Published online Jun 16, 2022. doi: 10.12998/wjcc.v10.i17.5717
Peer-review started: October 21, 2021
First decision: March 7, 2022
Revised: March 16, 2022
Accepted: April 15, 2022
Article in press: April 15, 2022
Published online: June 16, 2022
Spontaneous isolated superior mesenteric artery dissection (SISMAD) is a rare disease that originates from the superior mesenteric artery, without the presence of aortic and other arterial dissections. Most cases are diagnosed using contrast-enhanced computed tomography (CECT), whereas the application of ultrasound is less common.
Here, we report a case of SISMAD with sudden epigastric pain that worsened as the main symptom after eating. The patient had a long history of hypertension with unknown blood pressure control but no history of smoking or alcohol consumption. This case was initially diagnosed using ultrasound and the results were later confirmed by CECT. After admission, the patient fasted, followed by parenteral nutrition support and fluid supplementation to maintain electrolyte and acid–base balance. Metoprolol succinate sustained-release tablets and aspirin were given as nonoperative treatments. After 1 wk, the symptoms improved, and the patient was discharged. During telephone follow-up, the patient did not develop similar symptoms.
Whether ultrasound can be used as a routine and noninvasive imaging method for the diagnosis of SISMAD needs further exploration.
Core tip: Spontaneous isolated superior mesenteric artery dissection is a rare disease. Contrast-enhanced computed tomography (CECT) is often the preferred diagnostic method for this disease. The initial diagnosis of this disease by ultrasound is rarely reported. Compared to CECT, ultrasound is a convenient, rapid, noninvasive, inexpensive and feasible bedside imaging method, which can be used to diagnose superior mesenteric artery dissection.
- Citation: Zhang Y, Zhou JY, Liu J, Bai C. Diagnosis of spontaneous isolated superior mesenteric artery dissection with ultrasound: A case report. World J Clin Cases 2022; 10(17): 5717-5722
- URL: https://www.wjgnet.com/2307-8960/full/v10/i17/5717.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i17.5717
Spontaneous isolated superior mesenteric artery dissection (SISMAD), first reported in 1947, is a dissection disease arising from the superior mesenteric artery, without aortic and other arterial dissections[1].
Clinical manifestations of SISMAD are atypical. The most common symptoms include sudden persistent or paroxysmal severe abdominal pain, accompanied by other gastrointestinal symptoms. Also, some of the patients are asymptomatic. In addition, clinical and physical examinations reveal no specificity, and no laboratory indicators for SISMAD are currently available[2,3]. SISMAD may directly lead to intestinal ischemic necrosis and arterial rupture, which endangers the life of patients if not treated in a timely manner[4,5]. At present, the diagnosis of SISMAD is mainly dependent on imaging examinations, and contrast-enhanced computed tomography (CECT) and computed tomography angiography (CTA) are most commonly used[6,7]. Ultrasound is rarely used to diagnose SIDSMA. Here, we reported an ultrasound-confirmed SISMAD case without dissecting aneurysm or thrombosis, suggesting that ultrasound could be used in the diagnosis of SISMAD.
A 64-year-old Chinese Han female patient was admitted to the First Affiliated Hospital of Chengdu Medical College on April 27, 2020, due to intermittent pain in the upper abdomen.
Epigastric pain became worse after eating for 3 d.
She had a history of hypertension for > 10 years and was on antihypertensive medication, but her blood pressure control was unknown. The patient received a cardiac pacemaker implant 2 years ago, and was given dabigatran ester (capsules 110 mg bid) as long-term anticoagulant therapy after surgery. She underwent cholecystectomy in the First Affiliated Hospital of Chengdu Medical College due to calculous cholecystitis on March 21, 2019.
The patient did not have any history of smoking or alcohol consumption.
The blood pressure was 170/110 mmHg at admission.
No other obvious abnormalities were detected based on physical examination and laboratory tests.
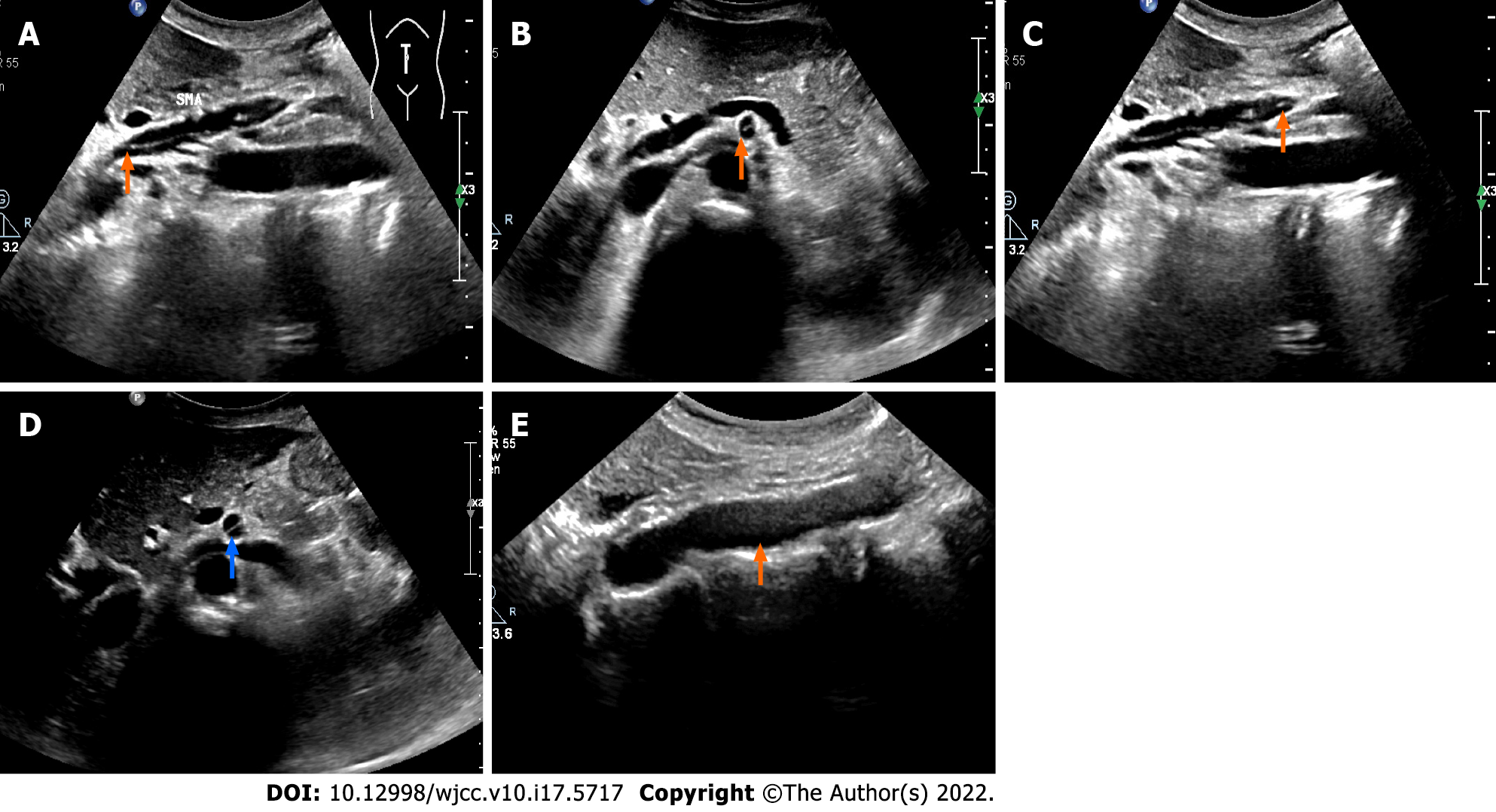
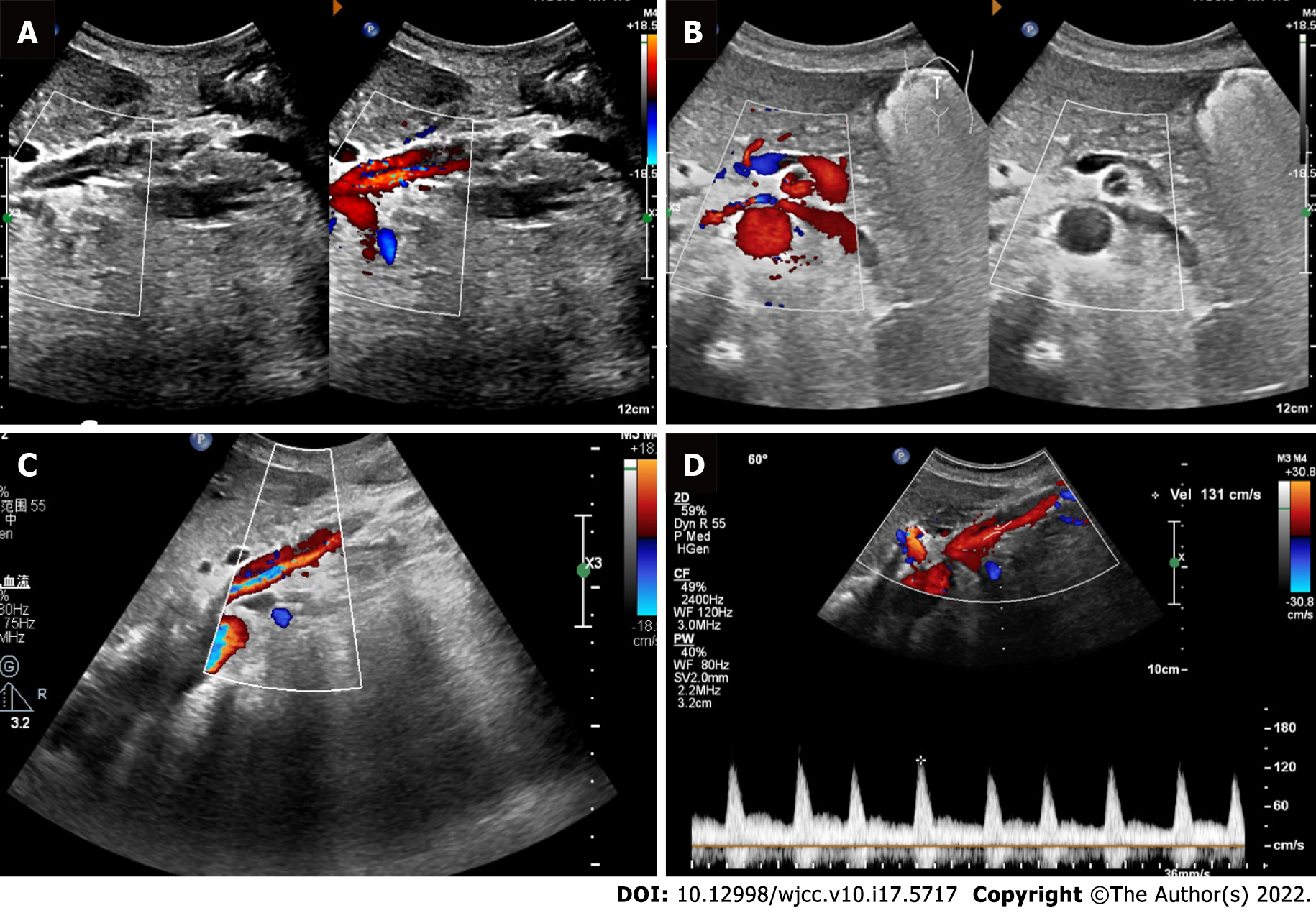
Abdominal ultrasound was routinely performed since the patient had superior abdominal pain. However, no obvious abnormalities in the liver, pancreas and spleen were observed. Strip echoes were found in the lumen about 1.6 cm from the opening of the superior mesenteric artery distal to the main trunk of the superior mesenteric artery with stripped intima. The arterial lumen was divided into true and false lumen by the exfoliated intima. Ventral false lumen had a large diameter, while that of the dorsal true lumen was small. Lumen sonopenetrability was normal, and no thrombosis was detected. Proximal to the exfoliated intima, a 3-mm wide rupture was observed (Figure 1). Color Doppler imaging showed blood flow passing through the incision. The blood flow in the ventral lumen was dark, while colored blood flow signals were observed in the dorsal lumen. Pulse Doppler was used to assess blood flow velocity in the true lumen (Figure 2).
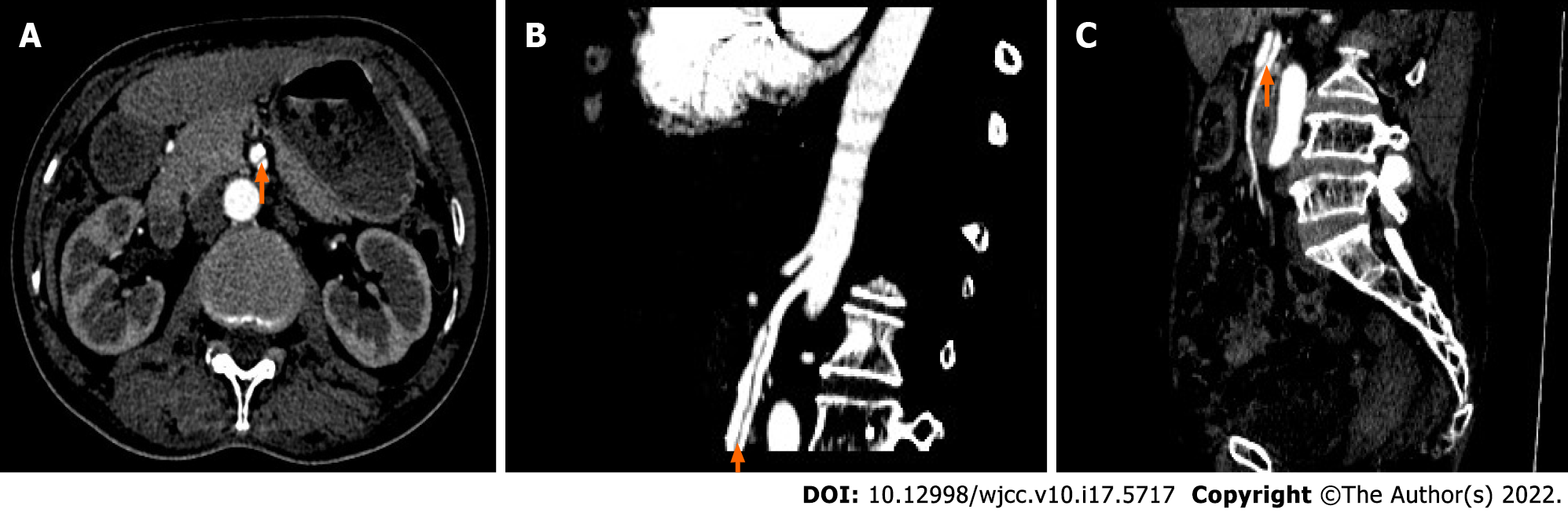
Ultrasonography of the abdominal aorta showed no shed intimal echo (Figure 1), suggesting isolated superior mesenteric artery dissection, which was later confirmed by CECT (Figure 3).
After admission, the patient fasted, followed by parenteral nutrition support and fluid supplementation to maintain electrolyte and acid–base balance. Metoprolol succinate sustained-release tablets (47.5 mg/d) were given to lower blood pressure, and aspirin (100 mg/d) was given as an antiplatelet treatment.
After 1 wk, the symptoms improved, and the patient was discharged. During telephone follow-up at 1, 3 and 6 mo after discharge, the patient did not experience similar symptoms and did not visit any local medical facility for imaging re-examination.
Currently, the most commonly used imaging methods for the diagnosis of SISMAD are CTA and CECT[8], and only a few diagnosed cases have been confirmed by ultrasound[9-12]. In this case report, ordinary grayscale ultrasound could detect the start and end points of the intimal exfoliation in the superior mesenteric artery, the location and number of ruptures, and whether there was thrombus in the lumen. Color Doppler ultrasonography was used to investigate the blood flow through the rupture sites, the blood flow velocity in the true and false lumen, and the filling defect areas caused by thrombus in real time. Yun et al[13] classified SISMAD into types I, II (IIa and IIb) and III. In this case, a rupture was detected about 1.6 cm from the opening of the superior mesenteric artery, while its distal end was closed. No thrombosis was detected in either the true or false lumen, and the ultrasound finding was in line with a type IIa SISMAD.
Isolated superior mesenteric artery dissection is a rare disease with unknown etiology. It has been reported that male sex, smoking, atherosclerosis, hypertension, hyperlipidemia, cystic necrosis of the middle artery, and Asian ethnicity might be related to the pathogenesis of SISMAD[14-16]. Among these, hypertension plays a crucial role in the development of arterial dissection. In our case, the patient had a history of hypertension for > 10 years. Furthermore, SISMAD was a rare acute abdomen with no specific clinical manifestations. The primary symptoms were sudden and severe abdominal pains, mainly epigastric pain[17,18]. Our patient had intermittent pain in the upper abdomen without any specific positive signs. Currently, conservative treatment, endovascular surgery, interventional radiology, and open surgery are therapeutic modalities for patients with SISMAD, but there are no clear recommendations for the treatment of SISMAD[15,16,19,20]. According to current guidelines, SISMAD treatment strategies are designed to control clinical symptoms and prevent complications such as intestinal necrosis. Most studies recommend initial treatment based on clinical presentation at admission. If SISMAD is found accidentally during CTA in other settings, the patient can be carefully observed and treated conservatively[6,21]. Asymptomatic patients receiving conservative treatments do not need secondary interventions[22]. In symptomatic SISMAD patients, EVT may be performed before mesenteric ischemia progresses if clinical symptoms persist. The reconstruction of SMA was significantly improved after EVT, especially for patients with Yun's IIb phenotype[23].
Although CTA or CECT could clearly display and classify the type of superior mesenteric artery dissection, especially small distal branch vessels, there was an issue of contrast agent allergy as patients received a large radiation dose[24]. Ultrasound was simple and easy to perform, radiation free, and repeatable, and could clearly observe the echoes of exfoliated intima, the positions of the rupture and the thrombosis, and hemodynamic changes could be displayed using Doppler ultrasound. Also, bedside examination could be performed when necessary[12,25]. It has also been suggested that early transition to ultrasound imaging exam should be considered in the follow-up of SISMAD patients, which may help to reduce radiation, contrast, and associated costs[17].
This case report suggests that ultrasound is a noninvasive examination method for routine screening of SISMAD, which could provide a clinical management basis for the diagnosis and treatment of the disease.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Radiology, nuclear medicine and medical imaging
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Ghannam WM, Egypt S-Editor: Liu JH L-Editor: Kerr C P-Editor: Liu JH
| 1. | Bauersfeld SR. Dissecting aneurysm of the aorta; a presentation of 15 cases and a review of the recent literature. Ann Intern Med. 1947;26:873-889. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 141] [Cited by in F6Publishing: 152] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 2. | Xu L, Shao J, Zhang D, Qiu C, Wang J, Li K, Fang L, Zhang X, Lei J, Lai Z, Ma J, Yu Y, Yu X, Du F, Qi W, Chen J, Liu B. Long-term outcomes of conservative treatment and endovascular treatment in patients with symptomatic spontaneous isolated superior mesenteric artery dissection: a single-center experience. BMC Cardiovasc Disord. 2020;20:256. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 3] [Cited by in F6Publishing: 11] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 3. | Tanaka Y, Yoshimuta T, Kimura K, Iino K, Tamura Y, Sakata K, Hayashi K, Takemura H, Yamagishi M, Kawashiri MA. Clinical characteristics of spontaneous isolated visceral artery dissection. J Vasc Surg. 2018;67:1127-1133. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 17] [Cited by in F6Publishing: 20] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 4. | Kim H, Park H, Park SJ, Park BW, Hwang JC, Seo YW, Cho HR. Outcomes of Spontaneous Isolated Superior Mesenteric Artery Dissection Without Antithrombotic Use. Eur J Vasc Endovasc Surg. 2018;55:132-137. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 22] [Cited by in F6Publishing: 22] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 5. | Karaolanis G, Antonopoulos C, Tsilimigras DI, Moris D, Moulakakis K. Spontaneous isolated superior mesenteric artery dissection: Systematic review and meta-analysis. Vascular. 2019;27:324-337. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 14] [Cited by in F6Publishing: 16] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 6. | Kimura Y, Kato T, Nagao K, Izumi T, Haruna T, Ueyama K, Inada T, Inoko M. Outcomes and Radiographic Findings of Isolated Spontaneous Superior Mesenteric Artery Dissection. Eur J Vasc Endovasc Surg. 2017;53:276-281. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 28] [Cited by in F6Publishing: 29] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 7. | Tomita K, Obara H, Sekimoto Y, Matsubara K, Watada S, Fujimura N, Shibutani S, Nagasaki K, Hayashi S, Harada H, Asami A, Uchida N, Kakefuda T, Kitagawa Y. Evolution of Computed Tomographic Characteristics of Spontaneous Isolated Superior Mesenteric Artery Dissection During Conservative Management. Circ J. 2016;80:1452-1459. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 49] [Cited by in F6Publishing: 52] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 8. | Nath A, Yewale S, Kousha M. Spontaneous Isolated Superior Mesenteric Artery Dissection. Case Rep Gastroenterol. 2016;10:775-780. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 7] [Cited by in F6Publishing: 10] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 9. | Ishimura M, Hayashi R, Shimotsuka H, Ogawa K, Iuchi K. A case of isolated superior mesenteric artery dissection evaluated clinical course by ultrasonography. ChoonpaIgaku. 2008;35:191-195. [DOI] [Cited in This Article: ] |
| 10. | Davis CB, Kendall JL. Emergency bedside ultrasound diagnosis of superior mesenteric artery dissection complicating acute aortic dissection. J Emerg Med. 2013;45:894-896. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 5] [Cited by in F6Publishing: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 11. | Huang CY, Sun JT, Lien WC. Early Detection of Superior Mesenteric Artery Dissection by Ultrasound: Two Case Reports. J Med Ultrasound. 2019;27:47-49. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 4] [Cited by in F6Publishing: 4] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 12. | Bao S, Wang T, Jin X, Zhang S, Qi H, Dong D, Mou X, Zhang X, Li C. Diagnostic value of color Doppler sonography for spontaneous isolated superior mesenteric artery dissection. Exp Ther Med. 2019;17:3489-3494. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 3] [Cited by in F6Publishing: 4] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 13. | Yun WS, Kim YW, Park KB, Cho SK, Do YS, Lee KB, Kim DI, Kim DK. Clinical and angiographic follow-up of spontaneous isolated superior mesenteric artery dissection. Eur J Vasc Endovasc Surg. 2009;37:572-577. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 138] [Cited by in F6Publishing: 154] [Article Influence: 10.3] [Reference Citation Analysis (0)] |
| 14. | Shiraki H, Kasamoto M, Yasutomi M, Kaji S, Akutsu K, Furukawa Y, Shimizu W, Inoue N. Clinical Features of Spontaneous Isolated Dissection of Abdominal Visceral Arteries. J Clin Med Res. 2020;12:13-17. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 4] [Cited by in F6Publishing: 6] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 15. | Luan JY, Guan X, Li X, Wang CM, Li TR, Zhang L, Han JT. Isolated superior mesenteric artery dissection in China. J Vasc Surg. 2016;63:530-536. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 52] [Cited by in F6Publishing: 48] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 16. | Kim YW. Current Understandings of Spontaneous Isolated Superior Mesenteric Artery Dissection. Vasc Specialist Int. 2016;32:37-43. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 30] [Cited by in F6Publishing: 34] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 17. | Zettervall SL, Karthaus EG, Soden PA, Buck DB, Ultee KH, Schermerhorn ML, Wyers MC. Clinical presentation, management, follow-up, and outcomes of isolated celiac and superior mesenteric artery dissections. J Vasc Surg. 2017;65:91-98. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 22] [Cited by in F6Publishing: 20] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 18. | DeCarlo C, Ganguli S, Borges JC, Schainfeld RM, Mintz AJ, Mintz J, Jaff MR, Weinberg I. Presentation, treatment, and outcomes in patients with spontaneous isolated celiac and superior mesenteric artery dissection. Vasc Med. 2017;22:505-511. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 15] [Cited by in F6Publishing: 16] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 19. | Takahashi B, Nakayama Y, Shiroma S, Ido K. Three Case Report of Spontaneous Isolated Dissection of the Superior Mesenteric Artery-With an Algorithm Proposed for the Management. Ann Vasc Dis. 2015;8:120-123. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 13] [Cited by in F6Publishing: 13] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 20. | Acosta S, Gonçalves FB. Management of Spontaneous Isolated Mesenteric Artery Dissection: A Systematic Review. Scand J Surg. 2021;110:130-138. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 7] [Cited by in F6Publishing: 19] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 21. | Qiu C, He Y, Li D, Shang T, Wang X, Wu Z, Zhang H. Mid-Term Results of Endovascular Treatment for Spontaneous Isolated Dissection of the Superior Mesenteric Artery. Eur J Vasc Endovasc Surg. 2019;58:88-95. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 21] [Cited by in F6Publishing: 21] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 22. | Wang J, He Y, Zhao J, Yuan D, Xu H, Ma Y, Huang B, Yang Y, Bian H, Wang Z. Systematic review and meta-analysis of current evidence in spontaneous isolated celiac and superior mesenteric artery dissection. J Vasc Surg. 2018;68:1228-1240.e9. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 53] [Cited by in F6Publishing: 50] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 23. | Yu SH, Hii IH, Wu IH. Comparison of Superior Mesenteric Artery Remodeling and Clinical Outcomes between Conservative or Endovascular Treatment in Spontaneous Isolated Superior Mesenteric Artery Dissection. J Clin Med. 2022;11. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 3] [Cited by in F6Publishing: 3] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 24. | Mandlik V, Prantl L, Schreyer AG. Contrast Media Extravasation in CT and MRI - A Literature Review and Strategies for Therapy. Rofo. 2019;191:25-32. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 6] [Cited by in F6Publishing: 3] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 25. | Czihal M, Lottspeich C, Hoffmann U. Ultrasound imaging in the diagnosis of large vessel vasculitis. Vasa. 2017;46:241-253. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 17] [Cited by in F6Publishing: 21] [Article Influence: 3.0] [Reference Citation Analysis (0)] |