Published online Jun 26, 2022. doi: 10.12998/wjcc.v10.i18.6105
Peer-review started: April 14, 2021
First decision: September 28, 2021
Revised: November 5, 2021
Accepted: May 5, 2022
Article in press: May 5, 2022
Published online: June 26, 2022
Currently, the mainstay of chronic eosinophilic pneumonia (CEP) treatment is corticosteroids, usually with a favorable response and good prognosis. However, relapse is common, requiring long-term use of corticosteroids, with risk of significant treatment-related complications. The dire need to develop new treatments for patients with CEP, who are dependent on, or resistant to corticosteroids has led to exploring novel therapies. We herein describe a patient with acute relapse of CEP, who was successfully treated with benralizumab, an IL-5Rα antagonist that has demonstrated rapid anti-eosinophil action in patients with asthma. Currently, only three recent patient reports on CEP relapse, also demonstrated successful treatment with benralizumab alone, without corticosteroids.
A 31-year-old non-smoking woman presented in our hospital with a 3 wk history of shortness of breath, dry cough and fever up to 38.3 °C. Laboratory examination revealed leukocytosis 10240 K/µL, eosinophilia 900 K/µL and normal values of hemoglobin, platelets, creatinine and liver enzymes. Computed tomography of the chest showed a mediastinal lymphadenopathy and consolidations in the right upper and left lower lobes. CEP was diagnosed, and the patient was treated with hydrocortisone intravenously, followed by oral prednisone, with prompt improvement. Three months later, she presented with relapse of CEP: aggravation of dyspnea, rising of eosinophilia and extension of pulmonary infiltrates on chest X-ray. She was treated with benralizumab only, with clinical improvement within 2 wk, and complete resolution of lung infiltrates following 5 wk.
Due to Benralizumab’s dual mechanism of action, it both neutralizes IL-5Rα pro-eosinophil functions and triggers apoptosis of eosinophils. We therefore maintain benralizumab can serve as a reasonable therapy choice for every patient with chronic eosinophilic pneumonia and a good alternative for corticosteroids.
Core Tip: Chronic eosinophilic pneumonia (CEP) is an idiopathic pulmonary disease, characterized by marked eosinophil accumulation in the pulmonary parenchyma. Currently, the mainstay of CEP treatment is corticosteroids. However, relapse is common, requiring long-term use of corticosteroids, with the risk of significant treatment-related adverse effects. Herein, we describe a patient with an acute CEP relapse, successfully treated with benralizumab alone, without corticosteroids. Currently, only three patients with acute relapse of CEP, were reported successfully treated with benralizumab alone, without corticosteroids. This therapy option may be particularly beneficial for patients who have previously suffered serious adverse effects from or have any contraindications to chronic corticosteroid treatment.
- Citation: Izhakian S, Pertzov B, Rosengarten D, Kramer MR. Successful treatment of acute relapse of chronic eosinophilic pneumonia with benralizumab and without corticosteroids: A case report . World J Clin Cases 2022; 10(18): 6105-6109
- URL: https://www.wjgnet.com/2307-8960/full/v10/i18/6105.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i18.6105
Chronic eosinophilic pneumonia (CEP) is an inflammatory lung disease, clinically characterized by isolated pulmonary involvement, with appearance of pulmonary eosinophilic infiltrates[1] that permeate the lungs, presenting symptoms include cough, fever and dyspnea[2]. Response to oral corticosteroids (OCS), the commonly administered treatment for CEP, is usually dramatic and rapid[3]. However, in approximately 50% of the patients, CEP relapses under tapering of OCS, and thus long-term OCS administration is required[3]. Unfortunately, chronic OCS treatment has a proven increased risk for treatment-related adverse effects and complications, (e.g., hypertension, diabetes mellitus, osteoporosis and infections)[4]. Therefore, the dire need to develop new treatments for patients with CEP, who are dependent on, or resistant to OCS has led to exploring novel therapies. Benralizumab, an IL-5Rα antagonist has demonstrated rapid anti-eosinophil action in patients with asthma. Successful treatment with benralizumab, was also recently reported in three patients with acute relapse of CEP[5-7]. We herein describe an additional patient with an acute relapse of CEP who was successfully treated with benralizumab alone, without corticosteroids.
On July 26, 2020, a 31-year-old non-smoking healthy woman was evaluated in our hospital. She presented with a 3-wk history of shortness of breath, dry cough and fever up to 38.3 °C.
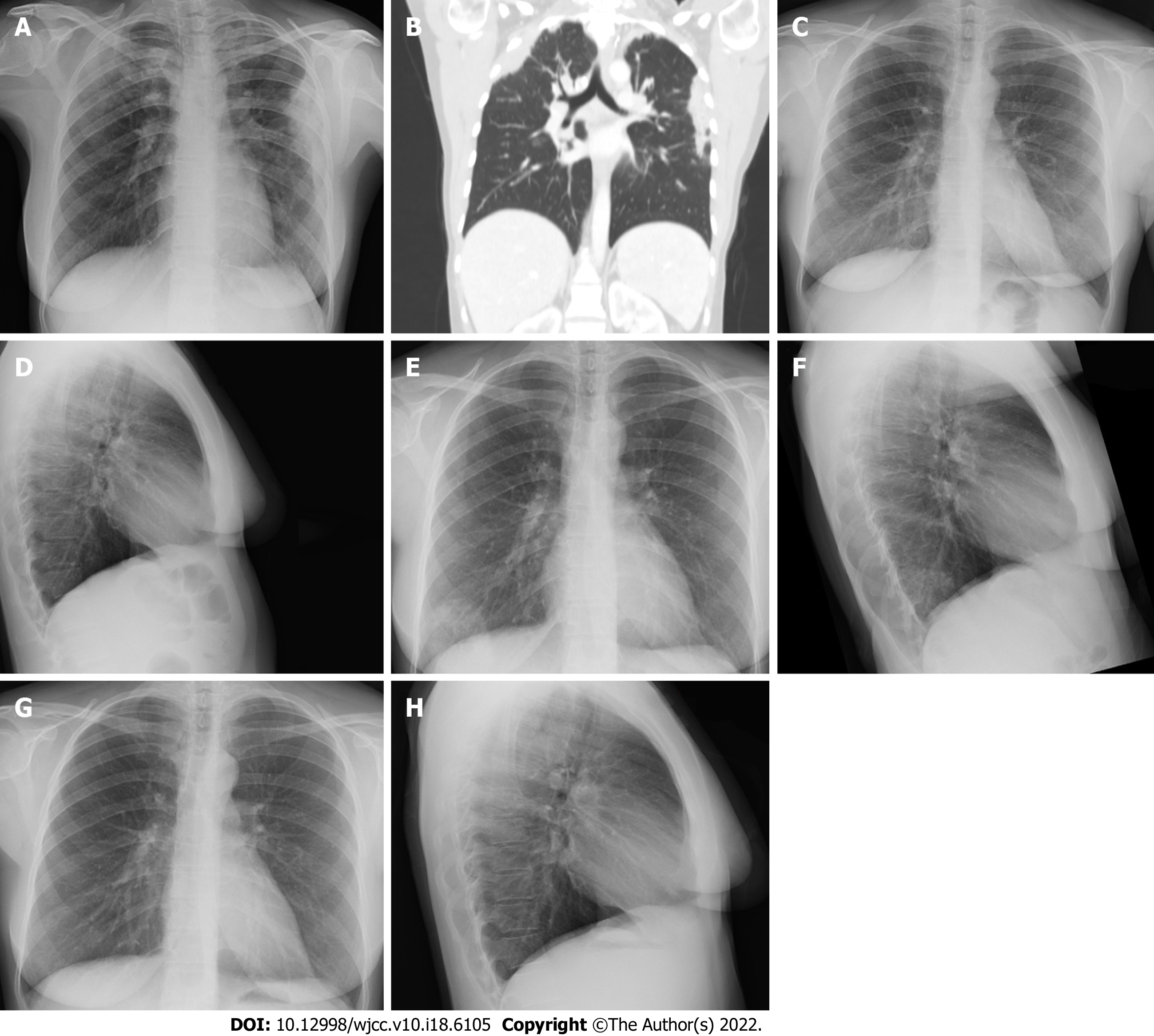
Two weeks prior to the presentation at our medical center, the patient was examined at a local emergency department for the same complaints, which had then appeared for one week. At that time, a chest X-ray showed infiltrates in the right upper and left lateral lung fields (Figure 1A). The laboratory examination revealed mild leukocytosis 11200 K/µL, eosinophilia 800 K/µL and an elevated level of serum C-reactive protein 45 mg/L. Nasopharyngeal swabs were negative for coronavirus disease 2019 (COVID-19). She was discharged home from the local hospital with recommendations for oral treatment with cefuroxime 500 mg and roxithromycin 150 mg, both twice daily for 7 days.
No specific history of past illness was reported.
The patient's temperature was 37.3 °C, heart rate 97 beats per minute, respiratory rate 16 breaths per minute, blood pressure 103/71 mmHg and oxygen saturation in room air 97%. On the chest examination, crepitation was detected on the left lung base. The rest of the physical examination was unrevealing.
Abnormal laboratory findings included leukocytosis 10240 K/µL and eosinophilia 900 K/µL. Results of other routine blood tests were normal. A screening panel was negative for allergic bronchopulmonary aspergillosis, including Aspergillus specific immunoglobulin E and Aspergillus fumigatus serum precipitant. No antinuclear and anti-neutrophil cytoplasmic antibodies were detected. Serologic tests for Toxocara, Strongyloides, Schistosoma and Echinococcus were negative.
Computed tomography (CT) of the chest (axial plain) showed a mediastinal lymphadenopathy, and pulmonary consolidations in the right upper and left lower lobes (Figure 1B).
Eosinophilic pneumonia was diagnosed based on clinical symptoms, peripheral blood eosinophilia, peripheral lung consolidation on chest CT and prompt response to systemic glucocorticoid therapy.
The patient was treated with hydrocortisone intravenously at a dosage of 100 mg three times per day, for 2 days, with rapid improvement of dyspnea and cough. The treatment was switched to oral prednisone, at a daily dosage of 40 mg, which was tapered down during the following 2 mo. On September 6, 2020, the patient was feeling well, eosinophilia had resolved, and pulmonary infiltrates no longer appeared on chest X-ray (Figures 1C and D).
On December 6, 2020, the patient was reevaluated, due to recurrence of dyspnea, cough and fever. Laboratory examination demonstrated blood eosinophilia 600 K/µL, white blood cells 8.8 k/micL and C-reactive protein 0.2 mg/dL. Chest X-ray revealed a new infiltrate in the right lower lobe of the frontal view (Figure 1E), which was clearer in the lateral view (Figure 1F). Acute relapse of CEP was diagnosed. We discussed with the patient treatment options, including the advantages and disadvantages of therapy with OCS vs anti-interleukin-5 drug, benralizumab. It was decided to start (on December 7, 2020) benralizumab subcutaneously, at a dosage of 30 mg monthly, without OCS. Following 2 wk, the patient reported significant improvement of the symptoms. One month after the first injection of benralizumab, eosinophils were zero and WBC 4 k/micL; CRP was not taken. Five weeks after the first injection, a chest X-ray was unrevealing (Figure 1G and H). Two months later, the patient received the second and third injections of benralizumab and demonstrated sustained clinical and radiographic remission of CEP.
To the best of our knowledge, we present the fourth recent report in the medical literature regarding rapid improvement of acute flare of CEP, following treatment with benralizumab, without OCS. In previous cases, benralizumab therapy was initiated after frequent, acute CEP relapses, or as an alternative after patient refusal to reinitiate OSC, due to treatment-related adverse effects. Isomoto et al[5] described a 58-year-old woman with CEP and a history of refractory asthma. She had three flares of her concomitant disease in the preceding year, which necessitated OCS therapy. Only for the fourth flare, her treating physician initiated a different therapy, one injection of benralizumab, which induced remission of her asthma and CEP following 16 wk. Izumo et al[6] described a 43-year-old healthy woman who presented with chronic cough. She was diagnosed with CEP and successfully treated with prednisolone. However, her symptoms worsened after prednisolone cessation. Following patient refusal to re-initiation of OCS, due to treatment-related adverse effects, benralizumab treatment was initiated. After 6 mo of benralizumab therapy, sustained remission of CEP was achieved. Yazawa et al[7] described a 70-year-old woman with a history of bronchial asthma who had dyspnea and cough for one month, and was diagnosed with CEP. She refused OCS and therefore was treated with benralizumab, which resulted in resolution of symptoms, hypoxemia and lung infiltrates. Moreover, 12 mo benralizumab maintenance treatment without OCS, provided sustained remission of CEP.
CEP is an idiopathic lung disease that is characterized by isolated pulmonary involvement, with marked eosinophil accumulation in the pulmonary parenchyma[1,2]. Therefore, we maintain benralizumab is a reasonable therapy choice for every patient with CEP. Predominately, due to its dual mechanism of action, benralizumab a humanized monoclonal antibody, as an interleukin-5 receptor α (IL-5Rα) antagonist, neutralizes the pro-eosinophil functions of IL-5R, by binding to its α subunit and by binding to FcγRIIIa receptor expressed by natural killer cells, triggers apoptosis of eosinophils via antibody-dependent cell-mediated cytotoxicity[8]. This therapy is especially important in patients with CEP, who present with specific clinical scenarios. As demonstrated, treatment with benralizumab may be beneficial for patients with frequent CEP relapses. Clearly, benralizumab could be the drug of choice in patients who demonstrate serious adverse effects following OCS therapy. Likewise, benralizumab therapy seems to be preferred in patients with comorbidities that are expected to be aggravated under OCS treatment.
For treatment of CEP, we maintain benralizumab can serve as a reasonable therapy choice for every patient and a good alternative for OCS.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Respiratory system
Country/Territory of origin: Israel
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C, C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Hu QD, China; Liu H, China; Pan H, China S-Editor: Wang JL (Online Science Editor) L-Editor: Wang TQ P-Editor: Ma YJ
| 1. | Suzuki Y, Suda T. Eosinophilic pneumonia: A review of the previous literature, causes, diagnosis, and management. Allergol Int. 2019;68:413-419. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 41] [Cited by in F6Publishing: 59] [Article Influence: 11.8] [Reference Citation Analysis (0)] |
| 2. | Marchand E, Reynaud-Gaubert M, Lauque D, Durieu J, Tonnel AB, Cordier JF. Idiopathic chronic eosinophilic pneumonia. A clinical and follow-up study of 62 cases. The Groupe d'Etudes et de Recherche sur les Maladies "Orphelines" Pulmonaires (GERM"O"P). Medicine (Baltimore). 1998;77:299-312. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 166] [Cited by in F6Publishing: 130] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 3. | Durieu J, Wallaert B, Tonnel AB. Long-term follow-up of pulmonary function in chronic eosinophilic pneumonia. Groupe d'Etude en Pathologie Interstitielle de la Société de Pathologie Thoracique du Nord. Eur Respir J. 1997;10:286-291. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 52] [Cited by in F6Publishing: 55] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 4. | Naughton M, Fahy J, FitzGerald MX. Chronic eosinophilic pneumonia. A long-term follow-up of 12 patients. Chest. 1993;103:162-165. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 91] [Cited by in F6Publishing: 99] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 5. | Isomoto K, Baba T, Sekine A, Aiko N, Ogura T. Promising Effects of Benralizumab on Chronic Eosinophilic Pneumonia. Intern Med. 2020;59:1195-1198. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 10] [Cited by in F6Publishing: 8] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 6. | Izumo T, Kuse N, Awano N, Tone M, Jo T, Yoshimura H, Minami J, Takada K, Muto Y, Fujimoto K, Inomata M. Rapid and sustained effects of a single dose of benralizumab on chronic eosinophilic pneumonia. Respir Med Case Rep. 2020;30:101062. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 2] [Cited by in F6Publishing: 5] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 7. | Yazawa S, Toyoshima M, Koda K, Suda T. Benralizumab as initial treatment for chronic eosinophilic pneumonia. Allergol Int. 2021;70:140-142. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 5] [Cited by in F6Publishing: 12] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 8. | Kolbeck R, Kozhich A, Koike M, Peng L, Andersson CK, Damschroder MM, Reed JL, Woods R, Dall'acqua WW, Stephens GL, Erjefalt JS, Bjermer L, Humbles AA, Gossage D, Wu H, Kiener PA, Spitalny GL, Mackay CR, Molfino NA, Coyle AJ. MEDI-563, a humanized anti-IL-5 receptor alpha mAb with enhanced antibody-dependent cell-mediated cytotoxicity function. J Allergy Clin Immunol. 2010;125:1344-1353.e2. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 378] [Cited by in F6Publishing: 409] [Article Influence: 29.2] [Reference Citation Analysis (0)] |