Published online Aug 26, 2022. doi: 10.12998/wjcc.v10.i24.8667
Peer-review started: March 15, 2022
First decision: April 19, 2022
Revised: April 20, 2022
Accepted: July 16, 2022
Article in press: July 16, 2022
Published online: August 26, 2022
Recently, two naval pilots in a two-seat trainer jet were forced to eject urgently due to sudden mechanical failure during night-time training. They were both successfully rescued and sent to the hospital for emergency treatment. In this study, we investigate their ejection injuries and recovery process.
We analyzed the clinical data of the traumatic condition and recovery process from ejection injuries of two pilots who ejected from a failed trainer jet and survived. After being successfully rescued and sent to the hospital, they were diagnosed with multiple ejection injuries, including eye trauma, limb bone and joint injury, rib and spine injury, and so on. Both cases underwent fluid replacement, acid suppression, nutritional support, hemostasis, bone metabolism improvement, phlegm elimination, psychological measurement, blood circulation promotion and detumescence, physical therapy, and external fixation with braces for 1 mo before being discharged from hospital. They then recuperated in a sanatorium for 2 mo, and the related laboratory tests and supplementary examinations show that they recovered from all the above injuries. After successfully passing the psychological test and physical examination, they returned to flight duty 3 mo after ejection.
The causes and conditions of ejection injury in the pilots were very complex. Although they finally recovered quickly and were released, it also serves as a reminder that attention should be paid to pilots’ ejection and parachute training in order to significantly reduce ejection injury and improve the ejection success rate. In addition, air defense support personnel should strengthen search and rescue and on-site emergency measures, and locate and rescue pilots in distress as early as possible to reduce subsequent injuries.
Core Tip: The ejection injuries to pilots are usually very complex. We analyzed two pilots’ traumatic condition and recovery process after they were ejected from a failed trainer and survived. After being successfully rescued, they were diagnosed with multiple ejection injuries and underwent a series of treatments for 1 mo. They then recuperated for 2 mo, and the related tests and examinations show that they recovered from injuries. After passing the psychological test and physical examination, they successfully returned to flight duty. Attention should be paid to pilots’ ejection training in order to reduce ejection injury and improve the ejection success rate. In addition, aviation rescuers should strengthen search techniques to locate and rescue pilots in distress as early as possible to reduce injuries.
- Citation: Zeng J, Liu XP, Yi JC, Lu X, Liu DD, Jiang YQ, Liu YB, Tian JQ. Analysis of two naval pilots’ ejection injuries: Two case reports. World J Clin Cases 2022; 10(24): 8667-8672
- URL: https://www.wjgnet.com/2307-8960/full/v10/i24/8667.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i24.8667
Ejection is an important way for pilots to escape planes in case of emergency, but the incidence of injury accompanying ejection escape is also very high[1-3]. As the conditions of ejection injuries are complex and diverse, it is very important to study ejection injuries and take targeted first-aid measures to save the lives of pilots in distress[4].
Recently, two naval pilots in a two-seat trainer jet were forced to eject urgently due to sudden mechanical failure during night-time training. The flight speed during the ejection was about 700 km/h, which was within the flight envelope. The ejection mode was rocket-assisted through-canopy ejection. At the moment of ejection, they experienced transient loss of consciousness. They were both successfully rescued and sent to the hospital for emergency treatment. After being diagnosed with multiple ejection injuries, they recuperated in a sanatorium for 2 mo, and the related laboratory tests and supplementary examinations show that they recovered from their injuries. After successfully passing the psychological test and physical examination, they returned to flight duty 3 mo after ejection. Their injury conditions and recovery process are presented below.
Case 1: A male flight cadet in the front cabin, 20-years-old, with total flight time of 300 h, suffered from multiple injuries to the whole body 2 h after ejection.
Case 2: A male flight instructor in the rear cabin, 40-years-old, with total flight time of 1700 h (including 280 h in the current aircraft model), suffered from multiple injuries to the whole body 11 h after ejection.
Case 1: Due to mechanical failure, the pilot ejected and parachuted from the front cabin of the trainer jet with transient loss of consciousness. He had recovered consciousness by the time he landed. He experienced chest pain, back pain and other body pains, and limited movement of the right ankle. Two hours after ejection, he was found by the villagers and sent to the local hospital by ambulance.
Case 2: Due to mechanical failure, the pilot ejected and parachuted from the rear cabin of the trainer jet with transient loss of consciousness. He regained consciousness after landing. He felt pain all over his body and limited movement of the left knee. Eleven hours after ejection, he was found and sent to the local hospital by ambulance.
No other abnormal health conditions were reported in both cases.
Both cases had no specific history of genetic diseases.
Case 1: The pilot was found with blueness and bilateral swelling on the eyelids; a splinter hemorrhage in the right conjunctiva, and swelling and percussion pain (+) in the neck, back, and waist; tenderness (+) in the T3-T5 and T8 vertebral spinous process; slightly limited thoracic vertebral extension; tenderness (+) and percussion pain (+) in the right hypochondriac region; swelling in the right ankle, tenderness (+) in the right lateral ankle and posterior ankle, slightly limited varus, and right lower limb muscle strength 4 +; and multiple skin abrasions on the back, waist, and extremities.
Case 2: The pilot was found with bilateral edema of the eyelids and a small splinter hemorrhage in the right conjunctiva; multiple abrasions on the face, bilateral forearm and legs, and swelling and bruising on the posterior-lateral left thigh; cyanosis of the skin, and swelling, tenderness (+), and immobility around the left knee joint.
Case 1: Aspartate aminotransferase 53 U/L, procalcitonin 0.51 ng/mL, indirect bilirubin 22.65 μmol/L, creatine kinase 175 IU/L, C-reactive protein (CRP) 8.1 mg/L, phosphocreatine kinase isoenzyme 33 U/L, and lactate dehydrogenase 360 U/L.
Case 2: Creatine kinase 1133 IU/L, creatinine 101 μmol/L, CRP 22.5 mg/L, phosphocreatine kinase isoenzyme 22 U/L, and lactate dehydrogenase 277 U/L.
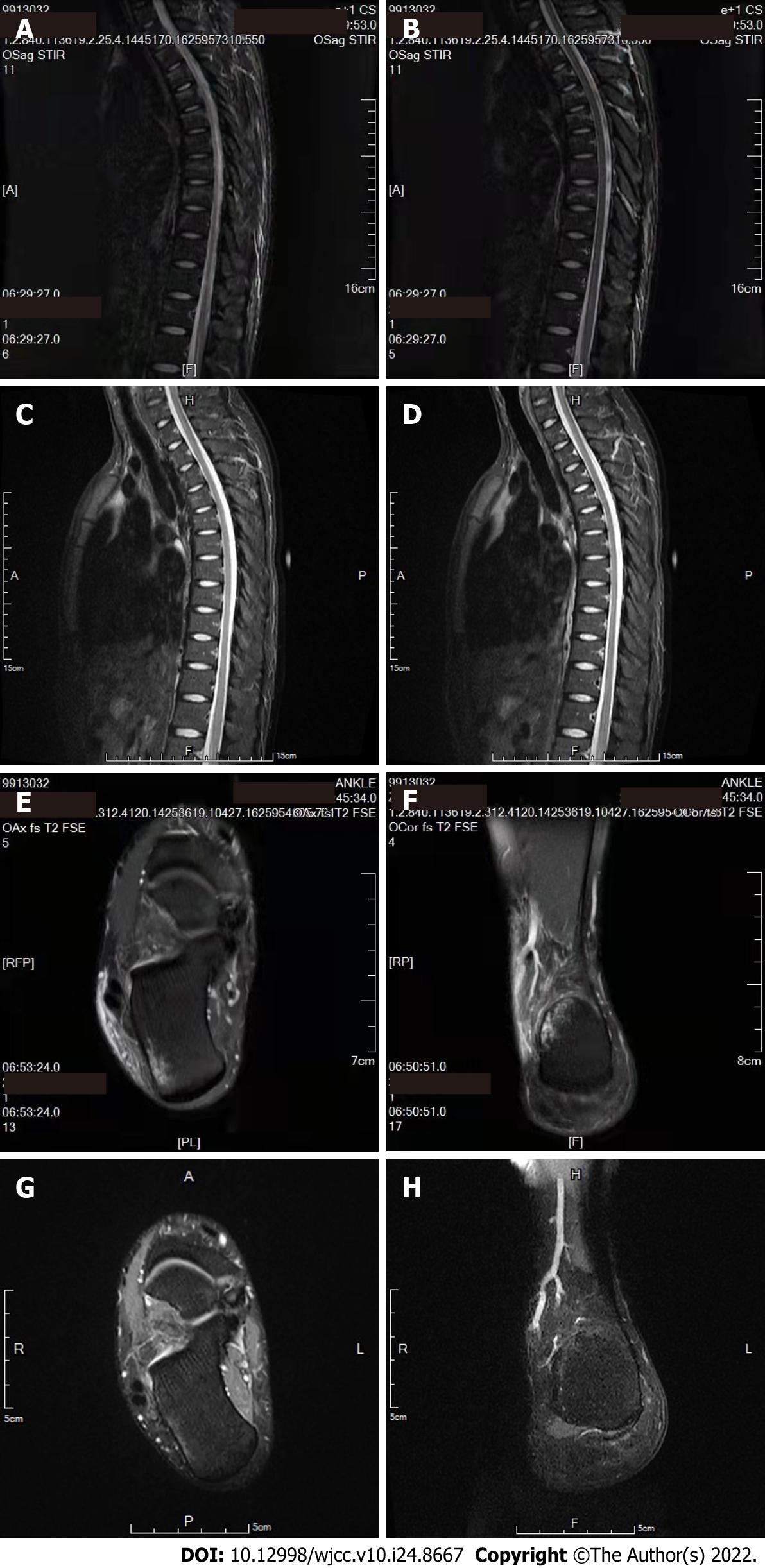
Case 1: Magnetic resonance imaging (MRI) showed: C3/4 and C4/5 intervertebral disc herniation; mild compression fractures of T3-T5 and T8 vertebral bodies; bone marrow edema of T1-T8 vertebral bodies and L5/S1 intervertebral disc herniation; laceration of anterior talofibular ligament of the right ankle; local Grade 1 injury of Achilles tendon of right ankle; bone marrow edema of right calcaneus; and soft tissue edema around right ankle. Chest computed tomography (CT) showed incomplete fractures of multiple right ribs (anterior ribs 5-9) (Figure 1A-D).
Case 2: MRI showed: Lumbar disc herniation of L3/4; thoracic T3 vertebral hemangioma.
Ocular trauma, subconjunctival hemorrhage (right); cervical disc herniation (C3/4, C4/5); multiple thoracic vertebral compression fractures (T3-T5, T8); incomplete fracture of multiple right ribs; Achilles tendon injury (right, Grade 1); laceration of anterior talofibular ligament of ankle (right); calcaneal contusion (right); and soft tissue injury in right ankle and lower back.
Ocular trauma, subconjunctival hemorrhage (right eye); left medial femoral condylar bone contusion with bone marrow edema; multiple injuries to posterior tendons and ligaments of left thigh; acute kidney injury; thoracic T3 vertebral hemangioma; and lumbar disc herniation (L3/4).
After admission, the two injured pilots were treated with fluid replacement, acid suppression, nutritional support, hemostasis, bone metabolism improvement, phlegm elimination, psychological measurement, blood circulation promotion and detumescence, physical therapy, and external fixation with braces for 1 mo before being discharged from hospital.
After discharge, they recuperated in a sanatorium for 2 mo, the related laboratory tests and supplementary examinations show that they recovered from all injuries. Psychological assessment: Healthy. Physical fitness test: Qualified. They were released 3 mo after the ejection (Figure 1E-H).
Congestive bilateral eyelid and right eyeball conjunctiva were potentially caused by the effects of continuous negative gravity (-G) conditions on visual function[5]. The analysis showed that both pilots were suspended upward when the danger occurred. At this time, -G caused blood to flow to the head, which led to the congestion of bulbar conjunctiva, increased the secretion of lacrimal glands, and caused eyelid edema and blurred vision. Continuous -G can also cause: (1) Changes in visual function; increased secretion of the lacrimal glands can lead to blurred vision; edema of the lower eyelid, shifting upward to cover the pupil and cause difficulty in opening the eyes, can lead to the temporary loss of vision; and conjunctiva rupture and hemorrhage, causing blood-stained tears to accumulate in the conjunctival sac, results in the redness of the visual field. The congested lower eyelid shifted upward to cover the pupil, and strong light irradiation led to the redness of visual field. Retinal circulation stagnation and hypoxia, and the lower eyelid covering the pupil, led to the loss of central vision; edema of the orbital tissue and disorder of the coordinated movement of the extraocular muscles led to diplopia; (2) Congestion in the reflux area of the superior vena cava can result in the congestion and edema of the neck and face, as well as subcutaneous hemorrhage points; (3) With the diaphragm in an upward position, ventilation blood flow imbalance can lead to dyspnea; (4) Increased intracranial pressure can lead to headache and distension of the head, as well as increased blood pressure; and (5) Increased carotid sinus pressure can lead to an abnormal heart rate.
Temporary loss of consciousness, spinal injury, head and neck injury and limb injury were likely due to the overload value during ejection, which may have reached about 20 G, with a high growth rate of G value and short action time. The ejection through the canopy increased the G value and G growth rate significantly. After ejection from the aircraft and before the parachute opens, the person-chair system or human body may rotate under the impact of the high-speed airflow. The inertial centrifugal force may cause equipment, such as oxygen masks, gloves, flight boots, and pistols to fall off, and the headband of the mask may injure the neck[4-6]. The high-speed airflow may also cause hypoxia and frostbite in pilots[3,4]. Both pilots experienced the transient loss of consciousness during ejection, and only recovered their consciousness during parachuting. The cadet in the front cabin had multiple thoracic vertebral compression and rib fractures, and a cervical disc herniation, while the instructor in the rear cabin had a cervical and lumbar disc herniation; it is considered that they were already displaced at the time of ejection. The mask and helmet caused minor injuries to the head and neck, and the cadet in the front cabin incurred neck strangulation and limb injury due to the displacement and collision of the limbs and loss of consciousness during ejection.
Parachute-opening injury is more common at the exerting parts of harness system, such as the scapula, chest and waist, and perineum, which can cause sternum, rib, spine, and limb fracture and dislocation, as well as visceral injuries[7]. The pilots presented multiple fractures to the right ribs, which was considered to have been caused by the parachutes opening. Meanwhile, parachuting is not excluded from being the cause of spinal injury in both patients.
Sprains and contusions to the lower limb joints and ligaments are mostly caused by landing. The cadet in the front cabin suffered from a right Achilles tendon injury; laceration of the anterior talofibular ligament of the right ankle; right calcaneal bone contusion; and soft tissue injury in the right ankle, back, and waist. The instructor in the back cabin suffered from left medial femoral condylar bone contusion with bone marrow edema, and multiple injuries to the posterior tendons and ligaments of the left thigh[8]. Moreover, the incident occurred in a jungle mountain area at night, so the poor visibility, more numerous obstacles, and improper landing posture could have aggravated the injuries. Both cases were found with abnormal enzyme labeling and elevated CRP at the time of admission, which were caused by muscle injury and systemic inflammatory reaction after injury. The instructor in the back cabin also showed abnormal creatinine and slightly increased urinary microproteins, which was related to his landing on the top of a mountain, longer rescue time, prolonged lack of water, and insufficient strength. The laboratory indexes all improved after active treatment.
The causes of ejection injury in these cases are complex. The two pilots carried out the ejection properly. Fortunately, they did not suffer from any visceral or fatal disability injuries, and recovered quickly and were released. However, it also serves as a reminder that attention should be paid to pilots’ ejection and parachute training. Before ejection, the flight parameters should be controlled within the ejection envelope (safe flying height and descent rate) as much as possible. The perfect mastery of ejection skills by pilots may contribute to significantly reduced ejection injury and improved ejection success rate[9,10]. Meanwhile, air defense support personnel should strengthen search and rescue and on-site emergency measures, and locate and rescue pilots in distress as quickly possible to reduce subsequent injuries[11].
Attention should be paid to pilots’ ejection and parachute training in order to significantly reduce ejection injury and improve the ejection success rate. In addition, air defense support personnel should strengthen search and rescue and on-site emergency measures, and locate and rescue pilots in distress quickly to reduce subsequent injuries.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Critical care medicine
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Gupta A, India; Shojiguchi N, Japan S-Editor: Yan JP L-Editor: Filipodia P-Editor: Yan JP
| 1. | Pavlović M, Pejović J, Mladenović J, Cekanac R, Jovanović D, Karkalić R, Randjelović D, Djurdjević S. Ejection experience in Serbian Air Force, 1990-2010. Vojnosanit Pregl. 2014;71:531-533. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 2] [Cited by in F6Publishing: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 2. | McBratney CM, Rush S, Kharod CU. Pilot ejection, parachute, and helicopter crash injuries. J Spec Oper Med. 2014;14:92-94. [PubMed] [Cited in This Article: ] |
| 3. | Manen O, Clément J, Bisconte S, Perrier E. Spine injuries related to high-performance aircraft ejections: a 9-year retrospective study. Aviat Space Environ Med. 2014;85:66-70. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 11] [Cited by in F6Publishing: 12] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 4. | Dikshit MB. To Err is Human Case Reports of Two Military Aircraft Accidents: Possible mechanisms of human failure. Sultan Qaboos Univ Med J. 2010;10:120-125. [PubMed] [Cited in This Article: ] |
| 5. | Miles JE. Factors Associated with Delayed Ejection in Mishaps Between 1993 and 2013. Aerosp Med Hum Perform. 2015;86:774-781. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 2] [Cited by in F6Publishing: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 6. | AlAbdulwahab SS, Kachanathu SJ, AlSunaidi ASN. A cross-sectional study on fear-avoidance beliefs and chronic low back pain in fighter pilots. Int J Crit Illn Inj Sci. 2021;11:29-32. [PubMed] [DOI] [Cited in This Article: ] [Cited by in F6Publishing: 1] [Reference Citation Analysis (0)] |
| 7. | Du C, Mo Z, Tian S, Wang L, Fan J, Liu S, Fan Y. Biomechanical investigation of thoracolumbar spine in different postures during ejection using a combined finite element and multi-body approach. Int J Numer Method Biomed Eng. 2014;30:1121-1131. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 40] [Cited by in F6Publishing: 34] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 8. | Nakamura A. Ejection experience 1956-2004 in Japan: an epidemiological study. Aviat Space Environ Med. 2007;78:54-58. [PubMed] [Cited in This Article: ] |
| 9. | Stemper BD, Storvik SG, Yoganandan N, Baisden JL, Fijalkowski RJ, Pintar FA, Shender BS, Paskoff GR. A new PMHS model for lumbar spine injuries during vertical acceleration. J Biomech Eng. 2011;133:081002. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 29] [Cited by in F6Publishing: 29] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 10. | Stemper BD, Yoganandan N, Pintar FA, Shender BS, Paskoff GR. Physical effects of ejection on the head-neck complex: demonstration of a cadaver model. Aviat Space Environ Med. 2009;80:489-494. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 7] [Cited by in F6Publishing: 8] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 11. | Epstein D, Markovitz E, Nakdimon I, Guinzburg A, Aviram E, Gordon B, Shapira S, Sharon S, Steinfeld Y, Miller A, Lipsky AM. Injuries associated with the use of ejection seats: a systematic review, meta-analysis and the experience of the Israeli Air Force, 1990-2019. Injury. 2020;51:1489-1496. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 4] [Cited by in F6Publishing: 4] [Article Influence: 1.0] [Reference Citation Analysis (0)] |