Abstract
Background
Postoperative pneumonia is a common complication after esophagectomy and is associated with a high mortality rate. Although many randomized, controlled trials have been conducted on the prevention of postoperative pneumonia, little attention has been paid to the efficacy of antimicrobial prophylaxis. The purpose of this study was to investigate the impact of antimicrobial prophylaxis on the prevention of postoperative pneumonia.
Methods
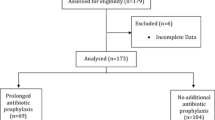
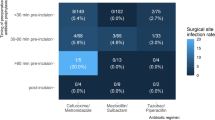
Data of patients with esophageal cancer who underwent thoracoscopic esophagectomy between 2016 and 2020 were collected. Early-period patients received cefazolin (CEZ) per protocol as antimicrobial prophylaxis (n = 250), and later-period patients received ampicillin/sulbactam (ABPC/SBT) (n = 106) because of the unavailability of CEZ in Japan. The incidence of pneumonia was compared between treatments in this quasi-experimental setting. Pneumonia detected by routine computed tomography (CT) on postoperative Days 5–6 was defined as early-onset pneumonia, and pneumonia that developed later was defined as late-onset pneumonia.
Results
The incidence of early-onset pneumonia was significantly lower (3.8% vs. 13.6%, P = 0.006), and the median length of postoperative hospital stay was significantly shorter (17 vs. 20 days, P < 0.001) in the ABPC/SBT group than in the CEZ group. The incidence of late-onset pneumonia was similar between groups (9.4% vs. 10.0%, P = 0.870). The incidence of Clostridioides difficile infections and the incidence of multidrug-resistant organisms were similar between groups. Multivariate analyses consistently showed the superiority of ABPC/SBT to CEZ in preventing early-onset pneumonia (odds ratio: 0.20, P = 0.006).
Conclusions
ABPC/SBT after esophagectomy was better at preventing early-onset pneumonia compared with CEZ and was feasible regarding the development of antimicrobial resistance.



Similar content being viewed by others
References
Finks JF, Osborne NH, Birkmeyer JD. Trends in hospital volume and operative mortality for high-risk surgery. N Engl J Med. 2011;364(22):2128–37.
Takeuchi H, Miyata H, Gotoh M, et al. A risk model for esophagectomy using data of 5354 patients included in a Japanese nationwide web-based database. Ann Surg. 2014;260(2):259–66.
Low DE, Kuppusamy MK, Alderson D, et al. Benchmarking complications associated with esophagectomy. Ann Surg. 2019;269(2):291–8.
Biere SS, van Berge Henegouwen MI, Maas KW, et al. Minimally invasive versus open oesophagectomy for patients with oesophageal cancer: a multicentre, open-label, randomised controlled trial. Lancet. 2012;379(9829):1887–92.
Mariette C, Markar SR, Dabakuyo-Yonli TS, et al. Hybrid minimally invasive esophagectomy for esophageal cancer. N Engl J Med. 2019;380(2):152–62.
Takesue T, Takeuchi H, Ogura M, et al. A prospective randomized trial of enteral nutrition after thoracoscopic esophagectomy for esophageal cancer. Ann Surg Oncol. 2015;22(Suppl 3):S802–9.
Kanekiyo S, Takeda S, Iida M, et al. Efficacy of perioperative immunonutrition in esophageal cancer patients undergoing esophagectomy. Nutrition. 2019;59:96–102.
Mudge LA, Watson DI, Smithers BM, et al. Multicentre factorial randomized clinical trial of perioperative immunonutrition versus standard nutrition for patients undergoing surgical resection of oesophageal cancer. Br J Surg. 2018;105(10):1262–72.
Yokoyama Y, Nishigaki E, Abe T, et al. Randomized clinical trial of the effect of perioperative synbiotics versus no synbiotics on bacterial translocation after oesophagectomy. Br J Surg. 2014;101(3):189–99.
Valkenet K, Trappenburg JCA, Ruurda JP, et al. Multicentre randomized clinical trial of inspiratory muscle training versus usual care before surgery for oesophageal cancer. Br J Surg. 2018;105(5):502–11.
van Adrichem EJ, Meulenbroek RL, Plukker JT, Groen H, van Weert E. Comparison of two preoperative inspiratory muscle training programs to prevent pulmonary complications in patients undergoing esophagectomy: a randomized controlled pilot study. Ann Surg Oncol. 2014;21(7):2353–60.
Radu DM, Jaureguy F, Seguin A, et al. Postoperative pneumonia after major pulmonary resections: an unsolved problem in thoracic surgery. Ann Thorac Surg. 2007;84(5):1669–73.
Bratzler DW, Dellinger EP, Olsen KM, et al. Clinical practice guidelines for antimicrobial prophylaxis in surgery. Am J Health Syst Pharm. 2013;70(3):195–283.
Schussler O, Dermine H, Alifano M, et al. Should we change antibiotic prophylaxis for lung surgery? Postoperative pneumonia is the critical issue. Ann Thorac Surg. 2008;86(6):1727–33.
Briez N, Piessen G, Bonnetain F, et al. Open versus laparoscopically-assisted oesophagectomy for cancer: a multicentre randomised controlled phase III trial—the MIRO trial. BMC Cancer. 2011;11:310.
Hochreiter M, Uhling M, Sisic L, et al. Prolonged antibiotic prophylaxis after thoracoabdominal esophagectomy does not reduce the risk of pneumonia in the first 30 days: a retrospective before-and-after analysis. Infection. 2018;46(5):617–24.
Yuda M, Yamashita K, Okamura A, et al. Influence of preoperative oropharyngeal microflora on the occurrence of postoperative pneumonia and survival in patients undergoing esophagectomy for esophageal cancer. Ann Surg. 2020;272(6):1035–43.
Nishigaki E, Abe T, Yokoyama Y, et al. The detection of intraoperative bacterial translocation in the mesenteric lymph nodes is useful in predicting patients at high risk for postoperative infectious complications after esophagectomy. Ann Surg. 2014;259(3):477–84.
Fujita T, Daiko H. Optimal duration of prophylactic antimicrobial administration and risk of postoperative infectious events in thoracic esophagectomy with three-field lymph node dissection: short-course versus prolonged antimicrobial administration. Esophagus. 2015;12(1):38–43.
Takesue Y, Kishimoto H, Kubo S, et al. Clinical practice guidelines for appropriate antimicrobial prophylaxis against postoperative infections. J Jpn Soc Surg Infect. 2016;13(2):79–158.
Abe T, Hosoi T, Kawai R, et al. Perioperative enteral supplementation with glutamine, fiber, and oligosaccharide reduces early postoperative surgical stress following esophagectomy for esophageal cancer. Esophagus. 2019;16(1):63–70.
Takatsu J, Higaki E, Hosoi T, et al. Clinical benefits of a swallowing intervention for esophageal cancer patients after esophagectomy. Dis Esophagus. 2020;34(5):doaa094.
Cunha BA. Pneumonia Essentials. 3rd edn. Royal Oak, Michigan: Physicians’ Press; 2010.
Low DE, Alderson D, Cecconello I, et al. International consensus on standardization of data collection for complications associated with esophagectomy: esophagectomy complications consensus group (ECCG). Ann Surg. 2015;262(2):286–94.
Society AT, America IDSO. Guidelines for the management of adults with hospital-acquired, ventilator-associated, and healthcare-associated pneumonia. Am J Respir Crit Care Med. 2005;171(4):388–416.
Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21(11):1539–58.
Rafailidis PI, Ioannidou EN, Falagas ME. Ampicillin/sulbactam: current status in severe bacterial infections. Drugs. 2007;67(13):1829–49.
Metlay JP, Waterer GW, Long AC, et al. Diagnosis and treatment of adults with community-acquired pneumonia. An official clinical practice guideline of the American thoracic society and infectious diseases society of America. Am J Respir Crit Care Med. 2019;200(7):e45-67.
Shimura S, Watari H, Komatsu M, et al. Antimicrobial susceptibility surveillance of obligate anaerobic bacteria in the Kinki area. J Infect Chemother. 2019;25(11):837–44.
Marik PE, Careau P. The role of anaerobes in patients with ventilator-associated pneumonia and aspiration pneumonia: a prospective study. Chest. 1999;115(1):178–83.
Hata R, Noguchi S, Kawanami T, et al. Poor oral hygiene is associated with the detection of obligate anaerobes in pneumonia. J Periodontol. 2020;91(1):65–73.
Yamasaki K, Kawanami T, Yatera K, et al. Significance of anaerobes and oral bacteria in community-acquired pneumonia. PLoS ONE. 2013;8(5):e63103.
Schlottmann F, Strassle PD, Charles AG, Patti MG. Esophageal cancer surgery: spontaneous centralization in the US contributed to reduce mortality without causing health disparities. Ann Surg Oncol. 2018;25(6):1580–7.
Kalff MC, Fransen LFC, de Groot EM, et al. Long-term survival after minimally invasive versus open esophagectomy for esophageal cancer: a nationwide propensity-score matched analysis. Ann Surg. 2020; Publish Ahead of Print.
Sakamoto T, Fujiogi M, Matsui H, Fushimi K, Yasunaga H. Comparing perioperative mortality and morbidity of minimally invasive esophagectomy versus open esophagectomy for esophageal cancer: a nationwide retrospective analysis. Ann Surg. 2021;274(2):324–30.
Length of hospital stay by country for acute care based on OECD databse. 2019. https://data.oecd.org/healthcare/length-of-hospital-stay.htm. Accessed 19 July 2021.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure
All of the authors declare that they have no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Higaki, E., Abe, T., Fujieda, H. et al. Significance of Antimicrobial Prophylaxis for the Prevention of Early-Onset Pneumonia After Radical Esophageal Cancer Resection: A Retrospective Analysis of 356 Patients Undergoing Thoracoscopic Esophagectomy. Ann Surg Oncol 29, 1374–1387 (2022). https://doi.org/10.1245/s10434-021-10867-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-021-10867-5