Abstract
Introduction
Small intestinal neuroendocrine tumors (SI-NETs) often present with metastatic disease. An ongoing debate exists on whether to perform primary tumor resection (PTR) in patients with stage IV SI-NETs, without symptoms of the primary tumor and inoperable metastatic disease.
Objective
The aim of this study was to compare a treatment strategy of upfront surgical resection versus a surveillance strategy of watch and wait.
Methods
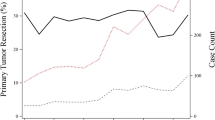
This was a retrospective cohort study of patients with stage IV SI-NETs at diagnosis, between 2000 and 2018, from two tertiary referral centers (Netherlands Cancer Institute [NKI] and Aintree University Hospital [AUH]) who had adopted contrasting treatment approaches: upfront surgical resection and watch and wait, respectively. Patients without symptoms related to the primary tumor were included. Multivariable intention-to-treat (ITT), per-protocol (PP), and instrumental variable (IV) analyses using ‘institute’ as an IV were performed to assess the influence of PTR on disease-specific mortality (DSM).
Results
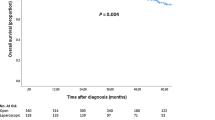
A total of 557 patients were identified, with 145 patients remaining after exclusion of stage I–III disease or symptoms of the primary tumor (93 from the NKI and 52 from AUH). The cohorts differed in performance status (PS; p = 0.006) and tumor grade (p < 0.001). PTR was independently associated with reduced DSM irrespective of statistical methods employed: ITT hazard ratio [HR] 0.60, p = 0.005; PP HR 0.58, p < 0.001; and IV HR 0.07, p = 0.019. Other factors associated with DSM were age, PS, high chromogranin A, and somatostatin analog treatment.
Conclusion
Taking advantage of contrasting institutional treatment strategies, this study identified PTR as an independent predictor of DSM. Future prospective studies should aim to validate these results.


Similar content being viewed by others
References
Dasari A, Shen C, Halperin D, et al. Trends in the incidence, prevalence, and survival outcomes in patients with neuroendocrine tumors in the United States. JAMA Oncol. 2017;3(10):1335.
Hallet J, Law CH, Cukier M, Saskin R, Liu N, Singh S. Exploring the rising incidence of neuroendocrine tumors: a population-based analysis of epidemiology, metastatic presentation, and outcomes. Cancer. 2015;121(4):589–97.
Huguet I, Grossman AB, O’Toole D. Changes in the epidemiology of neuroendocrine tumours. Neuroendocrinology. 2017;104(2):105–11.
Fraenkel M, Kim M, Faggiano A, de Herder WW, Valk GD. Incidence of gastroenteropancreatic neuroendocrine tumours: a systematic review of the literature. Endocr Relat Cancer. 2014;21(3):R153-163.
Rodriguez Laval V, Pavel M, Steffen IG, et al. Mesenteric fibrosis in midgut neuroendocrine tumors: functionality and radiological features. Neuroendocrinology. 2018;106(2):139–47.
Laskaratos FM, Rombouts K, Caplin M, Toumpanakis C, Thirlwell C, Mandair D. Neuroendocrine tumors and fibrosis: an unsolved mystery? Cancer. 2017;123(24):4770–90.
Laskaratos FM, Walker M, Wilkins D, et al. Evaluation of clinical prognostic factors and further delineation of the effect of mesenteric fibrosis on survival in advanced midgut neuroendocrine tumours. Neuroendocrinology. 2018;107(3):292–304.
Kasai Y, Mahuron K, Hirose K, et al. Prognostic impact of a large mesenteric mass > 2 cm in ileal neuroendocrine tumors. J Surg Oncol. 2019;120(8):1311–7.
Howe JR. It may not be too little or too late: resecting primary small bowel neuroendocrine tumors in the presence of metastatic disease. Ann Surg Oncol. 2020;27(8):2583–5. https://doi.org/10.1245/s10434-020-08695-0.
Zheng M, Li Y, Li T, Zhang L, Zhou L. Resection of the primary tumor improves survival in patients with gastro-entero-pancreatic neuroendocrine neoplasms with liver metastases: a SEER-based analysis. Cancer Med. 2019;8(11):5128–36.
Fisher AT, Titan AL, Foster DS, et al. Management of ileal neuroendocrine tumors with liver metastases. J Gastrointest Surg. 2020;24(7):1530–9.
Ahmed A, Turner G, King B, et al. Midgut neuroendocrine tumours with liver metastases: results of the UKINETS study. Endocr Relat Cancer. 2009;16(3):885–94.
Givi B, Pommier SJ, Thompson AK, Diggs BS, Pommier RF. Operative resection of primary carcinoid neoplasms in patients with liver metastases yields significantly better survival. Surgery. 2006;140(6):891–7 (discussion 897–898).
Gangi A, Manguso N, Gong J, et al. Midgut neuroendocrine tumors with liver-only metastases: benefit of primary tumor resection. Ann Surg Oncol. 2020;27(11):4525–32. https://doi.org/10.1245/s10434-020-08510-w.
Niederle B, Pape U. ENETS consensus guidelines update for neuroendocrine neoplasms of the jejunum and ileum. Neuroendocrinology. 2016;103:125–36.
Daskalakis K, Karakatsanis A, Hessman O, et al. Association of a prophylactic surgical approach to stage IV small intestinal neuroendocrine tumors with survival. JAMA Oncol. 2018;4(2):183–9.
Nagtegaal ID, Odze RD, Klimstra D, et al. The 2019 WHO classification of tumours of the digestive system. Histopathology. 2020;76(2):182–8.
Smets YFC, Westendorp RGJ, van der Pijl JW, et al. Effect of simultaneous pancreas-kidney transplantation on mortality of patients with type-1 diabetes mellitus and end-stage renal failure. Lancet. 1999;353(9168):1915–9.
Uddin MJ, Groenwold RH, Ali MS, et al. Methods to control for unmeasured confounding in pharmacoepidemiology: an overview. Int J Clin Pharm. 2016;38(3):714–23.
Martens EP, Pestman WR, de Boer A, Belitser SV, Klungel OH. Instrumental variables: application and limitations. Epidemiology. 2006;17(3):260–7.
Rassen JA, Brookhart MA, Glynn RJ, Mittleman MA, Schneeweiss S. Instrumental variables I: instrumental variables exploit natural variation in nonexperimental data to estimate causal relationships. J Clin Epidemiol. 2009;62(12):1226–32.
Freemantle N, Calvert M, Wood J, Eastaugh J, Griffin C. Composite outcomes in randomized trials: greater precision but with greater uncertainty? JAMA. 2003;289(19):2554–9.
Lauer MS, Topol EJ. Clinical trials—multiple treatments, multiple end points, and multiple lessons. JAMA. 2003;289(19):2575–7.
Montori VM, Permanyer-Miralda G, Ferreira-Gonzáles I, et al. Validity of composite end points in clinical trials. BMJ. 2021;330:594–6.
Hernan MA, Schisterman EF, Hernandez-Diaz S. Invited commentary: composite outcomes as an attempt to escape from selection bias and related paradoxes. Am J Epidemiol. 2014;179(3):368–70.
Austin PC. Balance diagnostics for comparing the distribution of baseline covariates between treatment groups in propensity-score matched samples. Stat Med. 2009;28(25):3083–107.
Sjolander A, Martinussen T. Instrumental variable estimation with the R Package ivtools. Epidemiol Methods. 2019. https://doi.org/10.1515/em-2018-0024.
Rubin DB. Multiple imputation for nonresponse in surveys. Hoboken: John Wiley & Sons Inc.; 1987.
Barnard J, Rubin DB. Small-sample degrees of freedom with multiple imputation. Biometrika. 1999;86(4):948–55.
van Buuren S, Groothuis-Oudshoorn K. mice: multivariate imputation by chained equations in R. J Stat Softw. 2011;45(3):1–67.
Kivrak Salim D, Bayram S, Gomceli I, et al. Palliative resection of primary site in advanced gastroenteropancreatic neuroendocrine tumors improves survivals. Turk J Gastroenterol. 2019;30(10):910–6.
Tierney JF, Chivukula SV, Wang X, et al. Resection of primary tumor may prolong survival in metastatic gastroenteropancreatic neuroendocrine tumors. Surgery. 2019;165(3):644–51.
Rinke A, Wittenberg M, Schade-Brittinger C, et al. Placebo controlled, double blind, prospective, randomized study on the effect of octreotide lar in the control of tumor growth in patients with metastatic neuroendocrine midgut tumors (PROMID): results of long-term survival. Neuroendocrinology. 2017;104(1):26–32.
van der Wal GE, Gouw AS, Kamps JA, et al. Angiogenesis in synchronous and metachronous colorectal liver metastases: the liver as a permissive soil. Ann Surg. 2012;255(1):86–94.
Danna EA, Sinha P, Gilbert MR, Clements VK, Pulaski BA, Ostrand-Rosenberg S. Surgical removal of primary tumor reverses tumor-induced immunosuppression despite the presence of metastatic disease. Cancer Res. 2004;64:2205–11.
Peinado H, Zhang H, Matei IR, et al. Pre-metastatic niches: organ-specific homes for metastases. Nat Rev Cancer. 2017;17(5):302–17.
Kim RS, Avivar-Valderas A, Estrada Y, et al. Dormancy signatures and metastasis in estrogen receptor positive and negative breast cancer. PloS One. 2012;7(4):e35569.
Foulds CE. Disrupting a negative feedback loop drives endocrine therapy-resistant breast cancer. Proc Natl Acad Sci U S A. 2018;115(33):8236–8.
Allemani C, Weir HK, Carreira H, et al. Global surveillance of cancer survival 1995–2009: analysis of individual data for 25 676 887 patients from 279 population-based registries in 67 countries (CONCORD-2). Lancet. 2015;385(9972):977–1010.
Acknowledgment
The authors thank all the patients, investigators of the study and supporting teams at both participating centers. They also thank Rob Kessels and Mutamba Kayembe for statistical coding support.
Funding
No funding was received for this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Daniel J. Cuthbertson declares to have received consultancy fees and/or investigator-initiated research support from IPSEN and Novartis. Stephen W. Fenwick declares to have received funding to support a nurse educational event. Sonja Levy, James D. Arthur, Melissa Banks, Niels F.M. Kok, Rafael Diaz-Nieto, Monique E. van Leerdam, Gerlof D. Valk, Koert F.D. Kuhlmann, and Margot E.T. Tesselaar have no conflicts of interest to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Levy, S., Arthur, J.D., Banks, M. et al. Primary Tumor Resection is Associated with Improved Disease-Specific Mortality in Patients with Stage IV Small Intestinal Neuroendocrine Tumors (NETs): A Comparison of Upfront Surgical Resection Versus a Watch and Wait Strategy in Two Specialist NET Centers. Ann Surg Oncol 29, 7822–7832 (2022). https://doi.org/10.1245/s10434-022-12030-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-022-12030-0