Published online Oct 6, 2019. doi: 10.12998/wjcc.v7.i19.3153
Peer-review started: May 8, 2019
First decision: August 1, 2019
Revised: August 16, 2019
Accepted: September 9, 2019
Article in press: September 9, 2019
Published online: October 6, 2019
There are some challenges concerning immediate implant placement in the molar region. Platelet-rich fibrin (PRF), an autologous biomaterial, has been used widely for periodontal intra-bony defects, sinus augmentation, socket preservation, and gingival recession. However, the literature remains scarce for reports on immediate implants with PRF, particularly in the case of fresh molar extraction socket.
The patient was a 43-year-old woman with maxillary molar vertical crown-root fracture. She underwent flapless immediate implant placement into the fresh molar socket with PRF. At the follow-up visit 15 d post procedure, the vascularization of soft tissue was visible. There was no swelling or pain after the surgery. Six months postoperatively, the regeneration of bone and soft tissues was visible. Subsequently, the definitive restoration was placed. The patient was satisfied with the aesthetic outcomes.
The flapless immediate implant placement into the fresh molar socket with PRF is a feasible procedure. This case report demonstrates that PRF promotes bone and soft tissue regeneration apart from having an enhanced anti-inflammatory ability. Furthermore, the procedure involves a minimally invasive technique, thus reducing the surgical complexity.
Core tip: The advantages of flapless immediate molar implant placement with platelet-rich fibrin included: (A) Promotion of bone and soft tissue regeneration; (B) Enhancement of the anti-inflammatory ability; (C) Minimally invasive procedure; and (D) Low surgical complexity.
- Citation: Sun XL, Mudalal M, Qi ML, Sun Y, Du LY, Wang ZQ, Zhou YM. Flapless immediate implant placement into fresh molar extraction socket using platelet-rich fibrin: A case report. World J Clin Cases 2019; 7(19): 3153-3159
- URL: https://www.wjgnet.com/2307-8960/full/v7/i19/3153.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v7.i19.3153
Immediate implant placement into fresh extraction is gaining popularity because of several advantages. Apart from involving fewer clinical procedures compared to conventional methods, this new technique also facilitates the maintenance of bone architecture. Many studies showed that the survival rate of the immediate implantation is comparable to that of the healed implantation[1-3]. The great mass of literature on immediate implant placement focused on the aesthetic zone and premolar region[4-6]. Published evidence on the molar region remains scarce. From the available literature, there are some challenges concerning immediate implant placement in the molar region. One of them is that the bulky molar root often leads to insufficient bone quantity in the fresh extraction socket. To overcome this, guided bone regeneration (GBR) is often performed to augment the bone around the implant[7,8]. However, if exposure of surgical site or infection occurs, it may seriously affect the process of bone augmentation, possibly leading to implant failure[9-11]. Another main challenge may arise when the defect of gingival tissues around the extraction socket leads to unfavorable primary closure. As a result, the buccal tissue needs to be periosteal-released in order to close the socket. This might come at the cost of compromising the blood supply and decreasing the attached gingival. In view of this, connective tissue graft has been devised as an alternative approach to correct the soft tissue deficiency with a donor site[12,13].
Platelet-rich fibrin (PRF), a second-generation platelet concentrate, is an autologous fibrin matrix. PRF contains platelets, growth factors, and leukocytes. Studies reported that PRF could provide a sustained release of the growth factors for tissue regeneration from 7 up to 28 d[14,15]. Furthermore, as an autologous biomaterial, PRF is able to facilitate cell proliferation, cell migration, angiogenesis, and infection prevention[16,17]. Thus, PRF has been widely used in periodontal intra-bony defects[18], sinus augmentation[19], socket preservation[20], and gingival recession[21]. However, very few cases about immediate implants with PRF have been reported, particularly in fresh molar extraction socket.
This case report describes immediate implant placement in fresh molar extraction socket, together with the use of PRF for bone regeneration and the soft tissue augmentation around the implant. GBR with PRF was performed to ensure sufficient bone tissues as support structure around the implant.
A 43-year-old female patient who was a non-smoker presented complaining of mobility of tooth #26.
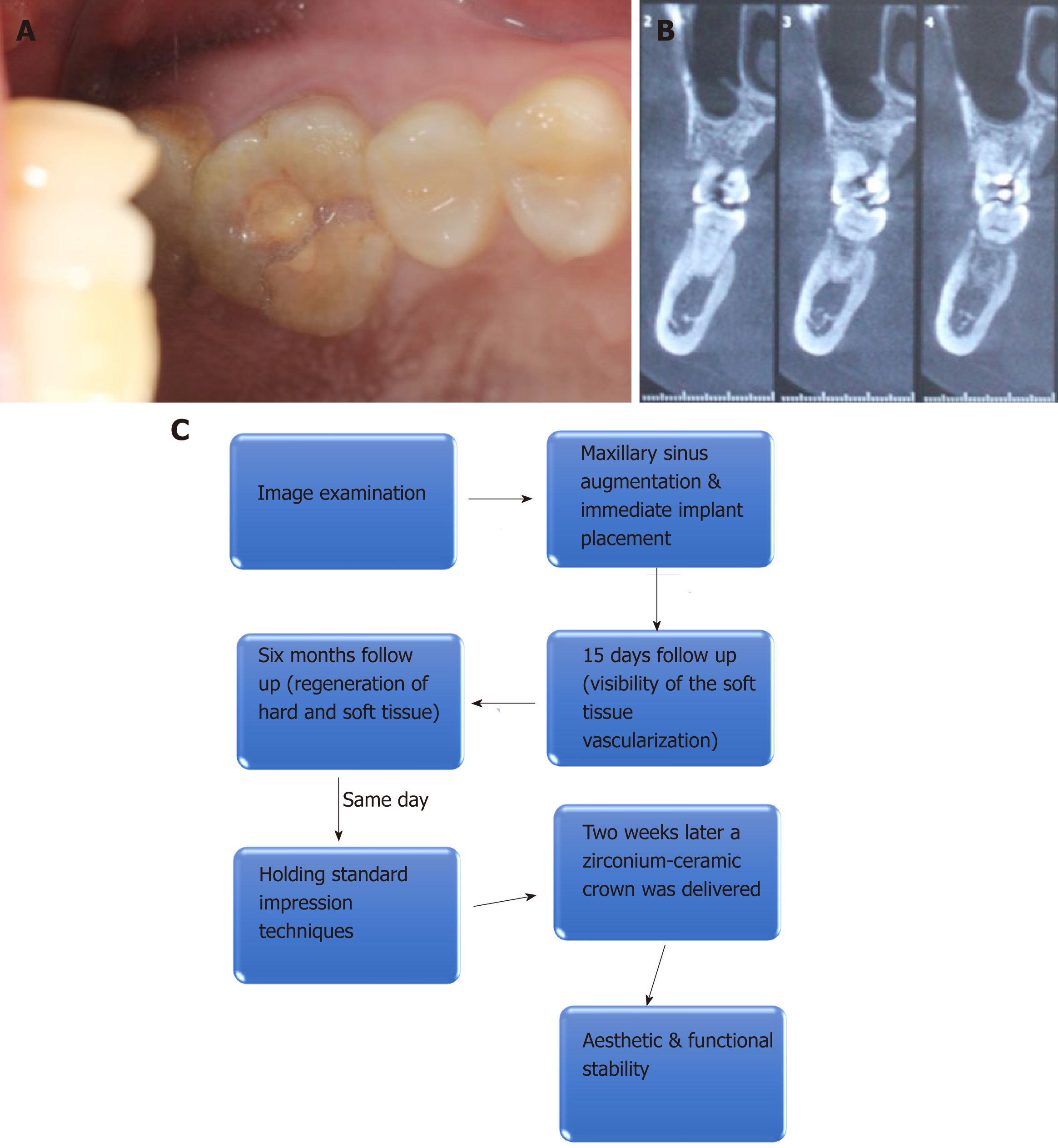
Clinical examination revealed that tooth #26 contained resin filling. It also presented as a vertical crown-root fracture, with no swelling but pain and difficulty in eating recorded (Figure 1A).
There was no significant systemic complaint. The family history was unremarkable.
Cone-beam computed tomography revealed a fracture line that extended from the occlusal surface to the end of the palatal root. The available bone height was 4 mm (Figure 1B). Clinical examination revealed that tooth #26 contained resin filling. She was diagnosed as having vertical crown-root fracture of tooth #26 (Figure 1A and B).
Vertical crown-root fracture of tooth #26.
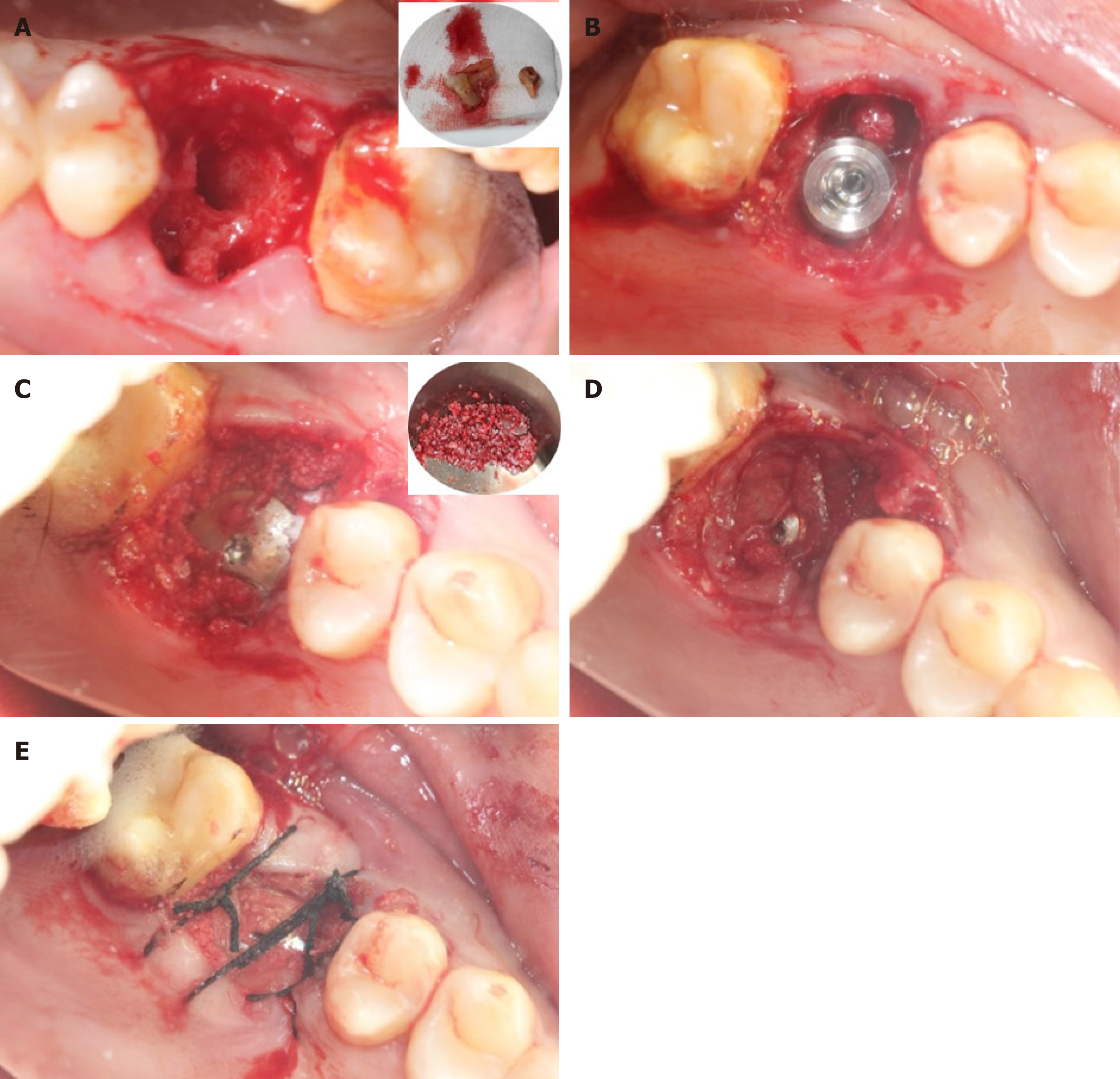
Based on the findings, immediate implant placement on tooth #26 combined with maxillary sinus floor augmentation was planned to resolve her complaint. The treatment plan was discussed with the patient, and based on the patient’s condition, the according treatment plan was drawn up as shown in Figure 1C. Pre-operatively, the patient rinsed her mouth with 0.12% chlorhexidine solution for 3 min every time, for a total of three times. Local anesthesia was administered. The molar tooth was removed using a minimally invasive flapless technique to preserve the socket walls (Figure 2A). Then, the socket was thoroughly debrided and irrigated. As the residual bone height was 6 mm, maxillary sinus floor augmentation was performed. After that, an implant (SLA, Straumann, Switzerland, 4.8 mm × 10 mm, soft level implant) was placed into the fresh socket and good primary implant stability was achieved (Figure 2B). In the four-wall bony defect, the healing abutment was screwed. PRF was prepared as described in a previously published study[22]. The bio-oss collagen with PRF was placed into the space between the implant and the socket walls (Figure 2C). Subsequently, the wound was covered with a PRF membrane. Sutures were put on loosely to allow the regeneration of soft tissue (Figure 2D and E). Postoperatively, 500 mg of azithromycin was prescribed (twice daily for 5 d). The patient was instructed to avoid chewing in the surgical area and to continue the mouthwash with chlorhexidine 0.12% for 10 d. Sutures were removed after 10 d.
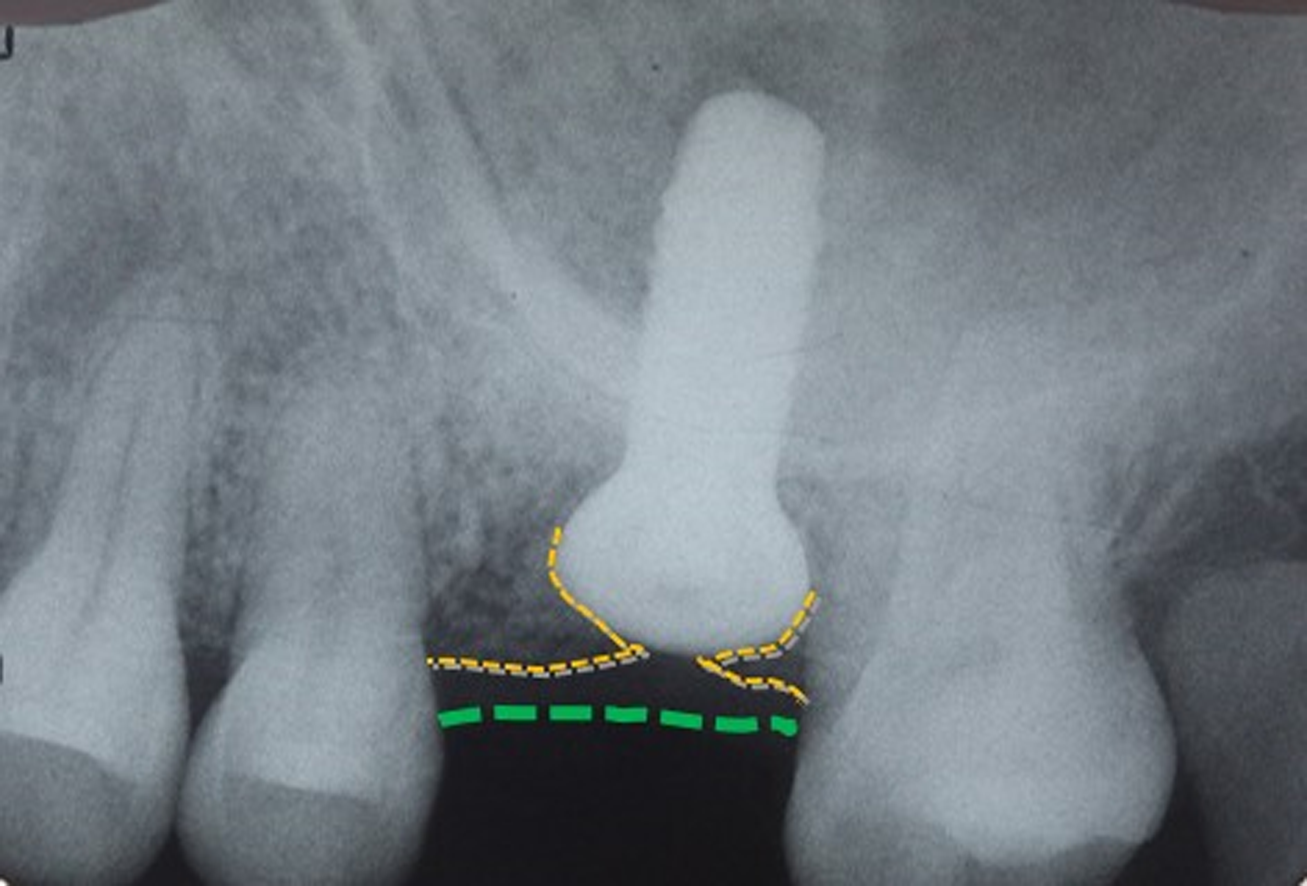
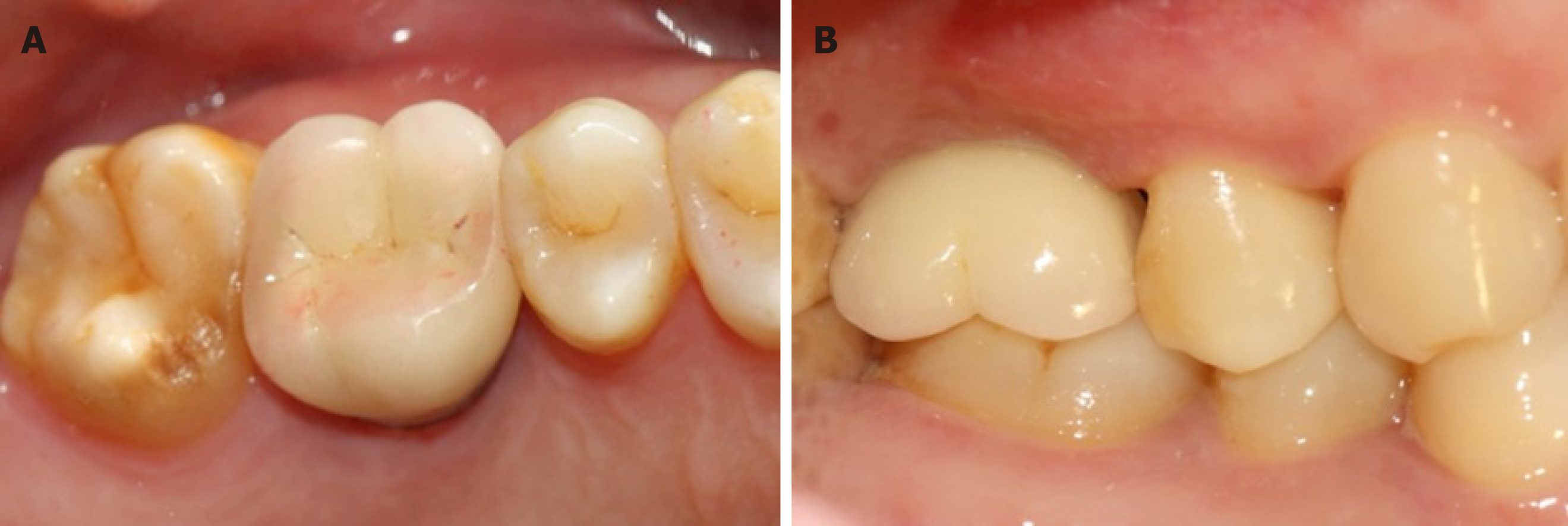
At the follow-up visit 15 d later, the vascularization of soft tissue was visible (Figure 3). There was no swelling or pain after the surgery. Six months postoperatively, the regeneration of bone tissue and soft tissue was visible under a periapical standard radiograph that was taken by a parallel technique (Figure 4). Subsequently, the second stage surgery was performed. The implant was exposed by minimally invasive incision. Healing abutment was replaced. The impression was carried out. The definitive restoration was placed after 2 wk (Figure 5). The patient was satisfied with the aesthetic outcomes.
With the advancement in implantology, immediate dental implant placement into fresh molar extraction socket has been presented as an alternative treatment to delayed placement. The survival rate of immediate molar implant placement was found to be the same as that of the delayed placement[23]. Nevertheless, the uptake of immediate implant placement in the molar socket has been hampered by several conditions that may affect the clinical outcomes, one of which is the implant stability. For immediate molar implant placement procedure, the primary stability of the implant is vital for implant success. Skillful preservation of the septal bone is a crucial step towards the success of the procedure. In order to obtain adequate primary stability of the implant, the molar tooth should be atraumatically extracted while preserving as much of the septal bone as possible. For this patient, the molar tooth was removed using a minimally invasive technique. The septal bone was completely preserved. As a result, the implant was successfully placed in the septal bone with good primary stability.
Furthermore, by applying the flapless procedure, there was less crestal bone loss compared to the flap procedure. A flapless procedure causes very minimal disruption to the periosteum; thus, it is able to maintain the periosteal blood supply to the buccal plate[23]. Many previous studies have reported that immediate implant placement with GBR could counteract the bone absorption after the tooth extraction[24,25]. As presented in a systematic review, an immediate implant with bone substitute material was shown to be beneficial towards the prevention of alveolar resorption and maintenance of soft tissue stability[26]. Recently, a study by Mudalal et al[27] showed that PRF was a biocompatible autograft material and that it had an outstanding ability of enhancing bone regeneration in immediate implant placement procedure. PRF is a fibrin membrane with abundant growth factors. These growth factors are important to promote the regeneration of bone tissue. For this patient, we were able to minimize the surgical trauma and preserve the blood supply by using the flapless procedure. The bio-oss collagen with PRF was placed into the space between the implant and the socket walls to promote the regeneration of bone tissues. After the procedure, no pain or swelling was experienced by the patient. During the 6-mo follow-up, new bones were visible on a periapical standard radiograph.
In most molar tooth extraction cases, the primary closure could be difficult to obtain due to the bulky root of the molar tooth. However, the primary closure was critical to ensure the success of the GBR procedure. Garcia et al[28] reported that GBR procedures that were done without membrane exposure could yield more regenerated bone compared to those done with membrane exposure. The flap procedure with relaxation incision is commonly used in the management of soft tissue to obtain primary closure. However, this procedure could disrupt the blood supply, leading to postoperative swelling and pain. In addition, this procedure has a higher complexity as it involves the use of connective tissue free flap, thus requiring a donor site. Several studies have shown that PRF played a significant role in promoting early wound healing besides enhancing anti-inflammatory ability[29]. In the present case, PRF membrane was covered on the wound without primary closure. The porous membrane structure of PRF allowed the discharge of the exudates. In other words, the PRF membrane was able to promote the regeneration of the soft tissue via the release of growth factors, on top of serving as a substitute barrier membrane to the absorbable membrane. By 15 d after the procedure, the vascularization of soft tissue was clearly visible at the follow-up visit. The regeneration of bone tissue was sufficient. Furthermore, there was no postoperative swelling or pain.
In this case, the minimal invasive extraction was performed to preserve as much of the septal bone as possible. As a result, good primary stability of the implant was achieved. The bone substitute materials with PRF were filled in the bone defects. By using a flapless procedure, there was minimal disruption of the periosteum and good preservation of the periosteal blood supply for bone regeneration. PRF was used as a membrane to primary closure. It was able to reduce post-surgical swelling, pain, and infection. Furthermore, keratinized gingiva was produced due to the release of the growth factors from PRF. In short, the immediate implant placement into the fresh molar socket with PRF is a feasible procedure.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, Research and Experimental
Country of origin: China
Peer-review report classification
Grade A (Excellent): A
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Mattos B, Vieyra JP S-Editor: Zhang L L-Editor: Wang TQ E-Editor: Xing YX
| 1. | Rosenquist B, Grenthe B. Immediate placement of implants into extraction sockets: implant survival. Int J Oral Maxillofac Implants. 1996;11:205-209. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 14] [Cited by in F6Publishing: 14] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 2. | Chen ST, Wilson TG, Hämmerle CH. Immediate or early placement of implants following tooth extraction: review of biologic basis, clinical procedures, and outcomes. Int J Oral Maxillofac Implants. 2004;19 Suppl:12-25. [PubMed] [Cited in This Article: ] |
| 3. | Kan JYK, Rungcharassaeng K, Deflorian M, Weinstein T, Wang HL, Testori T. Immediate implant placement and provisionalization of maxillary anterior single implants. Periodontol 2000. 2018;77:197-212. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 62] [Cited by in F6Publishing: 84] [Article Influence: 14.0] [Reference Citation Analysis (0)] |
| 4. | den Hartog L, Slater JJ, Vissink A, Meijer HJ, Raghoebar GM. Treatment outcome of immediate, early and conventional single-tooth implants in the aesthetic zone: a systematic review to survival, bone level, soft-tissue, aesthetics and patient satisfaction. J Clin Periodontol. 2008;35:1073-1086. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 194] [Cited by in F6Publishing: 202] [Article Influence: 13.5] [Reference Citation Analysis (0)] |
| 5. | Ferrus J, Cecchinato D, Pjetursson EB, Lang NP, Sanz M, Lindhe J. Factors influencing ridge alterations following immediate implant placement into extraction sockets. Clin Oral Implants Res. 2010;21:22-29. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 196] [Cited by in F6Publishing: 195] [Article Influence: 13.0] [Reference Citation Analysis (0)] |
| 6. | De Rouck T, Collys K, Cosyn J. Single-tooth replacement in the anterior maxilla by means of immediate implantation and provisionalization: a review. Int J Oral Maxillofac Implants. 2008;23:897-904. [PubMed] [Cited in This Article: ] |
| 7. | Gher ME, Quintero G, Assad D, Monaco E, Richardson AC. Bone grafting and guided bone regeneration for immediate dental implants in humans. J Periodontol. 1994;65:881-891. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 119] [Cited by in F6Publishing: 112] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 8. | Becker W, Lynch SE, Lekholm U, Becker BE, Caffesse R, Donath K, Sanchez R. A comparison of ePTFE membranes alone or in combination with platelet-derived growth factors and insulin-like growth factor-I or demineralized freeze-dried bone in promoting bone formation around immediate extraction socket implants. J Periodontol. 1992;63:929-940. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 140] [Cited by in F6Publishing: 126] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 9. | Augthun M, Yildirim M, Spiekermann H, Biesterfeld S. Healing of bone defects in combination with immediate implants using the membrane technique. Int J Oral Maxillofac Implants. 1995;10:421-428. [PubMed] [Cited in This Article: ] |
| 10. | Simion M, Baldoni M, Rossi P, Zaffe D. A comparative study of the effectiveness of e-PTFE membranes with and without early exposure during the healing period. Int J Periodontics Restorative Dent. 1994;14:166-180. [PubMed] [Cited in This Article: ] |
| 11. | Nemcovsky CE, Artzi Z, Moses O. Rotated palatal flap in immediate implant procedures. Clinical evaluation of 26 consecutive cases. Clin Oral Implants Res. 2000;11:83-90. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 35] [Cited by in F6Publishing: 37] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 12. | Juodzbalys G, Wang HL. Soft and hard tissue assessment of immediate implant placement: a case series. Clin Oral Implants Res. 2007;18:237-243. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 67] [Cited by in F6Publishing: 74] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 13. | Wiesner G, Esposito M, Worthington H, Schlee M. Connective tissue grafts for thickening peri-implant tissues at implant placement. One-year results from an explanatory split-mouth randomised controlled clinical trial. Eur J Oral Implantol. 2010;3:27-35. [PubMed] [Cited in This Article: ] |
| 14. | Dohan DM, Choukroun J, Diss A, Dohan SL, Dohan AJ, Mouhyi J, Gogly B. Platelet-rich fibrin (PRF): a second-generation platelet concentrate. Part II: platelet-related biologic features. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006;101:e45-e50. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 544] [Cited by in F6Publishing: 612] [Article Influence: 34.0] [Reference Citation Analysis (0)] |
| 15. | He L, Lin Y, Hu X, Zhang Y, Wu H. A comparative study of platelet-rich fibrin (PRF) and platelet-rich plasma (PRP) on the effect of proliferation and differentiation of rat osteoblasts in vitro. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009;108:707-713. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 283] [Cited by in F6Publishing: 305] [Article Influence: 21.8] [Reference Citation Analysis (0)] |
| 16. | Dohle E, El Bagdadi K, Sader R, Choukroun J, James Kirkpatrick C, Ghanaati S. Platelet-rich fibrin-based matrices to improve angiogenesis in an in vitro co-culture model for bone tissue engineering. J Tissue Eng Regen Med. 2018;12:598-610. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 45] [Cited by in F6Publishing: 65] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 17. | Bielecki T, Dohan Ehrenfest DM, Everts PA, Wiczkowski A. The role of leukocytes from L-PRP/L-PRF in wound healing and immune defense: new perspectives. Curr Pharm Biotechnol. 2012;13:1153-1162. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 106] [Cited by in F6Publishing: 112] [Article Influence: 10.2] [Reference Citation Analysis (0)] |
| 18. | Zhou J, Li X, Sun X, Qi M, Chi M, Yin L, Zhou Y. Bone regeneration around immediate placed implant of molar teeth with autologous platelet-rich fibrin: Two case reports. Medicine (Baltimore). 2018;97:e13058. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 6] [Cited by in F6Publishing: 5] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 19. | Tanaka H, Toyoshima T, Atsuta I, Ayukawa Y, Sasaki M, Matsushita Y, Hiraoka R, Koyano K, Nakamura S. Additional Effects of Platelet-Rich Fibrin on Bone Regeneration in Sinus Augmentation With Deproteinized Bovine Bone Mineral: Preliminary Results. Implant Dent. 2015;24:669-674. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 15] [Cited by in F6Publishing: 17] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 20. | Temmerman A, Vandessel J, Castro A, Jacobs R, Teughels W, Pinto N, Quirynen M. The use of leucocyte and platelet-rich fibrin in socket management and ridge preservation: a split-mouth, randomized, controlled clinical trial. J Clin Periodontol. 2016;43:990-999. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 89] [Cited by in F6Publishing: 103] [Article Influence: 12.9] [Reference Citation Analysis (0)] |
| 21. | Jankovic S, Aleksic Z, Klokkevold P, Lekovic V, Dimitrijevic B, Kenney EB, Camargo P. Use of platelet-rich fibrin membrane following treatment of gingival recession: a randomized clinical trial. Int J Periodontics Restorative Dent. 2012;32:e41-e50. [PubMed] [Cited in This Article: ] |
| 22. | Mudalal M, Zhou YM. Biological Additives and Platelet Concentrates for Tissue Engineering on Regenerative Dentistry Basic Science and Concise Review. Asian J Pharm. 2017;5:25-42. [Cited in This Article: ] |
| 23. | Ketabi M, Deporter D, Atenafu EG. A Systematic Review of Outcomes Following Immediate Molar Implant Placement Based on Recently Published Studies. Clin Implant Dent Relat Res. 2016;18:1084-1094. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 29] [Cited by in F6Publishing: 30] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 24. | Araújo MG, Linder E, Lindhe J. Bio-Oss collagen in the buccal gap at immediate implants: a 6-month study in the dog. Clin Oral Implants Res. 2011;22:1-8. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 148] [Cited by in F6Publishing: 145] [Article Influence: 10.4] [Reference Citation Analysis (0)] |
| 25. | Sanz M, Lindhe J, Alcaraz J, Sanz-Sanchez I, Cecchinato D. The effect of placing a bone replacement graft in the gap at immediately placed implants: a randomized clinical trial. Clin Oral Implants Res. 2017;28:902-910. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 64] [Cited by in F6Publishing: 72] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 26. | Li H, Zheng J, Zhang S, Yang C, Kwon YD, Kim YJ. Experiment of GBR for repair of peri-implant alveolar defects in beagle dogs. Sci Rep. 2018;8:16532. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 10] [Cited by in F6Publishing: 13] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 27. | Mudalal M, Sun XL, Li X, Fang J, Qi ML, Wang J, Du LY, Zhou YM. Minimally invasive endoscopic maxillary sinus lifting and immediate implant placement: A case report. World J Clin Cases. 2019;7:1234-1241. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 2] [Cited by in F6Publishing: 4] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 28. | Garcia J, Dodge A, Luepke P, Wang HL, Kapila Y, Lin GH. Effect of membrane exposure on guided bone regeneration: A systematic review and meta-analysis. Clin Oral Implants Res. 2018;29:328-338. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 66] [Cited by in F6Publishing: 88] [Article Influence: 14.7] [Reference Citation Analysis (0)] |
| 29. | Mudalal M, Sun X, Li X, Zhou Y. The evaluation of leukocyte-platelet rich fibrin as an anti-inflammatory autologous biological additive. A novel in vitro study. Saudi Med J. 2019;40:657-668. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 7] [Cited by in F6Publishing: 8] [Article Influence: 2.0] [Reference Citation Analysis (0)] |