Published online Sep 6, 2022. doi: 10.12998/wjcc.v10.i25.8880
Peer-review started: March 31, 2022
First decision: May 11, 2022
Revised: June 6, 2022
Accepted: August 1, 2022
Article in press: August 1, 2022
Published online: September 6, 2022
Population’s mental health surveillance is essential for knowing the distribution of mental well-being and mental disorders in the society. This allows for the establishment, evaluation, and revision of preventive measures and curative services. The results of such monitoring should serve as a database for evidence-based mental health policy. Mental disorders are among the top ten causes of burden globally and crisis situations such as the pandemic increase the risk of mental health problems, as they cause constant fear of contagion and the implementation of restrictive measures. The impact of the coronavirus disease 2019 (COVID-19) pandemic on the general population of the Slovak Republic has not yet been studied. The hypothesis was that more than one fifth of the population (women to a greater extent) will have symptoms of anxiety and depression.
To assess the mental health of the general Slovak population aged 15 years and older in the summer of 2021 by determining the prevalence of depressive and anxiety symptoms.
An anonymous cross-sectional survey was implemented in a sample of 1501 respondents in the summer of 2021 during the COVID-19 pandemic. The inclusion criteria were age of 15 years and older and ability to complete the survey questionnaire online or in a face-to-face interview. The survey assessed anxiety symptoms by the seven-item general anxiety disorder and depressive symptoms by the nine-item patient health questionnaire instruments. Recognized cut-off scores of 10 or greater were used for both.
Anxiety symptoms were present in 19.32% and depression in 24.65% of the sample. Symptoms of both disorders were more common in females: 15.00% of males and 24.00% of females experienced anxiety symptoms, and 19.00% of males and 30.00% of females experienced symptoms of depression. Symptoms of both disorders were the most common in the youngest age group (15-25 years old): One fifth of males (20.29%) and one third of females (35.32%) had symptoms of anxiety, and 26.09% males and 43.79% females had symptoms of depression. Mean score for anxiety was 5.44 [standard deviations (SD) = 4.96] for the overall sample, 6.15 (SD = 5.14) for females, and 4.67 (SD = 4.63) for males. The youngest females of the 15-25 years age group had the highest score (7.55, SD = 5.27) among all age groups, for both sexes. Mean score for depression was 6.74 for the overall sample (SD = 5.75), 7.43 for females (SD = 5.87), and 5.99 (SD = 5.52) for males. The highest depression score was observed in the youngest females of the 15-25 years age group (9.34, SD = 6.07). We found a significant association between anxiety or depressive symptoms and younger age [odds ratio (OR): 1.69, 95% confidence interval (CI): 1.16-2.45 and OR: 1.65, 95%CI: 1.17-2.34, respectively], being female (OR: 1.86, 95%CI: 1.42-2.42 and OR: 1.76, 95%CI: 0.20-0.29, respectively), and having primary education (OR: 1.66, 95%CI: 1.08-2.54 and OR: 1.65, 95%CI: 1.16-2.63, respectively).
Results of our study indicate that anxiety and depression are frequent in the Slovak Republic during the COVID-19 pandemic. This important observation should serve as an information basis for the development of effective mental health policies, consisting of preventive programs, and early detection and effective treatment services. The study results provide strong argument for the necessity of mental health reform that is currently being shaped in the Slovak Republic.
Core Tip: We have implemented a survey to assess anxiety and depressive symptoms by the general anxiety disorder and the patient health questionnaire instruments in the Slovak Republic during the coronavirus disease 2019 pandemic. Anxiety was present in 19.32% and depression in 24.65% of the population. Both disorders were more common in females. Our results indicate that anxiety and depressive symptoms were significantly associated with younger age, female sex, and lower than high school education. This is the first such survey of the population’s mental health in the Slovak Republic and the findings are important for the planning and improvement of mental health services in the country.
- Citation: Kralova M, Brazinova A, Sivcova V, Izakova L. Mental health of the Slovak population during COVID-19 pandemic: A cross-sectional survey. World J Clin Cases 2022; 10(25): 8880-8892
- URL: https://www.wjgnet.com/2307-8960/full/v10/i25/8880.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i25.8880
Population’s mental health surveillance is essential for knowing the distribution of mental well-being and mental disorders in the society. Mental disorders are among the top ten causes of burden for the global society, causing impairment that decreases the quality of life. The burden caused by mental disorders has increased over the past 30 years, with the two most common worldwide being affective and anxiety disorders[1]. Mental, neurological, and substance use disorders are the leading causes of years lived with disability. Despite the significant contribution of mental disorders to disability globally and their expected rise in the coming decades, mental health care has not been addressed in most countries to the same extent as physical health care. A large proportion of persons affected by these disorders do not have access to treatment[2]. Mental well-being has an important impact on an individual’s performance and population’s health. Its monitoring at the population level is crucial for the awareness of the current state and trends. This allows for the establishment, evaluation, and revision of preventive measures and curative services. The results of such monitoring should serve as a database for evidence-based mental health policy.
A population’s mental health is largely affected by crisis situations. In the beginning of the year 2020, the rapid spread of the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) virus as a causative agent for the coronavirus disease 2019 (COVID-19) has led to the declaration of a global pandemic on March 11, 2020 by the World Health Organization. The COVID-19 pandemic is an international public health emergency increasing the risk to both physical and mental health. The constant perception of risk of contagion, the absence of a definitive treatment for the disease, implemented measures such as social isolation[3], and the associated economic consequences are the factors negatively impacting the mental health of the population. Mounting scientific evidence shows an association between the COVID-19 pandemic and impaired mental health, mainly in the form of an increased prevalence of depressive and anxiety symptoms in the general population[4-6]. For the assessment of population’s mental health, numerous instruments are in use. The prevalence of depressive and anxiety symptoms in a population are frequently measured by the seven-item general anxiety disorder (GAD-7) and the nine-item patient health questionnaire (PHQ-9) instruments. Both have been formally validated against diagnostic clinical interviews to establish the sensitivity, specificity, and positive and negative predictive values of cut-off scores, and are used widely in clinical research[7,8]. These instruments are being used to evaluate the prevalence of depressive and anxiety symptoms in the general public or in specific population groups. The latter includes, for example, frontline workers, which can be medical students or health care professionals during the COVID-19 pandemic[9-11]. Apart from the observed impact of the crisis situation on the general public, substantial neurological and psychiatric morbidity is evident in people who have recovered from COVID-19, largely within the first half year after the infection. The risks were the highest in those with a severe case of COVID-19. A neurological or psychiatric diagnosis was present in one third of the patients[12].
The impact of the COVID-19 pandemic on the general population of the Slovak Republic has not yet been studied. Several studies were conducted to assess the current state of mental health of Slovak university students. The Slovak Republic is a Central European country with a population of about 5.7 million inhabitants, 53.70% of whom live in urban settings. The state of the population‘s mental health in the country can be assessed only from available routine statistics data-the number of people treated in outpatient and inpatient psychiatric care services. A general population survey was not carried out before the COVID-19 pandemic. Professional estimates signal a large gap in mental health and social care needs of persons affected by mental disorders in Slovakia, with about two thirds of people with affective disorders and an even larger proportion of those with anxiety disorders not receiving treatment[13]. The first COVID-19 case in Slovakia was confirmed on March 6, 2020. Subsequently, first an emergency situation and later on, a state of emergency was declared by the government, lasting 7 mo until May 2021. Strict rules and measures adopted at the beginning of the pandemic kept the first pandemic wave under control. In the second wave of the pandemic, during the winter of 2020/2021, the situation worsened significantly. At the beginning of 2021, the COVID-19 vaccination roll-out was implemented. However, in February 2021, Slovakia became the worst in the world in terms of deaths and hospitalized cases per capita. The situation improved towards the end of the spring of 2021 until the summer, when the third wave of the pandemic caused by the Delta variant of SARS-CoV-2 began in the country.
Three published studies evaluated mental health of young Slovaks during the COVID-19 pandemic. A study investigating the prevalence of depressive symptoms and the level of perceived stress during distance learning in the period of the COVID-19 pandemic among students of four Slovak universities showed that almost half of the participants were depressed and almost all perceived increased stress levels. Data collection was performed in March and April 2021[14]. Another two studies investigated the prevalence of depression and anxiety among college students in the Slovak Republic in 2020, using the PHQ-9 and GAD-7 instruments. They reported a prevalence of anxiety in 20% and 35% and depression in 34% and 47% of the study samples[15,16].
The aim of the current study was to assess the mental health of the general Slovak population aged 15 years and older in the summer of 2021 by determining the prevalence of depressive and anxiety symptoms. The hypothesis was that more than one fifth of the population (women to a greater extent) will have symptoms of anxiety and depression.
The greatest contribution of the study is the providing of unique information on the current state of mental health of the population of the Slovak Republic during the COVID-19 pandemic. The study results can contribute to the development of effective strategies for the improvement of the country’s mental health.
A cross-sectional study was implemented in July 2021 during the COVID-19 pandemic in the Slovak Republic to assess the prevalence of depressive and anxiety symptoms. The study was performed in a sample of 1501 respondents. The sample was drawn from the general population of individuals aged 15 years or more. The sample size was estimated using 95% confidence interval (CI) and 2.6% margin of error.
This study used the data collected by one of the Slovak survey agencies in a survey requested by the non-governmental organization League for Mental Health. The survey agency conducted the survey in a full managed access panel of respondents. In total 2000 respondents were invited to complete the survey in an either online or face-to-face form, and 1660 completed the survey. The response rate thus was 83%. After cleaning the data of the incomplete entries and the entries not eligible due to the needed stratification of respondents, data of 1501 respondents were used for the study. A stratified sample design was used to construct the sample in order to ensure that the general population’s age, sex, and residence subgroups are adequately represented.
The respondents confirmed voluntary (unpaid) participation in the survey by signing an informed consent form. The inclusion criteria were age of 15 years and older and ability to complete the survey questionnaire online or in a face-to-face interview.
The survey was implemented by using a self-administered online survey (1201 respondents) and a face-to-face computer-assisted personal interviewing (300 respondents). The survey included questions on demographic and clinical variables. Demographic data included sex, age (in categories 15-25 years old, 26-35 years old, 36-45 years old, 46-55 years old, 56-69 years old, and 70 years old and more), attained level of education (in categories primary, secondary without A-level, secondary with A-level, and university), region of residence (out of 8 regions of Slovakia), and size of residence by the number of inhabitants in resident town/city (in categories < 1000, 1000-4999, 5000-19999, 20000-99999, and 100000 and more). Participants assessed their current overall health as well as their mental health on a 5-point Likert scale (poor, fair, average, good, and excellent).
Symptoms of anxiety were assessed using the 7-item instrument GAD-7. The respondent answered seven questions and for each item gives a response for frequency (scored 0-3). For the screening of anxiety, the following total scores of GAD-7 were used for the assessment of severity: 0-4: No anxiety; 5-9: Mild; 10-14: Moderate; 15 and more: Severe. The total score was 21.
Symptoms of depression were assessed by the 9-item instrument PHQ-9. For each of the nine questions, the respondents entered frequency, which was scored 0-3. Total PHQ-9 scores of 5, 10, 15, and 20 represented mild, moderate, moderately severe, and severe depression, respectively. The total score was 27.
The internal consistency of GAD-7 and PHQ-9 instruments was assessed as excellent by finding the Cronbach's alpha to be above 0.80 in numerous research studies from other countries[17,18].
Both the GAD-7 and the PHQ-9 instruments assess the current prevalence of anxiety/depressive symptoms, as they ask about the problems experienced over the past 2 wk. The instruments have been formally internationally validated and applied in the survey in the Slovak language. They have not been validated for the Slovak Republic.
To address a potential selection bias, the study sample was constructed by stratified sampling based on age, sex, and region of residence. Collected data are described as absolute numbers and proportions according to sex, age groups, region of residence, number of inhabitants in resident town/city, and attained education. Prevalence and severity of anxiety and depressive symptoms were assessed by sex and age. Prevalence was calculated as population proportions. Severity was calculated as mean scores of GAD-7 and PHQ-9 with standard deviations (SD) by sex, in individual age groups. Univariate logistic regression was performed to assess the association between the two outcome variables, anxiety and depression-and independent variables, age, sex, size of residence (number of inhabitants), and education. The outcome variables were treated as dichotomous (no symptoms and mild symptoms = no anxiety/depression present; moderate to severe symptoms = anxiety/depression present). For the presence of anxiety/depression, a cutoff score of 10 or greater was used. Significance level (alpha) was 0.05. Data analyses were performed with Stata Statistical Software: Release 16, College Station, TX: StataCorp LLC.
The study on mental health during the COVID-19 pandemic in the Slovak Republic used the data of 1501 survey respondents. Sociodemographic characteristics and subjective perception of overall and mental health are presented in Table 1. The study group was comprised of 48.00% of males and 52.00% of females, coming from all age groups of 15 years and older, proportionally to the general population. The most frequent category according to the size of residents was 1000-4999 inhabitants (29.51%) and 20000-99999 (26.32%). The most frequent completed education was secondary, with A-level (34.91%) and without (31.85%). The most frequent answer in perception of overall and mental health was good (41.84% and 42.57%, respectively) and very good (23.85% and 26.32%, respectively).
| Males | Females | Total | |||||
| n | % | n | % | n | % | ||
| Age categories | 15-25 yr | 69 | 9.57 | 201 | 25.77 | 270 | 17.99 |
| 26-35 yr | 174 | 24.13 | 139 | 17.82 | 313 | 20.85 | |
| 36-45 yr | 150 | 20.80 | 120 | 15.38 | 270 | 17.99 | |
| 46-55 yr | 132 | 18.31 | 114 | 14.62 | 246 | 16.39 | |
| 56-69 yr | 138 | 19.14 | 118 | 15.13 | 256 | 17.06 | |
| 70+ yr | 58 | 8.04 | 88 | 11.28 | 146 | 9.73 | |
| Size of residence (No. of inhabitants) | < 1000 | 113 | 15.67 | 119 | 15.26 | 232 | 15.46 |
| 1000-4999 | 190 | 26.35 | 253 | 32.44 | 443 | 29.51 | |
| 5000-19999 | 109 | 15.12 | 133 | 17.05 | 242 | 16.12 | |
| 20000-99999 | 202 | 28.02 | 193 | 24.74 | 395 | 26.32 | |
| 100000+ | 107 | 14.84 | 82 | 10.51 | 189 | 12.59 | |
| Education | Primary | 73 | 10.12 | 137 | 17.56 | 210 | 13.99 |
| Secondary without A-level | 173 | 23.99 | 305 | 39.10 | 478 | 31.85 | |
| Secondary with A-level | 349 | 48.40 | 175 | 22.44 | 524 | 34.91 | |
| University | 126 | 17.48 | 163 | 20.90 | 289 | 19.25 | |
| Overall health | Excellent | 61 | 8.46 | 53 | 6.79 | 114 | 7.59 |
| Very good | 158 | 21.91 | 200 | 25.64 | 358 | 23.85 | |
| Good | 318 | 44.11 | 310 | 39.74 | 628 | 41.84 | |
| Fair | 143 | 19.83 | 164 | 21.03 | 307 | 20.45 | |
| Poor | 41 | 5.69 | 53 | 6.79 | 94 | 6.26 | |
| Mental health | Excellent | 95 | 13.18 | 65 | 8.33 | 160 | 10.66 |
| Very good | 199 | 27.60 | 196 | 25.13 | 395 | 26.32 | |
| Good | 311 | 43.13 | 328 | 42.05 | 639 | 42.57 | |
| Fair | 86 | 11.93 | 158 | 20.26 | 244 | 16.26 | |
| Poor | 30 | 4.16 | 33 | 4.23 | 63 | 4.20 | |
| Total | 721 | 100.00 | 780 | 100.00 | 1501 | 100.00 | |
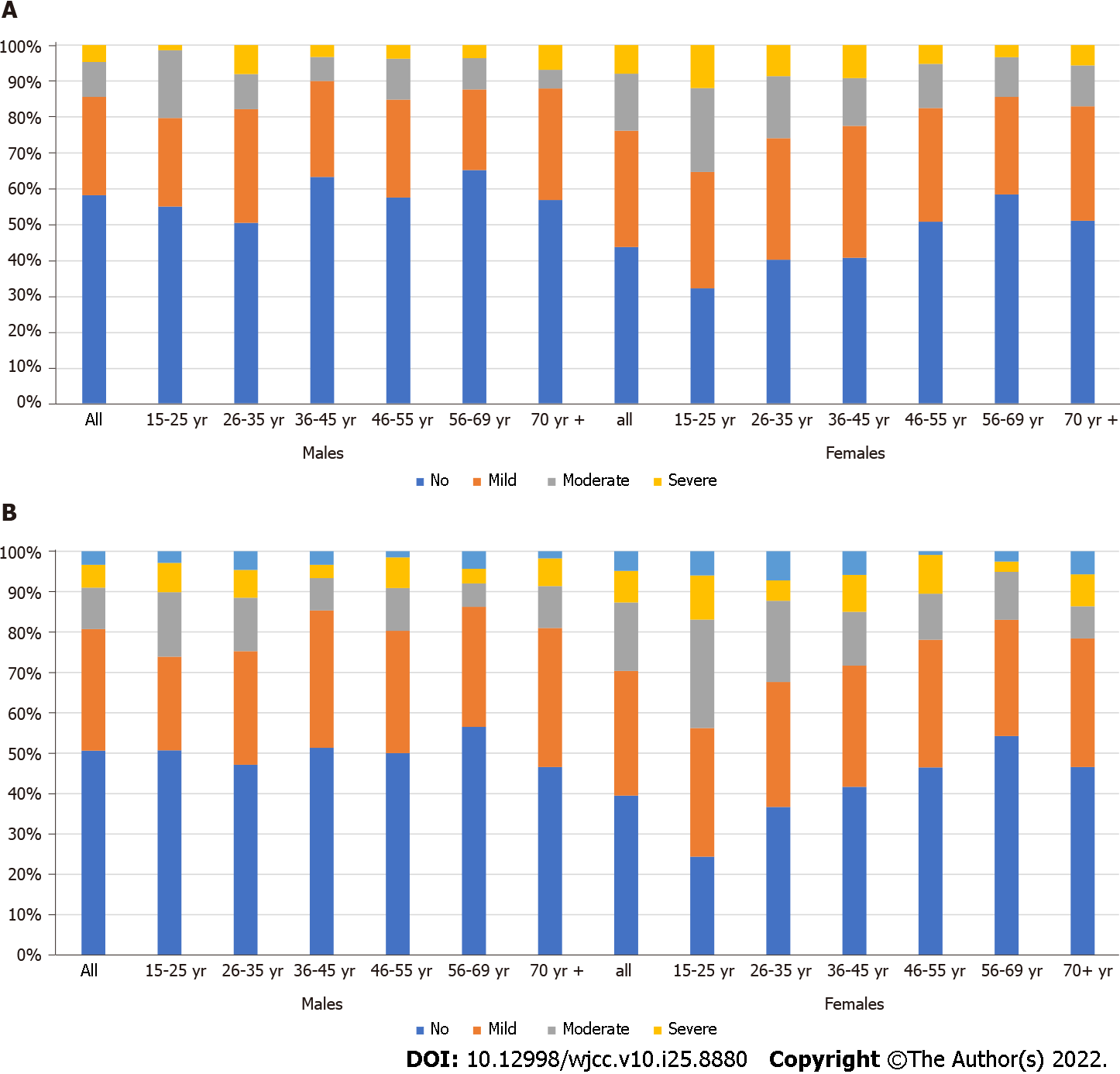
Figure 1 presents the proportions of symptoms of anxiety and depression by severity in males and females, in individual age groups. Anxiety was present in 19.32% and depression in 24.65% of the study group. Both disorders were more common in females. More than half (58.00%) of males vs 44.00% of females had no symptoms of anxiety and 51.00% of males vs 39.00% of females had no symptoms of depression. Around 15.00% of males and 24.00% of females had moderate to severe anxiety and 19.00% of males and 30.00% of females had moderate to severe depression.
The presence of symptoms of anxiety and depression also varied by age. The largest proportion of males and females without any symptoms of anxiety was in the age group 55-69 years old (65.22% of males and 58.47% of females). Similarly, the largest proportion of males and females without any symptoms of depression was also in the age group of 55-69 years old (56.52% of males and 54.24% of females). Moderate to severe anxiety was the most common in males in the age groups of 15-25 years old (20.29%) and 26-35 years old (17.82%). In females, it was the most common in the age groups of 15-25, 26-35, and 36-45 years old (35.32%, 25.9%, and 22.5%, respectively), as well as in the oldest age group of 70 + (17.04%). Moderate to severe depression was the most common in the youngest males (15-25 years old; 26.09%) and in the subsequent group (26-35 years old; 24.72%). Females had symptoms of moderate to severe depression more frequently – 43.79% in the youngest age group of 15-25 years old and 32.37% in the age group of 26-35 years old. Mean scores of anxiety and depression by age groups and sex are presented in Table 2.
| Anxiety | Depression | |||||||||||
| Males | Females | Total | Males | Females | Total | |||||||
| mean | SD | mean | SD | mean | SD | mean | SD | mean | SD | mean | SD | |
| 15-25 yr | 5.13 | 4.47 | 7.55 | 5.27 | 6.93 | 5.17 | 6.39 | 5.70 | 9.34 | 6.07 | 8.59 | 6.10 |
| 26-35 yr | 5.40 | 5.21 | 6.45 | 5.18 | 5.87 | 5.22 | 6.64 | 6.07 | 7.90 | 6.14 | 7.20 | 6.12 |
| 36-45 yr | 4.09 | 4.30 | 6.42 | 5.30 | 5.12 | 4.90 | 5.73 | 5.26 | 7.30 | 5.91 | 6.43 | 5.60 |
| 46-55 yr | 4.78 | 4.49 | 5.34 | 4.93 | 5.04 | 4.70 | 6.09 | 5.21 | 6.44 | 5.12 | 6.25 | 5.16 |
| 56-69 yr | 4.09 | 4.44 | 4.58 | 4.45 | 4.31 | 4.44 | 5.03 | 5.37 | 5.36 | 4.91 | 5.18 | 5.16 |
| 70+ yr | 4.60 | 4.37 | 5.23 | 4.90 | 4.98 | 4.69 | 6.29 | 5.08 | 6.57 | 5.79 | 6.46 | 5.50 |
| Total | 4.67 | 4.63 | 6.15 | 5.14 | 5.44 | 4.96 | 5.99 | 5.52 | 7.43 | 5.87 | 6.74 | 5.75 |
Sample mean score for anxiety measured by GAD-7 was 5.44 (SD = 4.96). Females had higher scores than males (6.15, SD = 5.14 vs 4.67, SD = 4.63). The youngest females of 15-24 years of age had the highest score (7.55, SD = 5.27) among all age groups, for both sexes.
Sample mean score for depressive symptoms measured by PHQ-9 was 6.74 (SD = 5.75). As in the case of anxiety symptoms, the highest score (9.34, SD = 6.07) was observed in the youngest females of 15-25 years of age.
We have assessed the association between the presence of the symptoms of anxiety or depression and age, sex, size of residence, and education by univariate regression. Anxiety/depressive symptoms were evaluated as present (moderate to severe) or not (none or mild symptoms). The outcomes of the analysis are found in Table 3. Younger age (15-25 years old) was statistically significantly associated with the presence of anxiety or depressive symptoms [odds ratio (OR): 1.69, 95%CI: 1.16-2.45 and OR: 1.65, 95%CI: 1.17-2.34, respectively] compared to the reference category of 26-35 years old, as well as being female (OR: 1.86, 95%CI: 1.42-2.42 and OR: 1.76, 95%CI: 0.20-0.29, respectively) compared to being male. Having primary education was significantly associated with symptoms of both anxiety and depression (OR: 1.66, 95%CI: 1.08-2.54 and OR: 1.65, 95%CI: 1.16-2.63, respectively) compared to university education. For anxiety, living in a big city of 100000 inhabitants and more was a protective factor (OR: 0.59, 95%CI: 0.36-0.96).
| Anxiety | Depression | Anxiety and depression | |||||
| OR | 95%CI | OR | 95%CI | OR | 95%CI | ||
| Age categories | 15-25 yr | 1.69b | 1.16-2.45 | 1.65b | 1.17-2.34 | 1.91b | 1.29-2.84 |
| 26-35 yr | Ref. | Ref. | Ref. | ||||
| 36-45 yr | 0.68 | 0.44-1.035 | 0.67a | 0.46-0.98 | 0.64 | 0.40-1.03 | |
| 46-55 yr | 0.71 | 0.46-1.099 | 0.67a | 0.45-0.99 | 0.67 | 0.41-1.08 | |
| 56-69 yr | 0.56a | 0.35-0.88 | 0.46c | 0.30-0.70 | 0.54 | 0.33-0.89 | |
| 70+ yr | 0.65 | 0.38-1.10 | 0.66 | 0.41-1.06 | 0.63 | 0.35-1-13 | |
| Sex (male = ref.) | Females | 1.86c | 1.42-2.42 | 1.76c | 0.20-0.29 | 1.72c | 1.29-2.29 |
| Size of residence | 1000-4999 | Ref. | Ref. | Ref. | |||
| < 1000 | 1.19 | 0.81-1.76 | 1.17 | 0.82-1.66 | 1.15 | 0.76-1.73 | |
| 5000-19999 | 0.82 | 0.55-1.24 | 0.81 | 0.56-1.17 | 0.80 | 0.51-1.24 | |
| 20000-99000 | 1.09 | 0.78-1.52 | 0.91 | 0.66-1.24 | 0.98 | 0.68-1-41 | |
| 100000+ | 0.59a | 0.36-0.96 | 0.66 | 0.44-1.01 | 0.49a | 0.28-0.84 | |
| Education | Primary | 1.66a | 1.08-2.54 | 1.75b | 1.16-2.63 | 2.01b | 1.26-3.20 |
| Secondary | 0.98 | 0.67-1.43 | 1132400 | 0.92-1.86 | 1.19 | 0.78-1.82 | |
| Secondary A | 0.97 | 0.67-1.41 | 42370,00 | 0.82-1.64 | 1.12 | 0.74-1.70 | |
| University | Ref. | Ref. | Ref. | ||||
We have also assessed the group that had both moderate to severe symptoms of anxiety and depression at the same time. This condition was met by 236 respondents (15.72%), the majority (149) of whom were women. A significant association was confirmed with younger age (15-25 years old) (OR: 1.91 95%CI: 1.29-2.84), being female (OR: 1.72, 95%CI: 1.29-2.29), and having primary education (OR: 2.01, 95%CI: 1.26-3.20). Living in a city of 100000 and more inhabitants was for this group (joint presence of depression and anxiety) a significantly protective factor (OR: 0.49, 95%CI: 0.28-0.84).
Our study provided information about the state of mental health of the general population in the Slovak Republic observed in the summer of 2021 during the beginning of the third wave of the COVID-19 pandemic.
The virus SARS-CoV-2 has a direct effect on physical and mental health. The impact of the viral infection on physical health is complex and described elsewhere. The mental health in COVID-19 patients is characterized by an increased incidence of the first diagnosis of mental disorder within 90 d after the infection[19].
The indirect effect of the spread of the virus is caused by the impact of implemented measures on the society. The impact is caused by the prolonged feelings of fear of contagion, social isolation, uncertainty, and economic instability. Available evidence shows common prevalence of anxiety and depressive symptoms in the global general population during various phases of the COVID-19 pandemic.
A systematic review and meta-analysis by Nochaiwong et al[5] that summarized information from 32 countries presented a pooled prevalence of 26.90% for anxiety and 28.00% for depression with a great variability among the included studies. Our results observed in the Slovak Republic showed anxiety in 19.32% and depression in 24.65% of the population. The difference between our results and the pooled data from the systematic review is explainable by the different time periods-the systematic review covered the studies published in the first phase of the pandemic while our study was implemented in the summer of 2021. For the assessment of the symptoms, various instruments were used in the studies included in the systematic review and that contributes to the difference with our results.
When we compare the results of our survey with surveys that used the same instruments (GAD-7 and PHQ-9) for the estimate of prevalence of depressive and anxiety symptoms during the COVID-19 pandemic, we see similar results. Hyland et al[20] reported a prevalence of 20.00% for anxiety and 22.80% for depression in the general population of the Republic of Ireland in the first week of nationwide quarantine measures in 2020. A survey of the general adult population in Germany in comparable period to our study (summer 2021) presented a prevalence of anxiety in 13.40% and prevalence of depression in 20.00% of the population[21]. Some country results report higher observed rates of anxiety and depression.
An online survey implemented in the spring of 2020 in Kosovo observed 35.60% of population having depressive symptoms[22]. A study by Benatov et al[23] reported the prevalence of anxiety and depression in Germany, Israel, Poland, and Slovenia, measured twice during the COVID-19 pandemic. The second measurement in May and June 2021 corresponds closely with the time of implementation of our study. At that time point, the study conducted in Germany found that 31.58% of the population reported symptoms of anxiety and 42.82% symptoms of depression, in Israel 20.09% of the population had symptoms of anxiety and 29.44% symptoms of depression, in Poland 38.12% of the population had symptoms of anxiety and 42.15% of the population had symptoms of depression, and in Slovenia 21.58% of the population had symptoms of anxiety and 22.97% of the population had symptoms of depression.
Looking outside Europe, in United States adults surveyed in the spring of 2021, depressive symptoms were observed in 32.80% of the population, while a study conducted in the adult population of Canada in March 2020 found that 47.20% of the population had symptoms of anxiety and 44.10% had symptoms of depression. Adult Australians surveyed in the spring of 2020 had symptoms of anxiety present in 55.10% and symptoms of depression in 47.70% of the population[24-26].
A survey in Hong Kong carried out in April and May 2020 revealed that 14.00% of the population had symptoms of anxiety and 19.00% of the population had symptoms of depression[27]. The general population in Mexico had symptoms of anxiety in 20.80% and symptoms of depression in 27.50% of the population[28].
Several studies looked specifically at symptoms of anxiety and depression in professional groups serving on the frontline during the COVID-19 pandemic, such as healthcare workers[11,29] or university students[10,30], with varied results.
Age and sex made a difference in the prevalence of anxiety and depressive symptoms. In our study group, 15.00% of the males had symptoms of moderate to severe anxiety compared to 24.00% of the females. In the above-mentioned Australian survey, it was 14.00% of the males and 22.00% of the females. One fifth (19.00%) of Slovak males and 30.00% of females had moderate to severe depression, whereas in the Australian study the figures were 20.00% of males and 26.00% of females[26]. A higher prevalence and higher intensity of depressive and anxiety symptoms observed by higher mean scores in women can have various explanations. First, there is established evidence that depression and anxiety are more frequently found in women. Second, the type of psychosocial burden as the one that the COVID-19 pandemic produces, affects more females than males - commonly they are the family members who are compelled to stay at home with children during online schooling, resulting in an extra burden and the eventual decrease of financial income.
In our survey, we observed the highest prevalence and severity of depressive and anxiety symptoms in young people and the lowest in the older adults. The younger adults in the 15-24 years age group, especially women, had the highest rates of anxiety and depression present and the highest mean scores of both GAD-7 and PHQ-9. The regression analysis confirmed a significant association between the presence of anxiety or depression and being in the youngest age category (OR: 1.69, 95%CI: 1.16-2.45 and OR: 1.65, 95%CI: 1.17-2.34, respectively). For those having both anxiety and depression, the association with young age was even stronger (OR: 1.91, 95%CI: 1.29-2.84). These findings are consistently in accordance with the results of the studies from other countries carried out on different continents during the COVID-19 pandemic - younger age was found to be significantly associated with higher levels of both anxiety and depression as compared to older age categories[23,25,31-33].
During the COVID-19 pandemic, cross-sectional online surveys indicated that older adults were less psychologically distressed than the younger ones. A longitudinal study revealed that COVID-19 in the elderly in comparison with young adults did not have a major impact resulting in feelings of loneliness and dissatisfaction with life. Altogether, research studies suggested that older age may act as a buffer against the COVID-19-related impact on mental health[34]. The older adults’ ability to adapt to adversity varies, depending on cultural, social, economic, and other individual factors. The long-term impact of COVID-19 therefore remains to be evaluated by prospective, longitudinal studies.
We have explored the association of education with the depressive and anxiety symptoms. In our study we found that lower than secondary education significantly increased the risk of both anxiety and depressive symptoms. Having lower educational attainment may cause impaired access to valid information and increase feelings of doubt and insecurity[35]. The size of residence did not play a major role in our results, although respondents living in the biggest cities of more than 100 thousand inhabitants seemed to be protected against the severe mental health impact of COVID-19 compared to those living in smaller towns.
The main implication of the study is that a large proportion of the Slovak population experiences symptoms of anxiety and/or depression. This fact emphasizes the importance of further research regarding the population’s mental health using broad spectrum diagnostic tools that are able to diagnose the most common disorders. At the same time, it is important to assess the use of mental health care services and to identify the gaps. The study results can serve as an important information basis for the development of effective mental health policies, consisting of preventive programs, and early detection and effective treatment services. Mental health awareness raising implemented by governmental as well as non-governmental organizations is crucial to improve the quality of life at the individual level. Employers need to prioritize promotion and protection of mental health at work in order to provide safe and sound working environment. At the state level, the barriers in the access to the mental health services need to be identified and cleared away. The study results provide a strong argument for the necessity of the mental health reform currently being shaped in the Slovak Republic.
Our study had its strengths and limitations. The main strength is that it brought knowledge of the mental health status of the population during the COVID-19 pandemic and identified the population groups at the highest risk of mental health problems. The limitations of the study were several. First, a population survey of mental health has not been carried out in the Slovak Republic before, therefore we do not possess the data needed to ascertain the prevalence trend.
The survey was mainly internet based, therefore people with limited internet access or technological literacy might be underrepresented. We have relied on the participants’ self-report of depressive and anxiety symptoms.
Last, the study was conducted in the summer of 2021, that is at the time of a certain relief from the greatest burden of the pandemic after the second wave, thus, the results may be a snapshot of the good times’ situation.
The comparisons with results of similar studies from other countries need to be done with extra caution. We need to take into account that the different social, cultural, political, and economic conditions have a complex effect on the population’s mental health.
As the COVID-19 pandemic spread across the world, it has brought with it a considerable degree of fear and uncertainty that impacted various aspects of societal life, including mental health. Knowing the mental health status of the population is crucial for the implementation of interventions and adequate public policies in order to mitigate the detrimental effects of the pandemic.
Great mental health care gap was observed in the Slovak Republic previously, leaving many people with depressive and anxiety disorders without treatment. This is caused by the fact that mental health care in the country is provided mainly by psychiatrists and private psychologists. General practitioners do not participate in the mental health care, therefore the access is very limited. Effective preventive programs are not implemented. The COVID-19 pandemic revealed the extent of society’s mental health crisis and it became a public and political issue.
The results of our study indicate that perceived anxiety and depressive symptoms are frequent in the population of the Slovak Republic during the COVID-19 pandemic. Both the prevalence rates and mean scores for anxiety and depressive symptoms are highest in those under 25 years and in females. Older age and larger cities of residence seem to provide a bit of a buffer and lower education is associated with a higher incidence of anxiety and depressive symptoms. These results provide a strong argument for the need of urgent establishment of the Community Mental Health Centers and Crisis Intervention Centers, as well as case management provided by multidisciplinary teams and combination of psychiatric treatment with psychotherapy, psycho-social rehabilitation and social care, as planned within the launched mental health care reform in the Slovak Republic.
Our study, together with international scientific outcomes, invites new research to further explore the relationships between the COVID-19 pandemic and population’s mental health with an emphasis on long-term consequences.
Monitoring of population’s mental health is essential for knowing the distribution of mental well-being and mental disorders in the society. Mental disorders constitute a large burden, and they are the leading cause of disability. The information provided by such monitoring should serve as a database for evidence-based mental health policy, for setting the effective preventive measures and curative services.
As there is abundant evidence that the population’s mental health is largely affected by crisis situations and the impact of the coronavirus disease 2019 (COVID-19) pandemic on the general population of the Slovak Republic has not yet been studied, we have conducted a study on the prevalence of depressive and anxiety symptoms.
The aim of the current study was to assess the mental health of the general Slovak population aged 15 years and older in the summer of 2021 (beginning of the Delta wave of the COVID-19 pandemic) by determining the prevalence of depressive and anxiety symptoms.
A cross-sectional study was implemented in July 2021 during the COVID-19 pandemic in the Slovak Republic to assess the prevalence of depressive and anxiety symptoms. The study was performed in a sample of 1501 respondents. The symptoms of anxiety were assessed using the 7-item instrument generalized anxiety disorder (GAD-7) and the symptoms of depression were assessed by the 9-item instrument patient health questionnaire (PHQ-9) instruments.
Anxiety was present in 19.32% and depression in 24.65% of the study group. Both disorders were more common in females. Around 15.00% of males and 24.00% of females had moderate to severe anxiety, and 19.00% of males and 30.00% of females had moderate to severe depression. Moderate to severe anxiety was the most common in males in the age groups of 15-25 years old (20.29%) and 26-35 years old (17.82%). In females, it was the most common in the age groups of 15-25, 26-35, and 36-45 years old (35.32%, 25.9%, and 22.5%, respectively), as well as in the oldest age group of 70+ (17.04%). Moderate to severe depression was the most common in youngest males (15-25 years old; 26.09%) and in the subsequent group (26-35 years old; 24.72%). Younger age (15-25 years old) was statistically significantly associated with the presence of anxiety or depressive symptoms, as well as being female and having primary education.
The results of our study indicate that perceived anxiety and depressive symptoms are frequent in the population of the Slovak Republic during the COVID-19 pandemic. Both the prevalence rates and mean scores for anxiety and depressive symptoms are highest in those under 25 years and in females. These results, together with great mental health care gap observed in the Slovak Republic previously, call for the need of urgent implementation of the mental health care reform that is under way in the country.
Our study, together with international scientific outcomes, invites new research to further explore the relationships of COVID-19 pandemic and population’s mental health with an emphasis on long-term consequences.
The authors would like to acknowledge the Slovak non-governmental organization League for Mental Health (LMH) that initiated the survey that provided the data for this study. The LMH is active in mental health promotion and raising the awareness of mental health in the Slovak Republic for more than 20 years.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Psychiatry
Country/Territory of origin: Slovakia
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C, C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Laranjeira C, Portugal; Setiawati Y, Indonesia; Siddiqui SA, India S-Editor: Wang DM L-Editor: Wang TQ P-Editor: Wang DM
| 1. | GBD 2019 Mental Disorders Collaborators. Global, regional, and national burden of 12 mental disorders in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet Psychiatry. 2022;9:137-150. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 436] [Cited by in F6Publishing: 1119] [Article Influence: 559.5] [Reference Citation Analysis (0)] |
| 2. | Patel V, Chisholm D, Parikh R, Charlson FJ, Degenhardt L, Dua T, Ferrari AJ, Hyman S, Laxminarayan R, Levin C, Lund C, Medina Mora ME, Petersen I, Scott J, Shidhaye R, Vijayakumar L, Thornicroft G, Whiteford H; DCP MNS Author Group. Addressing the burden of mental, neurological, and substance use disorders: key messages from Disease Control Priorities, 3rd edition. Lancet. 2016;387:1672-1685. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 434] [Cited by in F6Publishing: 437] [Article Influence: 54.6] [Reference Citation Analysis (0)] |
| 3. | Brooks SK, Webster RK, Smith LE, Woodland L, Wessely S, Greenberg N, Rubin GJ. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020;395:912-920. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 9682] [Cited by in F6Publishing: 7558] [Article Influence: 1889.5] [Reference Citation Analysis (1)] |
| 4. | Daiane Borges M, Flávia JOA, Camila SST, Aline SR, Luís FSC-d-A, Amandeep S, Barreto ML. Effects of COVID-19 on Anxiety, Depression and Other Mental Health Issues: A worldwide scope review. 2020 Preprint. Available from: Research Square. [DOI] [Cited in This Article: ] |
| 5. | Nochaiwong S, Ruengorn C, Thavorn K, Hutton B, Awiphan R, Phosuya C, Ruanta Y, Wongpakaran N, Wongpakaran T. Global prevalence of mental health issues among the general population during the coronavirus disease-2019 pandemic: a systematic review and meta-analysis. Sci Rep. 2021;11:10173. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 294] [Cited by in F6Publishing: 253] [Article Influence: 84.3] [Reference Citation Analysis (0)] |
| 6. | Salari N, Hosseinian-Far A, Jalali R, Vaisi-Raygani A, Rasoulpoor S, Mohammadi M, Khaledi-Paveh B. Prevalence of stress, anxiety, depression among the general population during the COVID-19 pandemic: a systematic review and meta-analysis. Global Health. 2020;16:57. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1946] [Cited by in F6Publishing: 1639] [Article Influence: 409.8] [Reference Citation Analysis (0)] |
| 7. | Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16:606-613. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 21545] [Cited by in F6Publishing: 23873] [Article Influence: 1038.0] [Reference Citation Analysis (0)] |
| 8. | Spitzer RL, Kroenke K, Williams JB, Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006;166:1092-1097. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 11947] [Cited by in F6Publishing: 14941] [Article Influence: 830.1] [Reference Citation Analysis (0)] |
| 9. | Halperin SJ, Henderson MN, Prenner S, Grauer JN. Prevalence of Anxiety and Depression Among Medical Students During the Covid-19 Pandemic: A Cross-Sectional Study. J Med Educ Curric Dev. 2021;8:2382120521991150. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 61] [Cited by in F6Publishing: 72] [Article Influence: 24.0] [Reference Citation Analysis (0)] |
| 10. | Naser AY, Dahmash EZ, Al-Rousan R, Alwafi H, Alrawashdeh HM, Ghoul I, Abidine A, Bokhary MA, Al-Hadithi HT, Ali D, Abuthawabeh R, Abdelwahab GM, Alhartani YJ, Al Muhaisen H, Dagash A, Alyami HS. Mental health status of the general population, healthcare professionals, and university students during 2019 coronavirus disease outbreak in Jordan: A cross-sectional study. Brain Behav. 2020;10:e01730. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 190] [Cited by in F6Publishing: 192] [Article Influence: 48.0] [Reference Citation Analysis (0)] |
| 11. | Zhang WR, Wang K, Yin L, Zhao WF, Xue Q, Peng M, Min BQ, Tian Q, Leng HX, Du JL, Chang H, Yang Y, Li W, Shangguan FF, Yan TY, Dong HQ, Han Y, Wang YP, Cosci F, Wang HX. Mental Health and Psychosocial Problems of Medical Health Workers during the COVID-19 Epidemic in China. Psychother Psychosom. 2020;89:242-250. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 801] [Cited by in F6Publishing: 807] [Article Influence: 201.8] [Reference Citation Analysis (0)] |
| 12. | Taquet M, Geddes JR, Husain M, Luciano S, Harrison PJ. 6-month neurological and psychiatric outcomes in 236 379 survivors of COVID-19: a retrospective cohort study using electronic health records. Lancet Psychiatry. 2021;8:416-427. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 901] [Cited by in F6Publishing: 1061] [Article Influence: 353.7] [Reference Citation Analysis (0)] |
| 13. | Brazinova A, Hasto J, Levav I, Pathare S. Mental Health Care Gap: The Case of the Slovak Republic. Adm Policy Ment Health. 2019;46:753-759. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 3] [Cited by in F6Publishing: 3] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 14. | Rutkowska A, Liska D, Cieślik B, Wrzeciono A, Broďáni J, Barcalová M, Gurín D, Rutkowski S. Stress Levels and Mental Well-Being among Slovak Students during e-Learning in the COVID-19 Pandemic. Healthcare (Basel). 2021;9. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 10] [Cited by in F6Publishing: 12] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 15. | Gavurova B, Ivankova V, Rigelsky M, Mudarri T, Miovsky M. Somatic Symptoms, Anxiety, and Depression Among College Students in the Czech Republic and Slovakia: A Cross-Sectional Study. Front Public Health. 2022;10:859107. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 5] [Cited by in F6Publishing: 5] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 16. | Hajduk M, Dancik D, Januska J, Strakova A, Turcek M, Heretik A, Pecenak J. Depression and anxiety among College Students in Slovakia - Comparison of the Year 2018 and during COVID-19 pandemic. Bratisl Lek Listy. 2022;123:44-49. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 6] [Cited by in F6Publishing: 7] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 17. | Bisby MA, Karin E, Scott AJ, Dudeney J, Fisher A, Gandy M, Hathway T, Heriseanu AI, Staples L, Titov N, Dear BF. Examining the psychometric properties of brief screening measures of depression and anxiety in chronic pain: The Patient Health Questionnaire 2-item and Generalized Anxiety Disorder 2-item. Pain Pract. 2022;22:478-486. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 2] [Cited by in F6Publishing: 3] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 18. | Shevlin M, Butter S, McBride O, Murphy J, Gibson-Miller J, Hartman TK, Levita L, Mason L, Martinez AP, McKay R, Stocks TV, Bennett KM, Hyland P, Vallieres F, Valiente C, Vazquez C, Contreras A, Peinado V, Trucharte A, Bertamini M, Panzeri A, Bruno G, Granziol U, Mignemi G, Spoto A, Vidotto G, Bentall RP. Measurement invariance of the Patient Health Questionnaire (PHQ-9) and Generalized Anxiety Disorder scale (GAD-7) across four European countries during the COVID-19 pandemic. BMC Psychiatry. 2022;22:154. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 11] [Cited by in F6Publishing: 11] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 19. | Taquet M, Luciano S, Geddes JR, Harrison PJ. Bidirectional associations between COVID-19 and psychiatric disorder: retrospective cohort studies of 62 354 COVID-19 cases in the USA. Lancet Psychiatry. 2021;8:130-140. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 736] [Cited by in F6Publishing: 805] [Article Influence: 268.3] [Reference Citation Analysis (0)] |
| 20. | Hyland P, Shevlin M, McBride O, Murphy J, Karatzias T, Bentall RP, Martinez A, Vallières F. Anxiety and depression in the Republic of Ireland during the COVID-19 pandemic. Acta Psychiatr Scand. 2020;142:249-256. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 294] [Cited by in F6Publishing: 283] [Article Influence: 70.8] [Reference Citation Analysis (0)] |
| 21. | Hajek A, König HH. The Prevalence and Correlates of Probable Major Depressive Disorder and Probable Generalized Anxiety Disorder during the COVID-19 Pandemic. Results of a Nationally Representative Survey in Germany. Int J Environ Res Public Health. 2021;18. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 9] [Cited by in F6Publishing: 3] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 22. | Fanaj N, Mustafa S. Depression Measured by PHQ-9 in Kosovo during the COVID-19 Outbreak: An Online Survey. Psychiatr Danub. 2021;33:95-100. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 5] [Cited by in F6Publishing: 5] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 23. | Benatov J, Ochnik D, Rogowska AM, Arzenšek A, Mars Bitenc U. Prevalence and Sociodemographic Predictors of Mental Health in a Representative Sample of Young Adults from Germany, Israel, Poland, and Slovenia: A Longitudinal Study during the COVID-19 Pandemic. Int J Environ Res Public Health. 2022;19. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 23] [Cited by in F6Publishing: 29] [Article Influence: 14.5] [Reference Citation Analysis (0)] |
| 24. | Ettman CK, Cohen GH, Abdalla SM, Sampson L, Trinquart L, Castrucci BC, Bork RH, Clark MA, Wilson I, Vivier PM, Galea S. Persistent depressive symptoms during COVID-19: a national, population-representative, longitudinal study of U.S. adults. Lancet Reg Health Am. 2022;5:100091. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 24] [Cited by in F6Publishing: 75] [Article Influence: 25.0] [Reference Citation Analysis (0)] |
| 25. | Nwachukwu I, Nkire N, Shalaby R, Hrabok M, Vuong W, Gusnowski A, Surood S, Urichuk L, Greenshaw AJ, Agyapong VIO. COVID-19 Pandemic: Age-Related Differences in Measures of Stress, Anxiety and Depression in Canada. Int J Environ Res Public Health. 2020;17. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 137] [Cited by in F6Publishing: 156] [Article Influence: 39.0] [Reference Citation Analysis (0)] |
| 26. | Stocker R, Tran T, Hammarberg K, Nguyen H, Rowe H, Fisher J. Patient Health Questionnaire 9 (PHQ-9) and General Anxiety Disorder 7 (GAD-7) data contributed by 13,829 respondents to a national survey about COVID-19 restrictions in Australia. Psychiatry Res. 2021;298:113792. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 14] [Cited by in F6Publishing: 24] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 27. | Choi EPH, Hui BPH, Wan EYF. Depression and Anxiety in Hong Kong during COVID-19. Int J Environ Res Public Health. 2020;17. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 563] [Cited by in F6Publishing: 432] [Article Influence: 108.0] [Reference Citation Analysis (0)] |
| 28. | Galindo-Vázquez O, Ramírez-Orozco M, Costas-Muñiz R, Mendoza-Contreras LA, Calderillo-Ruíz G, Meneses-García A. Symptoms of anxiety, depression and self-care behaviors during the COVID-19 pandemic in the general population. Gac Med Mex. 2020;156:298-305. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 12] [Cited by in F6Publishing: 20] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 29. | Peccoralo LA, Pietrzak RH, Feingold JH, Syed S, Chan CC, Murrough JW, Kaplan C, Verity J, Feder A, Charney DS, Southwick SM, Ripp JA. A prospective cohort study of the psychological consequences of the COVID-19 pandemic on frontline healthcare workers in New York City. Int Arch Occup Environ Health. 2022;. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 5] [Cited by in F6Publishing: 16] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 30. | Wang X, Hegde S, Son C, Keller B, Smith A, Sasangohar F. Investigating Mental Health of US College Students During the COVID-19 Pandemic: Cross-Sectional Survey Study. J Med Internet Res. 2020;22:e22817. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 376] [Cited by in F6Publishing: 546] [Article Influence: 136.5] [Reference Citation Analysis (7)] |
| 31. | Owens M, Townsend E, Hall E, Bhatia T, Fitzgibbon R, Miller-Lakin F. Mental Health and Wellbeing in Young People in the UK during Lockdown (COVID-19). Int J Environ Res Public Health. 2022;19. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 7] [Cited by in F6Publishing: 7] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 32. | Özdin S, Bayrak Özdin Ş. Levels and predictors of anxiety, depression and health anxiety during COVID-19 pandemic in Turkish society: The importance of gender. Int J Soc Psychiatry. 2020;66:504-511. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 854] [Cited by in F6Publishing: 646] [Article Influence: 161.5] [Reference Citation Analysis (0)] |
| 33. | Solomou I, Constantinidou F. Prevalence and Predictors of Anxiety and Depression Symptoms during the COVID-19 Pandemic and Compliance with Precautionary Measures: Age and Sex Matter. Int J Environ Res Public Health. 2020;17. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 383] [Cited by in F6Publishing: 303] [Article Influence: 75.8] [Reference Citation Analysis (0)] |
| 34. | Parlapani E, Holeva V, Nikopoulou VA, Kaprinis S, Nouskas I, Diakogiannis I. A review on the COVID-19-related psychological impact on older adults: vulnerable or not? Aging Clin Exp Res. 2021;33:1729-1743. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 16] [Cited by in F6Publishing: 20] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 35. | Fancourt D, Steptoe A, Bu F. Trajectories of anxiety and depressive symptoms during enforced isolation due to COVID-19 in England: a longitudinal observational study. Lancet Psychiatry. 2021;8:141-149. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 504] [Cited by in F6Publishing: 580] [Article Influence: 193.3] [Reference Citation Analysis (0)] |