Abstract
Background
Liver-directed therapies (LDT) are important components of the multidisciplinary care of patients with colorectal cancer liver metastases (CRCLM) that contribute to improved long-term outcomes. Factors associated with receipt of LDT are poorly understood.
Patients and Methods
Patients > 65 years old diagnosed with CRCLM were identified within the Medicare Standard Analytic File (2013–2017). Patients with extrahepatic metastatic disease were excluded. Mixed-effects analyses were used to assess patient factors associated with the primary outcome of LDT, defined as hepatectomy, ablation, and/or hepatic artery infusion chemotherapy (HAIC), as well as the secondary outcome of hepatectomy.
Results
Among 23,484 patients with isolated CRCLM, only 2004 (8.5%) received LDT, although resectability status could not be determined for the entire cohort. Among patients who received LDT, 61.7% underwent hepatectomy alone, 28.1% received ablation alone, 8.5% underwent hepatectomy and ablation, and 1.8% received HAIC either alone (0.8%) or in combination with hepatectomy and/or ablation (0.9%). Patient factors independently associated with lower odds of LDT included older age, female sex, Black race, greater comorbidity burden, higher social vulnerability index, primary rectal cancer, synchronous liver metastasis, and further distance from a high-volume liver surgery center (p < 0.05). Results were similar for receipt of hepatectomy.
Conclusions
Despite the well-accepted role of LDT for CRCLM, only a small proportion of Medicare beneficiaries with CRCLM receive LDT. Increasing access to specialized centers with expertise in LDT, particularly for Black patients, female patients, and those with higher levels of social vulnerability or long travel distances, may improve outcomes for patients with CRCLM.
Similar content being viewed by others
Colorectal cancer (CRC) is the third most common cause of cancer with an estimated annual incidence of 151,030 cases per year, and is the third leading cause of cancer death in the USA.1 The most common site of distant metastasis from CRC is the liver, with up to 25% of patients presenting with synchronous colorectal cancer liver metastasis (CRCLM) and as many as 50% of patients eventually developing metachronous CRCLM.2,3 While median overall survival with systemic chemotherapy alone is only 24 months, potentially curative liver-directed therapy (LDT), including hepatectomy, radiofrequency or microwave ablation, and/or hepatic artery infusion chemotherapy (HAIC), can be associated with 5-year overall survival as high as 60%.4,5
The definition for resectability of CRCLM in recent decades has expanded to include any patient in whom all primary and metastatic disease can be surgically removed with negative margins and an adequate future liver remnant can be maintained.6 Furthermore, modern systemic chemotherapy regimens,7,8,9,10,11 development of minimally invasive liver ablation techniques,12 and decreased morbidity associated with HAIC13,14 have led to improved survival and a further increase in the number of patients who may be eligible for curative-intent LDT. However, the definition of resectability and determination of which patients with CRCLM may benefit from LDT remains complex and highly variable across medical providers.15,16
Given the complexity in the assessment and decision-making regarding the surgical management of CRCLM and the limited number of available specialists and tertiary care centers in the USA, several prior studies have raised concerns regarding possible disparities in access to specialty care for patients with CRCLM.17,18,19 These studies utilized older data and focused only on surgical resection of CRCLM rather than LDT more broadly. Using national Medicare claims data, we seek to identify patient factors that contributed to specialty care on the basis of the hypothesis that significant disparities currently exist in receipt of various LDT modalities, including hepatectomy, ablation, and HAIC relative to patient race, socioeconomic status, and travel distance to specialty centers.
Patients and Methods
Data Sources
Medicare
Medicare beneficiaries > 65 years old with an initial diagnosis of colorectal cancer between 1 January 2013 and 31 March 2017 using International Classification of Diseases, Ninth Edition (ICD-9) and Tenth Edition (ICD-10) codes were identified within the Medicare 100% Inpatient Standard Analytic File (SAF). The SAF is managed by the Centers for Medicare and Medicaid Services (CMS) and includes patient-level inpatient, outpatient, skilled nursing facility, home health, and hospice claims data with respect to demographics, diagnoses, procedures, and costs. The claims are linked to the Medicare Limited Data Set Denominator and Master Beneficiary Summary Files to obtain insurance status and mortality data. Medicare SAF data were available from 1 January 2012 to 31 December 2017. Therefore, each patient had at least one year of “look back” claims to identify the initial diagnosis of colorectal cancer. Using similar methodology, the study cohort was then restricted to patients with an initial diagnosis of liver metastasis between 1 January 2013 and 31 March 2017 and either 60 days prior to or within 3 years following the initial diagnosis of colorectal cancer. Each patient had at least 9 months of potential follow-up following the initial diagnosis of liver metastasis. Further exclusion criteria included: (1) a diagnosis of other distant metastases prior to or within 180 days following the initial diagnosis of colorectal cancer; (2) a diagnosis of primary esophageal, gastric, small bowel, hepatopancreaticobiliary, or gynecologic cancer prior to or within 180 days following the initial diagnosis of liver metastasis; (3) discontinuous enrollment in Medicare Part A/B or HMO enrollment from the date of initial diagnosis of colorectal cancer through the date of death or end of the study period on 31 December 2017; and (4) missing county of residence for the patient. All administrative coding utilized for the study is presented in Table 1.
NIS
The Nationwide Inpatient Sample (NIS) was utilized to determine the proportion of Medicare beneficiaries who underwent hepatectomy (36.2%) for cancer between 2013 and 2016 to estimate the total annual hospital volume. The NIS is a part of the Healthcare Cost and Utilization Project and is the largest publicly available national all-payer hospital database with a weighted sample of > 35 million inpatient admissions in the USA annually.20 This methodology, using the NIS to estimate total volume for hospitals within Medicare claims, has been previously utilized and described.21,22 Using the estimated total annual hospital volume, hospitals were dichotomized into low- and high-volume liver surgery centers. Utilizing the lowest tertile of annual volume as the cutoff a priori, low-volume liver surgery centers were defined as hospitals that performed an average of < 20 liver resections for cancer per year, and high-volume liver surgery centers were defined as hospitals that performed an average of ≥ 20 liver resections for cancer per year.
Outcomes
The primary outcome was receipt of LDT within 365 days of the date of the initial liver metastasis diagnosis. LDT was defined as hepatectomy, percutaneous, laparoscopic, or open liver ablation, and/or receipt of hepatic artery infusion chemotherapy (HAIC) (Table 1). Other LDT modalities such as transarterial embolization (TAE) or chemoembolization (TACE), yttrium-90 (Y-90) radioembolization, and stereotactic body radiation therapy (SBRT) were not evaluated as these procedures are most often palliative in nature without a goal of cure. The secondary outcome was receipt of hepatectomy within 365 days of the date of the initial liver metastasis diagnosis.
Covariates
Patient factors included age (66–69, 70–79, or ≥ 80 years), sex, race (white, Black, or other), van Walraven Elixhauser comorbidity score, Centers for Disease Control and Prevention (CDC) Social Vulnerability Index characterized into quintiles, year of diagnosis, primary cancer site, synchronous versus metachronous CRCLM, and distance to the nearest high-volume liver surgery center. The van Walraven Elixhauser comorbidity score is a validated modification of the 30 Elixhauser binary comorbidity measures that uses a weighted score for each of the comorbidities to compute a single numeric score for administrative data using ICD-9/ICD-10 diagnosis codes.23,24 The CDC Social Vulnerability Index is a county-level estimate of the population’s social vulnerability based on 15 US census variables including socioeconomic status, household composition and disability, minority status and language, and housing type and transportation.25 Primary cancer site was categorized into right colon, left colon, unspecified colon site, and rectal cancer. Synchronous CRCLM was defined as an initial liver metastasis diagnosis date within 180 days of initial CRC diagnosis date, and metachronous CRCLM was defined as an initial liver metastasis diagnosis date 180 days or more after initial CRC diagnosis date. Distance to the nearest high-volume liver surgery center and distance to the nearest HAIC center were estimated using the great-circle distance in miles from the county centroid of the patient’s primary residence at the time of diagnosis to the county centroid of the nearest high-volume liver surgery center and nearest HAIC center, respectively, using the Haversine formula. This information was available through the National Bureau of Economic Research (NBER) and based upon the Federal Information Processing Standard Publication (FIPS) U.S. county codes using 2010 US census data.26
Statistical Analysis
Bivariate analyses were performed assessing the association between factors and receipt of LDT using chi-squared and Mann–Whitney U tests, and clinically appropriate factors were manually entered into multivariable analyses for the outcomes of LDT and hepatectomy. Two-level Bayesian multivariate mixed-effects analyses were performed accounting for clustering of patients at the county level while evaluating factors associated with the outcome measures.27,28 Weakly informative independent normal priors were specified for the log odds ratio, variance parameters were set to 1, covariances to 0, and the degree of belief to 0.002, and the Gibbs sampler was utilized to run Bayesian models for 13,000 Monte Carlo Markov chain iterations with a burn-in of 3000 iterations.22,29
Bayesian mixed-effects logistic regression analyses were performed using the MCMCglmm package in R version 4.1.0 (R Foundation for Statistical Computing, Vienna, Austria).29 All other analyses were performed using SAS 9.4 (SAS Institute, Cary, NC). The study was approved by the Institutional Review Board at the Ohio State University Wexner Medical Center.
Results
Study Cohort Characteristics
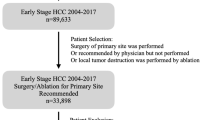
A total of 23,484 patients met inclusion criteria. Among 61,829 patients with an initial diagnosis of CRC and liver metastasis, a total of 38,345 patients were excluded owing to other distant metastatic disease (N = 24,869), another primary abdominal malignancy (N = 4857), discontinuous enrollment in Medicare Part A/B or HMO enrollment (N = 8523), or missing county of residence (N = 96).
The most common primary cancer site was right-sided colon cancer (32.9%; N = 7738) followed by left-sided colon cancer (29.9%; N = 7024), unspecified colon cancer site (20.4%; N = 4792), and rectal cancer (16.7%; N = 3930). The median age of the study cohort was 77 [interquartile range (IQR) = 71–84] years. A higher proportion of patients were male (52.4%; N = 12,310), of white (84.3%; N = 19,798) versus Black (10.8%; N = 2543) or other race/ethnicity (4.9%; N = 1,143) and had synchronous CRCLM (82.4%; N = 19,356) versus metachronous disease (17.6%; N = 4128). The median distance to the nearest high-volume liver surgery center was 40.4 (IQR = 13.7–83.6) miles, and 12.9% of patients (N = 3028) lived more than 120 miles from the nearest high-volume liver surgery center. The median distance to the nearest HAIC center was 130.2 (IQR = 68.7–247.3) miles, and 53% of patients (N = 12,449) lived more than 120 miles from the nearest HAIC center.
Liver-Directed Therapy (LDT)
Overall, 8.5% (N = 2004) underwent LDT with hepatectomy, liver ablation, and/or HAIC. Among patients who received LDT, 71.7% (N = 1437) underwent hepatectomy, 38.1% (N = 764) underwent liver ablation, and 1.8% (N = 36) received HAIC. Table 2 presents the bivariate analysis assessing factors associated with LDT and Table 3 presents the multivariable analyses assessing factors associated with LDT. Older age, female sex, Black race, higher comorbidity burden, lower socioeconomic status, primary rectal cancer, synchronous CRCLM, and further distance from the nearest high-volume liver surgery center were independently associated with lower odds of LDT.
Hepatectomy
Overall, 6.1% of patients underwent hepatectomy as the initial LDT modality. Table 3 presents the multivariable analyses assessing factors associated with hepatectomy. Results were similar to that of LDT. Specifically, older age, female sex, Black race, higher comorbidity burden, lower socioeconomic status, primary rectal cancer, synchronous metastasis, and further distance from the nearest high-volume liver surgery center were independently associated with lower odds of hepatectomy.
Discussion
Less than 10% of Medicare beneficiaries with CRCLM underwent LDT in the form of hepatectomy, ablation, and/or HAIC between 2013 and 2017. Furthermore, patients who were Black, had higher social vulnerability, or lived further away from a high-volume liver surgery center were less likely to undergo LDT or hepatectomy. These findings demonstrate that considerable disparities continue to exist in the treatment of CRCLM and highlight the importance of future research and interventions aimed at improving access to care for these at-risk patient populations.
Prior studies using older regional or national data noted similar disparities with respect to undergoing hepatectomy for CRCLM. In a retrospective cohort study by Neuwirth et al. using Surveillance, Epidemiology and End Results (SEER) Medicare data that included 11,351 patients diagnosed with synchronous CRCLM between 2000 and 2011, only 4.1% of patients underwent hepatectomy and 25% saw a surgeon after diagnosis.17 The authors similarly observed that Black patients and those living in ZIP codes with higher levels of poverty were significantly less likely to undergo surgical treatment. However, the study did not exclude patients with other sites of distant metastasis, included only patients with synchronous CRCLM, and focused only on receipt of hepatectomy, which may explain the lower rate of LDT compared with the current study.
In another retrospective population-based study using the California Cancer Registry between 2000 and 2012, Raoof et al. evaluated county-level variation in liver resection rates for synchronous CRCLM.18 The authors observed that the overall rate of hepatectomy was only 10% with county-level rates ranging from 0 to 33% with no improvement over the course of the study period. The authors also noted that Black patients and those with Medicaid insurance were significantly less likely to undergo hepatectomy and patients who underwent initial treatment at a National Cancer Institute-Designated Cancer Center or a high-volume liver surgery hospital were significantly more likely to undergo liver resection. In a study by Thornblade et al. using a similar study cohort using the California Cancer Registry, the authors observed that Black patients with CRCLM had lower median overall survival and lower rates of chemotherapy receipt and liver resection compared with white patients.19 However, there was no difference in overall survival between Black and white patients who underwent hepatectomy for CRCLM, suggesting that access to care may explain a significant proportion of the racial disparity in survival.
The reason for these low rates of LDT are likely multifactorial. The definition of “resectability” of CRCLM is complex and varies widely across providers and specialties. In a case-based survey of 112 medical oncologists in Michigan who treat colorectal cancer, the proportion of respondents who felt that specific patient factors were contraindications to hepatectomy varied with respect to extrahepatic disease (80.3%), poor performance status (77.7%), presence of more than four metastatic lesions (62.5%), bilobar metastases (43.8%), and metastasis size > 5 cm (40.2%).15 Furthermore, compared with low-referring physicians, high-referring medical oncologists were more likely to refer patients with moderate recurrence risk (82.8% versus 9%, p < 0.001) and high recurrence risk (31.0% vs. 10.7%, p = 0.05). In another survey of 64 medical oncologists and surgeons of various subspecialties in Canada using six clinical cases in which the patients ultimately underwent successful one- or two-stage hepatectomy and/or ablation of CRCLM, the proportion of cases considered to have resectable disease varied widely across physician specialties, including medical oncology (51%), colorectal surgery (52%), general surgery (61%), surgical oncology (75%), and hepatobiliary surgery (92%).16 While underestimation of resectability by providers appears to limit referrals to liver surgeons, another issue is geographic accessibility to a liver surgeon. In fact, up to 40% of referring providers report having no liver surgeons within their practice area.15 Furthermore, patients with CRCLM who receive care at experienced, high-volume liver surgery centers are more likely to receive surgery, and patients who are Black or have lower socioeconomic status are less likely to receive care at a high-volume hospital.18,30,31,32 This problem is likely reflected in the current study by the markedly decreased odds of LDT for patients living further away from a high-volume liver surgery center, Black patients, and patients with higher social vulnerability. Furthermore, patients who are socioeconomically disadvantaged may not have the financial means to travel to a liver surgery center.
Additional findings of the current study were that female patients and those with right-sided colon cancer or synchronous CRCLM were less likely to receive LDT. While no definitive conclusions can be made on the basis of data available within the study, these findings may be related to tumor biology. Female patients were more likely to have right-sided colon cancer (p < 0.0001) and synchronous CRCLM (p = 0.004) compared with male patients. Prior studies have demonstrated that right-sided colon cancer is associated with more extensive CRCLM and a higher likelihood of KRAS and BRAF mutations and microsatellite instability, which portend a worse prognosis, compared with left-sided colon cancer and rectal cancer, and synchronous CRCLM is associated with a higher burden of liver metastases, rate of bilobar disease, and risk of recurrence compared with metachronous CRCLM.33,34,35,36,37,38 Therefore, female patients and those with right-sided colon cancer or synchronous CRCLM may be less likely have CRCLM considered to be resectable or amenable to other LDT modalities. However, future study is warranted to determine whether there is a healthcare disparity related to female sex or if this finding is a reflection of more aggressive tumor biology.
There are several strategies that may help reduce these disparities in the treatment of CRCLM. Under ideal circumstances, all patients with oligometastatic CRCLM should undergo formal multidisciplinary review, including evaluation by a liver surgeon who has received specialized training in hepatobiliary surgery or complex general surgical oncology.30 Universal use of multidisciplinary tumor boards including medical oncologists, surgical oncologists/hepatobiliary surgeons, interventional radiologists, and radiation oncologists may help improve referral and rates of LDT. In fact, up to 44% of patients who are assigned palliative chemotherapy at tumor boards in which there is no liver surgeon present are later found to be potentially resectable following independent review by a liver surgeon.39 In geographic areas where there is no qualified liver surgeon, virtual tumor board or telemedicine referral and evaluation, which has been shown to be cost-effective and economically viable for specialized care especially during the COVID-19 pandemic, and the use of resources from organizations such as the Americas Hepato–Pancreato–Biliary Association that allow providers to remotely query hepatobiliary surgeons for multidisciplinary review and comment on specific cases may be alternative options.30,40,41 Educating various stakeholders including medical providers, policymakers, and payers regarding the expanding criteria for resectability of CRCLM and the efficacy of other LDT modalities may also lead to higher referral rates and the creation of financial assistance programs for disadvantaged patients with limited financial means and higher travel burden to the nearest liver surgery center. Assistance programs offering subsidized travel and accommodations may also be of particular benefit to patients who are candidates for HAIC and require outpatient visits every 2 weeks for filling of the pump with floxuridine.
While this is the first large study to investigate overall rates and disparities in use of LDT including hepatectomy, ablation, and HAIC using national data, there are several limitations. First, the Medicare SAF comprises administrative data that are susceptible to medical coding errors. In addition, oncologic staging is not available within the data. However, the use of diagnosis coding algorithms to identify metastatic disease in colorectal cancer within administrative claims data has been shown to have low false positive rates as evidenced by specificity > 90% in multiple validation studies.42,43 Furthermore, tumor biology such as TNM classification, histology, and presence of mutations and the location and burden of CRCLM that affect resectability and candidacy for LDT are not available within the Medicare claims. Therefore, the denominator of patients with CRCLM amenable to LDT could not be determined. However, with an estimated 15–20% of patients having resectable CRCLM at the time of initial diagnosis, the hepatectomy rate of 6.1% and overall LDT rate of 8.5% suggests that LDT was underutilized. An additional limitation is that the study cohort was necessarily restricted to patients > 65 years old with Medicare insurance. The rates of LDT are likely higher in younger patients with less comorbidity burden and better functional status. However, prior studies have demonstrated low rates of hepatectomy for CRCLM using all-payer population-based datasets.18,19 Furthermore, inclusion of only patients with Medicare insurance allowed for a focus on other disparities outside of insurance status. In addition, receipt of systemic therapy, which may increase resectability and candidacy for LDT in patients who initially have unresectable CRCLM, could not reliably be assessed within the Medicare claims data. Finally, patients may have undergone other LDT modalities, such as TAE, TACE, Y-90 radioembolization, and SBRT. However, these other modalities are most often palliative in nature and the focus of the study was on receipt of LDT with potentially curative intent.
Conclusions
Despite expanding criteria for the resectability of CRCLM and a continually growing body of literature supporting the use of LDT, only a small proportion of Medicare beneficiaries with CRLM undergo LDT. Future research focusing on increasing access to specialized centers with expertise in LDT and eliminating barriers to care, particularly for Black patients, female patients, and those with higher levels of social vulnerability or long travel distances, may improve outcomes for patients with CRCLM.
References
Siegel RL, Miller KD, Fuchs HE, Jemal A. Cancer statistics, 2022. CA Cancer J Clin. 2022;72(1):7–33.
Bozzetti F, Doci R, Bignami P, Morabito A, Gennari L. Patterns of failure following surgical resection of colorectal cancer liver metastases Rationale for a multimodal approach. Ann Surg. 1987;205(3):264–70.
Ekberg H, Tranberg KG, Andersson R, et al. Pattern of recurrence in liver resection for colorectal secondaries. World J Surg. 1987;11(4):541–7.
Kopetz S, Chang GJ, Overman MJ, et al. Improved survival in metastatic colorectal cancer is associated with adoption of hepatic resection and improved chemotherapy. J Clin Oncol. 2009;27(22):3677–83.
Pawlik TM, Scoggins CR, Zorzi D, et al. Effect of surgical margin status on survival and site of recurrence after hepatic resection for colorectal metastases. Ann Surg. 2005;241(5):715–722, discussion 722–714.
Pawlik TM, Schulick RD, Choti MA. Expanding criteria for resectability of colorectal liver metastases. Oncologist. 2008;13(1):51–64.
Pozzo C, Basso M, Cassano A, et al. Neoadjuvant treatment of unresectable liver disease with irinotecan and 5-fluorouracil plus folinic acid in colorectal cancer patients. Ann Oncol. 2004;15(6):933–9.
Falcone A, Ricci S, Brunetti I, et al. Phase III trial of infusional fluorouracil, leucovorin, oxaliplatin, and irinotecan (FOLFOXIRI) compared with infusional fluorouracil, leucovorin, and irinotecan (FOLFIRI) as first-line treatment for metastatic colorectal cancer: the Gruppo Oncologico Nord Ovest. J Clin Oncol. 2007;25(13):1670–6.
Souglakos J, Androulakis N, Syrigos K, et al. FOLFOXIRI (folinic acid, 5-fluorouracil, oxaliplatin and irinotecan) vs FOLFIRI (folinic acid, 5-fluorouracil and irinotecan) as first-line treatment in metastatic colorectal cancer (MCC): a multicentre randomised phase III trial from the Hellenic Oncology Research Group (HORG). Br J Cancer. 2006;94(6):798–805.
Modest DP, Martens UM, Riera-Knorrenschild J, et al. FOLFOXIRI plus panitumumab as first-line treatment of RAS wild-type metastatic colorectal cancer: the randomized, open-label, phase II VOLFI study (AIO KRK0109). J Clin Oncol. 2019;37(35):3401–11.
Tang W, Ren L, Liu T, et al. Bevacizumab plus mFOLFOX6 versus mFOLFOX6 alone as first-line treatment for RAS mutant unresectable colorectal liver-limited metastases: the BECOME randomized controlled trial. J Clin Oncol. 2020;38(27):3175–84.
Khajanchee YS, Hammill CW, Cassera MA, Wolf RF, Hansen PD. Hepatic resection vs minimally invasive radiofrequency ablation for the treatment of colorectal liver metastases: a Markov analysis. Arch Surg. 2011;146(12):1416–23.
Chan DL, Alzahrani NA, Morris DL, Chua TC. Systematic review and meta-analysis of hepatic arterial infusion chemotherapy as bridging therapy for colorectal liver metastases. Surg Oncol. 2015;24(3):162–71.
Levi FA, Boige V, Hebbar M, et al. Conversion to resection of liver metastases from colorectal cancer with hepatic artery infusion of combined chemotherapy and systemic cetuximab in multicenter trial OPTILIV. Ann Oncol. 2016;27(2):267–74.
Krell RW, Reames BN, Hendren S, et al. Surgical referral for colorectal liver metastases: a population-based survey. Ann Surg Oncol. 2015;22(7):2179–94. https://doi.org/10.1245/s10434-014-4318-x.
Aubin JM, Bressan AK, Grondin SC, et al. Assessing resectability of colorectal liver metastases: how do different subspecialties interpret the same data? Can J Surg. 2018;61(4):251–6.
Neuwirth MG, Epstein AJ, Karakousis GC, Mamtani R, Paulson EC. Disparities in resection of hepatic metastases in colon cancer. J Gastrointest Oncol. 2018;9(1):126–34.
Raoof M, Jutric Z, Haye S, et al. Systematic failure to operate on colorectal cancer liver metastases in California. Cancer Med. 2020;9(17):6256–67.
Thornblade LW, Warner S, Melstrom L, Singh G, Fong Y, Raoof M. Association of race/ethnicity with overall survival among patients with colorectal liver metastasis. JAMA Netw Open. 2020;3(9):e2016019.
NIS Overview. 2021; https://www.hcup-us.ahrq.gov/nisoverview.jsp. Accessed 7 March 2022.
Birkmeyer JD, Siewers AE, Finlayson EV, et al. Hospital volume and surgical mortality in the United States. N Engl J Med. 2002;346(15):1128–37.
Aquina CT, Becerra AZ, Fleming FJ, et al. Variation in outcomes across surgeons meeting the Leapfrog volume standard for complex oncologic surgery. Cancer. 2021;127(21):4059–71.
van Walraven C, Austin PC, Jennings A, Quan H, Forster AJ. A modification of the Elixhauser comorbidity measures into a point system for hospital death using administrative data. Med Care. 2009;47(6):626–33.
Quan H, Sundararajan V, Halfon P, et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care. 2005;43(11):1130–9.
CDC/ATSDR Social Vulnerability Index 2016 Database. https://www.atsdr.cdc.gov/placeandhealth/svi/data_documentation_download.html. Accessed 16 June 2021.
County Distance Database. https://www.nber.org/research/data/county-distance-database. Accessed 21 October 2020.
Gelman A, Hill J. Data analysis using regression and multilevel/hierarchical models. Cambridge; New York: Cambridge University Press; 2007.
Merlo J, Chaix B, Ohlsson H, et al. A brief conceptual tutorial of multilevel analysis in social epidemiology: using measures of clustering in multilevel logistic regression to investigate contextual phenomena. J Epidemiol Community Health. 2006;60(4):290–7.
Hadfield JD. MCMC Methods for multi-response generalized linear mixed models: the MCMCglmm R package. 2010. 2010;33(2):22.
Wei AC, Jarnagin WR. Questioning why more patients with colorectal liver metastases are not referred for metastasectomy. JAMA Surg. 2020;155(10):909–10.
Epstein AJ, Gray BH, Schlesinger M. Racial and ethnic differences in the use of high-volume hospitals and surgeons. Arch Surg. 2010;145(2):179–86.
Diaz A, Hyer JM, Azap R, Tsilimigras D, Pawlik TM. Association of social vulnerability with the use of high-volume and Magnet recognition hospitals for hepatopancreatic cancer surgery. Surgery. 2021;170(2):571–8.
Engstrand J, Nilsson H, Stromberg C, Jonas E, Freedman J. Colorectal cancer liver metastases—a population-based study on incidence, management and survival. BMC Cancer. 2018;18(1):78.
Margonis GA, Buettner S, Andreatos N, et al. Association of BRAF Mutations with survival and recurrence in surgically treated patients with metastatic colorectal liver cancer. JAMA Surg. 2018;153(7):e180996.
Charlton ME, Kahl AR, Greenbaum AA, et al. KRAS testing, tumor location, and survival in patients with stage IV colorectal cancer: SEER 2010–2013. J Natl Compr Canc Netw. 2017;15(12):1484–93.
Tsai MS, Su YH, Ho MC, et al. Clinicopathological features and prognosis in resectable synchronous and metachronous colorectal liver metastasis. Ann Surg Oncol. 2007;14(2):786–94. https://doi.org/10.1245/s10434-006-9215-5.
Konopke R, Kersting S, Distler M, et al. Prognostic factors and evaluation of a clinical score for predicting survival after resection of colorectal liver metastases. Liver Int. 2009;29(1):89–102.
Diehl TM, Abbott DE. Molecular determinants and other factors to guide selection of patients for hepatic resection of metastatic colorectal cancer. Curr Treat Options Oncol. 2021;22(9):82.
Vega EA, Salehi O, Nicolaescu D, et al. Failure to cure patients with colorectal liver metastases: the impact of the liver surgeon. Ann Surg Oncol. 2021;28(12):7698–706. https://doi.org/10.1245/s10434-021-10030-0.
Alkmim MB, Figueira RM, Marcolino MS, et al. Improving patient access to specialized health care: the Telehealth Network of Minas Gerais, Brazil. Bull World Health Organ. 2012;90(5):373–8.
Kichloo A, Albosta M, Dettloff K, et al. Telemedicine, the current COVID-19 pandemic and the future: a narrative review and perspectives moving forward in the USA. Fam Med Community Health. 2020;8(3).
Hassett MJ, Ritzwoller DP, Taback N, et al. Validating billing/encounter codes as indicators of lung, colorectal, breast, and prostate cancer recurrence using 2 large contemporary cohorts. Med Care. 2014;52(10):e65-73.
Whyte JL, Engel-Nitz NM, Teitelbaum A, Gomez Rey G, Kallich JD. An Evaluation of algorithms for identifying metastatic breast, lung, or colorectal cancer in administrative claims data. Med Care. 2015;53(7):e49-57.
Funding
None
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure
Aslam Ejaz is a consultant for Natera Inc. and an advisor for Delcath Inc.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Aquina, C.T., Brown, Z.J., Beane, J.D. et al. Disparities in Care Access to Liver-Directed Therapy Among Medicare Beneficiaries with Colorectal Cancer Liver Metastasis. Ann Surg Oncol 30, 335–344 (2023). https://doi.org/10.1245/s10434-022-12513-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-022-12513-0