F6Publishing: 16] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 6. | Haukenes G, Viggen B, Boye B, Kalvenes MB, Flø R, Kalland KH. Viral antibodies in infectious mononucleosis. FEMS Immunol Med Microbiol. 1994;8:219-224. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 18] [Cited by in F6Publishing: 18] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 7. | Luderer R, Kok M, Niesters HG, Schuurman R, de Weerdt O, Thijsen SF. Real-time Epstein-Barr virus PCR for the diagnosis of primary EBV infections and EBV reactivation. Mol Diagn. 2005;9:195-200. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 22] [Cited by in F6Publishing: 20] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 8. | De Paschale M, Clerici P. Serological diagnosis of Epstein-Barr virus infection: Problems and solutions. World J Virol. 2012;1:31-43. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 180] [Cited by in F6Publishing: 179] [Article Influence: 14.9] [Reference Citation Analysis (2)] |
| 9. | Zhang Y, Xiao M, Zhang S, Xia P, Cao W, Jiang W, Chen H, Ding X, Zhao H, Zhang H, Wang C, Zhao J, Sun X, Tian R, Wu W, Wu D, Ma J, Chen Y, Zhang D, Xie J, Yan X, Zhou X, Liu Z, Wang J, Du B, Qin Y, Gao P, Qin X, Xu Y, Zhang W, Li T, Zhang F, Zhao Y, Li Y, Zhang S. Coagulopathy and Antiphospholipid Antibodies in Patients with Covid-19. N Engl J Med. 2020;382:e38. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1532] [Cited by in F6Publishing: 1549] [Article Influence: 387.3] [Reference Citation Analysis (0)] |
| 10. | Wu Y, Xiao YX, Huang TY, Zhang XY, Zhou HB, Zhang XX, Wu YE. What makes D-dimer assays suspicious-heterophilic antibodies? J Clin Lab Anal. 2019;33:e22687. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 15] [Cited by in F6Publishing: 13] [Article Influence: 2.6] [Reference Citation Analysis (0)] |