Abstract
Background
Controversies exist among liver surgeons regarding clinical outcomes of the laparoscopic versus the robotic approach for major complex hepatectomies. The authors therefore designed a study to examine and compare the perioperative outcomes of laparoscopic left hepatectomy or extended left hepatectomy (L-LH/L-ELH) versus robotic left hepatectomy or extended left hepatectomy (R-LH/R-ELH) using a large international multicenter collaborative database.
Methods
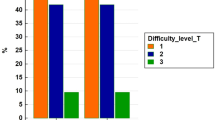
An international multicenter retrospective analysis of 580 patients undergoing L-LH/L-ELH or R-LH/R-ELH at 25 specialized hepatobiliary centers worldwide was undertaken. Propensity score-matching (PSM) was used at a 1:1 nearest-neighbor ratio according to 15 perioperative variables, including demographics, tumor characteristics, Child-Pugh score, presence of portal hypertension, multiple resections, histologic diagnosis, and Iwate difficulty grade.
Results
Before the PSM, 190 (32 %) patients underwent R-LH/R-ELH, and 390 (68 %) patients underwent L-LH/L-ELH. After the matching, 164 patients were identified in each arm without significant differences in demographics, preoperative variables, medical history, tumor pathology, tumor characteristics, or Iwate score. Regarding intra- and postoperative outcomes, the rebotic approach had significantly less estimated blood loss (EBL) (100 ml [IQR 200 ml] vs 200 ml [IQR 235 ml]; p = 0.029), fewer conversions to open operations (n = 4 [2.4 %] vs n = 13, [7.9 %]; p = 0.043), and a shorter hospital stay (6 days [IQR 3 days] vs 7 days [IQR 3.3 days]; p = 0.009).
Conclusion
Both techniques are safe and feasible in major hepatic resections. Compared with L-LH/L-ELH, R-LH/R-ELH is associated with less EBL, fewer conversions to open operations, and a shorter hospital stay.


Similar content being viewed by others

References
Miyasaka Y, Nakamura M, Wakabayashi G. Pioneers in laparoscopic hepato-biliary-pancreatic surgery. J Hepato-Biliary-Pancreatic Sci. 2018;25:109–11.
Ziogas IA, Giannis D, Esagian SM, Economopoulos KP, Tohme S, Geller DA. Laparoscopic versus robotic major hepatectomy: a systematic review and meta-analysis. Surg Endosc. 2021;35:524–35. https://doi.org/10.1007/s00464-020-08008-2 (Epub 28 September 2020 PMID: 32989544).
Goh BKP, Lee SY, Teo JY, et al. Changing trends and outcomes associated with the adoption of minimally invasive hepatectomy: a contemporary single-institution experience with 400 consecutive resections. Surg Endosc. 2018;32:4658–65.
Lai ECH, Tang CN. Training robotic hepatectomy: the Hong Kong experience and perspective. HepatoBiliary Surg Nutr. 2017;6:222–9.
Sucandy I, Luberice K, Lippert T, et al. Robotic major hepatectomy: an institutional experience and clinical outcomes. Ann Surg Oncol. 2020;27:4970–9.
Goh BKP, Lee SY, Koh YX, et al. Minimally invasive major hepatectomies: a Southeast Asian single-institution contemporary experience with its first 120 consecutive cases. ANZ J Surg. 2020;90:553–7.
Mathew RP, Venkatesh SK. Liver vascular anatomy: a refresher. Abdom Radiol. 2018;43:1886–95.
Nagino M, DeMatteo R, Lang H, et al. Proposal of a new comprehensive notation for hepatectomy: the “New World” terminology. Ann Surg. 2021;274:1–3.
Sucandy I, Schlosser S, Bourdeau T, et al. Robotic hepatectomy for benign and malignant liver tumors. J Robot Surg. 2020;14:75–80.
Broering D, Sturdevant ML, Zidan A. Robotic donor hepatectomy: a major breakthrough in living donor liver transplantation. Am J Transplant. 2022;22:14–23.
Gavriilidis P, Roberts KJ, Aldrighetti L, et al. A comparison between robotic, laparoscopic, and open hepatectomy: a systematic review and network meta-analysis. Eur J Surg Oncol. 2020;46:1214–24.
Sotiropoulos GC, Prodromidou A, Kostakis ID, et al. Meta-analysis of laparoscopic vs open liver resection for hepatocellular carcinoma. Updates Surg. 2017;69:291–311.
Sheetz KH, Claflin J, Dimick JB. Trends in the adoption of robotic surgery for common surgical procedures. JAMA Netwk Open. 2020;3(1):e1918911. https://doi.org/10.1001/jamanetworkopen.2019.18911.
Kamel MK, Tuma F, Keane CA, et al. National trends and perioperative outcomes of robotic-assisted hepatectomy in the USA: a propensity score-matched analysis from the National Cancer Database. World J Surg. 2022;46:189–96.
Chiow AKH, Fuks D, Choi GH, et al. International multicentre propensity score-matched analysis comparing robotic versus laparoscopic right posterior sectionectomy. Br J Surg. 2021;108:1513–20.
Yang HY, Choi GH, Chin KM, et al. Robotic and laparoscopic right anterior sectionectomy and central hepatectomy: multicentre propensity score-matched analysis. Br J Surg. 2022;109(4):311–14. https://doi.org/10.1093/bjs/znab463.
Chong CC, Fuks D, Lee K-F, et al. Propensity score-matched analysis comparing robotic and laparoscopic right and extended right hepatectomy. JAMA Surg. 2020;157(5):436–44. https://doi.org/10.1001/jamasurg.2022.0161.
Kawaguchi Y, Fuks D, Kokudo N, et al. Difficulty of laparoscopic liver resection. Ann Surg. 2018;267:13–7.
Clavien PA, Barkun J, de Oliveira ML, et al. The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg. 2009;250:187–96.
Tanaka S, Kawaguchi Y, Kubo S, et al. Validation of index-based IWATE criteria as an improved difficulty scoring system for laparoscopic liver resection. Surg United States. 2019;165:731–40.
Ban D, Tanabe M, Ito H, et al. A novel difficulty scoring system for laparoscopic liver resection. J Hepatobiliary Pancreat Sci. 2014;21:745–53. https://doi.org/10.1002/jhbp.166 (PMID: 25242563).
Tsung A, Geller DA, Sukato DC, et al. Robotic versus laparoscopic hepatectomy: a matched comparison. Ann Surg. 2014;259:549–55.
Cipriani F, Fiorentini G, Magistri P, et al. Pure laparoscopic versus robotic liver resections: multicentric propensity score-based analysis with stratification according to difficulty scores. J Hepato-Biliary-Pancreatic Sci. Epub ahead of print 2021. DOI: https://doi.org/10.1002/jhbp.1022.
Cai JP, Chen W, Chen LH, et al. Comparison between robotic-assisted and laparoscopic left hemi-hepatectomy. Asian J Surg. 2022;45:265–8.
Hu Y, Guo K, Xu J, et al. Robotic versus laparoscopic hepatectomy for malignancy: a systematic review and meta-analysis. Asian J Surg. 2021;44:615–28.
Acknowledgement
International robotic and laparoscopic liver resection study group investigators: Chung-Yip Chan (Department of Hepatopancreatobiliary and Transplant Surgery, Singapore General Hospital and National Cancer Centre Singapore, Singapore); Mizelle D’Silva (Department of Surgery, Seoul National University Hospital Bundang, Seoul National University College of Medicine, Seoul, Korea); Henri Schotte (Department of Digestive and Hepatobiliary/Pancreatic Surgery, Groeninge Hospital, Kortrijk, Belgium); Celine De Meyere (Department of Digestive and Hepatobiliary/Pancreatic Surgery, Groeninge Hospital, Kortrijk, Belgium); Felix Krenzien (Department of Surgery, Campus Charité Mitte and Campus Virchow-Klinikum, Charité-Universitätsmedizin, Corporate Member of Freie Universität Berlin, and Berlin Institute of Health, Berlin, Germany); Moritz Schmelzle (Department of Surgery, Campus Charité Mitte and Campus Virchow-Klinikum, Charité-Universitätsmedizin, Corporate Member of Freie Universität Berlin, and Berlin Institute of Health, Berlin, Germany); Prashant Kadam (Department of Hepatopancreatobiliary and Liver Transplant Surgery, University Hospitals Birmingham NHS Foundation Trust, Birmingham, UK); Roberto Montalti (Department of Clinical Medicine and Surgery, Division of HPB, Minimally Invasive and Robotic Surgery, Federico II University Hospital Naples, Naples, Italy); Qu Liu (Faculty of Hepatopancreatobiliary Surgery, The First Medical Center of Chinese People’s Liberation Army (PLA) General Hospital, Beijing, China); Kit-Fai Lee (Division of Hepatobiliary and Pancreatic Surgery, Department of Surgery, Prince of Wales Hospital, The Chinese University of Hong Kong, New Territories, Hong Kong SAR, China; Diana Salimgereeva (Department of Hepato-Pancreato-Biliary Surgery, Moscow Clinical Scientific Center, Moscow, Russia); Ruslan Alikhanov (Department of Hepato-Pancreato-Biliary Surgery, Moscow Clinical Scientific Center, Moscow, Russia); Lip Seng Lee (Hepatopancreatobiliary Unit, Department of Surgery, Changi General Hospital, Singapore); Mikel Gastaca (Hepatobiliary Surgery and Liver Transplantation Unit, Biocruces Bizkaia Health Research Institute, Cruces University Hospital, University of the Basque Country, Bilbao, Spain); Jae Young Jang (Department of General Surgery, CHA Bundang Medical Center, CHA University School of Medicine, Seongnam, Korea); Chetana Lim (Department of Digestive, HBP and Liver Transplantation, Hopital Pitie-Salpetriere, APHP, Sorbonne Université, Paris, France); Kevin P. Labadie (Department of Surgery, University of Washington Medical Center. Seattle, WA, USA)
Funding
Dr. Kingham was partially supported by the US National Cancer Center Institute MSKCC Core Grant Number P30 CA008747 for this study.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Disclosure
Dr Brian K. P. Goh has received travel grants and honorarium from Johnson and Johnson and Transmedic, the local distributor for the Da Vinci robot. Dr Marco V. Marino is a consultant for CAVA robotics LLC. Johann Pratschke reports a research grant from Intuitive Surgical Deutschland GmbH and personal fees or non-financial support from Johnson & Johnson, Medtronic, AFS Medical, Astellas, CHG Meridian, Chiesi, Falk Foundation, La Fource Group, Merck, Neovii, NOGGO, pharma-consult Peterson, and Promedicis. Moritz Schmelzle reports personal fees or other support outside of the submitted work from Merck, Bayer, ERBE, Amgen, Johnson & Johnson, Takeda, Olympus, Medtronic, Intuitive. Fernando Rotellar reports speaker fees and support outside the submitted work from Integra, Medtronic, Olympus, Corza, Sirtex and Johnson & Johnson. The remaining authors haved no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Sucandy, I., Rayman, S., Lai, E.C. et al. Robotic Versus Laparoscopic Left and Extended Left Hepatectomy: An International Multicenter Study Propensity Score-Matched Analysis. Ann Surg Oncol 29, 8398–8406 (2022). https://doi.org/10.1245/s10434-022-12216-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-022-12216-6


