Hong Kong Med J 2023 Dec;29(6):548–50 | Epub 2 Nov 2023
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
CASE REPORT
Tuberculosis of the knee as a great mimicker of
inflammatory arthritis: a case report
Holy MH Chan, MB, BS1; Henry Fu, MB, BS, FRCSEd (Orth)2; KY Chiu, MB, BS, FRCSEd (Orth)2
1 Li Ka Shing Faculty of Medicine, The University of Hong Kong, Hong Kong SAR, China
2 Department of Orthopaedics and Traumatology, School of Clinical Medicine, The University of Hong Kong, Hong Kong SAR, China
Corresponding author: Dr Henry Fu (drhfu@ortho.hku.hk)
Case presentation
In January 2015, a 36-year-old man with good past
health presented to a hospital in Hong Kong with
intermittent low-grade fever and left knee effusion.
Physical examination revealed mild effusion,
erythema, warmth and tenderness over the left knee,
with 10˚ flexion contracture and flexion range up
to only 70˚. The levels of inflammatory markers (C-reactive
protein [CRP], erythrocyte sedimentation
rate [ESR], and antinuclear antibodies [ANA])
were elevated. Single-attempt arthrocentesis on
the affected knee yielded 1 mL of yellow fluid,
subsequently negative for Gram stain and culture
only. No obvious abnormalities were observed on
plain radiograph (Fig 1a), but magnetic resonance
imaging (MRI) in June 2015 demonstrated synovial
thickening, bone marrow oedema and subtle
cortical erosion at the lateral femoral condyle
(Fig 1b). Infection could not be excluded. Non-steroidal
anti-inflammatory drugs were prescribed
for symptomatic control. The recurrent left knee
effusion persisted despite treatment, but no further
attempts at arthrocentesis were made until 2018.
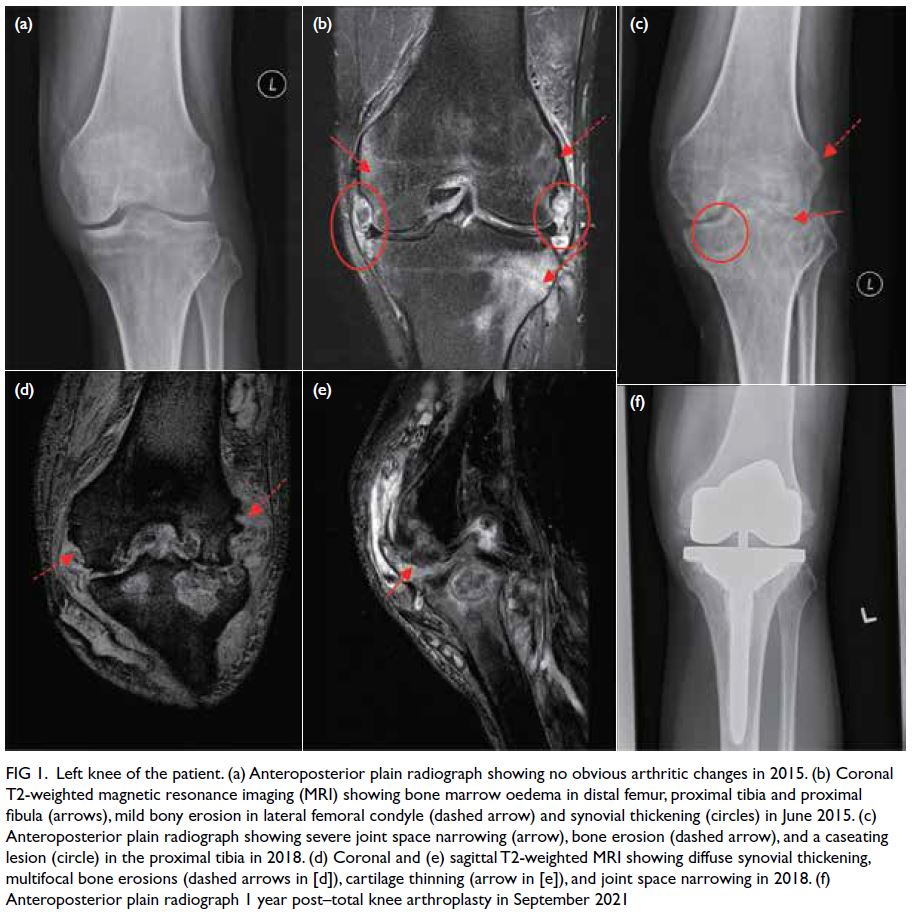
Figure 1. Left knee of the patient. (a) Anteroposterior plain radiograph showing no obvious arthritic changes in 2015. (b) Coronal T2-weighted magnetic resonance imaging (MRI) showing bone marrow oedema in distal femur, proximal tibia and proximal fibula (arrows), mild bony erosion in lateral femoral condyle (dashed arrow) and synovial thickening (circles) in June 2015. (c) Anteroposterior plain radiograph showing severe joint space narrowing (arrow), bone erosion (dashed arrow), and a caseating lesion (circle) in the proximal tibia in 2018. (d) Coronal and (e) sagittal T2-weighted MRI showing diffuse synovial thickening, multifocal bone erosions (dashed arrows in [d]), cartilage thinning (arrow in [e]), and joint space narrowing in 2018. (f) Anteroposterior plain radiograph 1 year post–total knee arthroplasty in September 2021
In view of the joint stiffness, recurrent
knee effusion and persistently elevated levels of
inflammatory markers, the patient was referred to
a rheumatologist. A working diagnosis of atypical
rheumatoid arthritis (RA) was made despite
negative testing of anticyclic citrullinated peptide
antibody and rheumatoid factor. Sulphasalazine
was started in September 2015. Due to persistent
knee inflammation, intraarticular steroid injection
was given in November 2015 with limited effect.
Methotrexate and leflunomide were prescribed in
escalating doses. The patient was simultaneously
followed up by the orthopaedic department where
analgesics and physiotherapy were prescribed.
Interval MRI in December 2017 showed diffuse
synovial thickening, multifocal erosive changes and
bone marrow oedema in the proximal tibia, reported
to be in keeping with RA. Due to progressive
worsening of his knee, the patient attended the
private sector and was prescribed golimumab
biologics in February 2018.
In April 2018, a cystic swelling developed over
the posterolateral aspect of his left knee. Results of
aspiration yielded a positive acid-fast bacilli smear
and rapid cultures via Mycobacteria Growth Indicator
Tube grew Mycobacterium tuberculosis. Knee X-ray
revealed complete erosion of the medial and lateral
tibiofemoral joints (Fig 1c) while MRI showed
synovial thickening and intraosseous collection over
the medial and lateral tibia (Fig 1d and e). Disease-modifying
antirheumatic drugs were discontinued
and the patient commenced a 9-month course of
antituberculous drugs, namely isoniazid, rifampicin,
ethambutol, pyrazinamide, and pyridoxine.
Despite eventually controlling the tuberculosis
(TB), the patient’s knee function deteriorated and he
was referred to a tertiary hospital for consideration
of total knee arthroplasty (TKA). Preoperative
assessment revealed 60˚ ankylosis of the left knee
(Fig 2a) and healed sinus tracts without signs of
residual infection. Preoperative investigations
revealed normal ESR and CRP levels. Robotic
arm–assisted TKA with varus-valgus constrained
insert (Fig 1f) was performed in March 2020 and
the patient was prescribed a 12-month course of
antituberculous chemotherapy postoperatively.
Postoperative range of motion (ROM) was 0˚ to 70˚
with 10˚ extension lag at 6 weeks due to quadriceps
atrophy. Manipulation under anaesthesia was
performed 3 months postoperatively to enhance
flexion range. A final ROM was of 0˚ to 95˚ was
achieved with no residual extension lag (Fig 2b and c). The latest follow-up 1.5 years postoperatively
showed stable ROM with no signs of reinfection. The
patient could walk unaided.
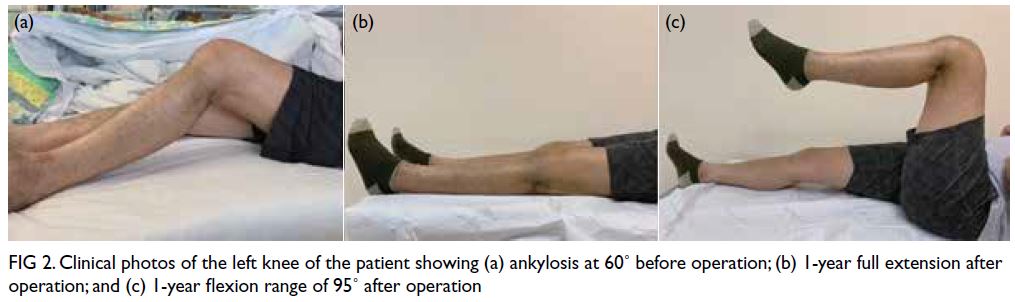
Figure 2. Clinical photos of the left knee of the patient showing (a) ankylosis at 60˚ before operation; (b) 1-year full extension after operation; and (c) 1-year flexion range of 95˚ after operation
Discussion
Tuberculosis of the knee is a rare form of
osteoarticular TB that is prone to misdiagnosis due
to its nonspecific presentation. It has an indolent
course compared with bacterial septic arthritis.
The clinical, radiological and laboratory features
mimic inflammatory arthritis such as RA. Both
diseases can present with monoarticular joint pain,
erythema, swelling, and stiffness. In knee TB, the Phemister triad of juxta-articular osteopenia, joint
space narrowing and peripheral bone erosions can
be observed on plain radiographs, but these can
also be evident in RA. Magnetic resonance imaging
features of TB include multifocal bone erosions,
articular surface destruction, cartilage erosions, and
marrow oedema.1 Similar laboratory results include
elevated white cell count (WCC) and percentage of
polymorphonuclear neutrophils (PMNs) in blood
and synovial fluid, and sustained elevation of ESR,
CRP and anti-nuclear antibody levels due to active
inflammation.
As in all circumstances of suspected infection,
a patient’s symptoms and risk factors such as
diabetes mellitus, RA and prior surgery should be
assessed.2 Local skin condition, effusion and ROM
should be noted on physical examination. Synovial fluid from arthrocentesis should be sent for total and
differential cell counts, biochemistry, microbiology,
crystals, and cytology. Total and differential
counts are helpful in differentiating infective and
inflammatory causes. Synovial fluid with WCC
of >50 000/mm3 and PMN level of >75% point
towards acute septic arthritis, while WCC of 2000 to
100 000/mm3 and PMN level of >50% suggest
inflammatory arthritis.3 Nonetheless in TB, the
WCC is typically in the inflammatory range of
10 000 to 20 000/mm.3 4 Joint aspirate should be sent
for fungal and acid-fast bacilli smear, culture and
TB–polymerase chain reaction (TB-PCR) to identify
atypical organisms in refractory patients. Although
the high specificity and shorter turnaround time
of TB-PCR can complement cultures and help
achieve an early diagnosis of TB, culture remains the gold standard to exclude TB infection due to its
higher sensitivity. When synovial fluid aspirate is
inadequate, repeated aspiration or even arthroscopic
synovial biopsy should be considered. Autoimmune
markers should be determined to exclude an
autoimmune cause. Serial knee X-rays and MRIs
should be taken regularly to monitor disease
progression. In equivocal cases, arthroscopic
synovial biopsy can be performed. A typical
histological finding of caseating granuloma with
lymphocytic infiltration is diagnostic of TB.
Although arthrocentesis is less invasive, it has a
lower diagnostic sensitivity (80%) for knee TB than
synovial biopsy (90%).4
Tuberculosis of the knee can be managed
conservatively by 12 to 18 months of antituberculous
chemotherapy if identified early. With increasing joint
damage, surgical intervention including debridement,
synovectomy and arthroplasty might be necessary.
The long disease course of joint destruction leads to
fibrosis and ankylosis of the knee joint. Total knee
arthroplasty is regarded as a primary treatment for
advanced TB of the knee. Sultan et al5 suggest TKA
be performed 1 to 5 years following eradication of TB
to minimise reinfection risk. Postoperatively, 12 to 18
months of antituberculous drug therapy is believed to
be highly effective in preventing recurrent infection,
possibly due to the biofilm-lacking nature and poor
metal adherence of TB.5
Robotic arm–assisted TKA with varus-valgus
constrained insert was performed for our patient.
The use of a constrained implant facilitated greater
coronal plane stability in view of the extensive bone
loss, ankylosis and ligamentous laxity secondary to
prolonged TB infection. Robotic arm–assisted TKA
was adopted since it enables higher accuracy in bone
cutting and implant positioning than manual TKA.6
This is important for a patient receiving TKA at a
young age.
Tuberculosis of knee is rarely documented in
Hong Kong. This case highlights the importance of
recognising TB as an important differential diagnosis
of inflammatory arthritis. Maintaining a high index of suspicion will facilitate early diagnosis, potentially
sparing the patient from joint destruction and TKA
at a young age. In the event of recurrent knee effusion,
synovial fluid samples should be sent for TB-PCR in
addition to cell count, cytology, bacterial, acid-fast
bacilli smear and cultures. Total knee arthroplasty
plays a significant role in restoration of acceptable
ROM in a knee with extensive bone erosion and
ankylosis.
Author contributions
Concept or design: All authors.
Acquisition of data: All authors.
Analysis or interpretation of data: All authors.
Drafting of the manuscript: HMH Chan, H Fu.
Critical revision of the manuscript for important intellectual content: H Fu, KY Chiu.
Acquisition of data: All authors.
Analysis or interpretation of data: All authors.
Drafting of the manuscript: HMH Chan, H Fu.
Critical revision of the manuscript for important intellectual content: H Fu, KY Chiu.
All authors had full access to the data, contributed to the study, approved the final version for publication, and take responsibility for its accuracy and integrity.
Conflicts of interest
All authors have disclosed no conflicts of interest.
Funding/support
This study received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Ethics approval
The patient was treated in accordance with the Declaration of Helsinki and provided consent for publication of this case report.
References
1. Choi JA, Koh SH, Hong SH, Koh YH, Choi JY, Kang HS.
Rheumatoid arthritis and tuberculous arthritis:
differentiating MRI features. AJR Am J Roentgenol
2009;193:1347-53. Crossref
2. Margaretten ME, Kohlwes J, Moore D, Bent S. Does this
adult patient have septic arthritis? JAMA 2007;297:1478-88. Crossref
3. Horowitz DL, Katzap E, Horowitz S, Barilla-LaBarca ML.
Approach to septic arthritis. Am Fam Physician 2011;84:653-60.
4. Wallace R, Cohen AS. Tuberculous arthritis: a report of
two cases with review of biopsy and synovial fluid findings.
Am J Med 1976;61:277-82. Crossref
5. Sultan AA, Cantrell WA, Rose E, et al. Total knee
arthroplasty in the face of a previous tuberculosis infection of the knee: what do we know in 2018? Expert Rev Med
Devices 2018;15:717-24. Crossref
6. Hampp EL, Chughtai M, Scholl LY, et al. Robotic-arm
assisted total knee arthroplasty demonstrated greater
accuracy and precision to plan compared with manual
techniques. J Knee Surg 2019;32:239-50. Crossref

