Abstract
Background
Minimally invasive surgical (MIS) staging is the standard treatment approach for clinical stage I endometrial cancer. Historical rates of inoperability in endometrial cancer are approximately 10%. Given surgical and medical advancements against increasing population obesity, we aimed to describe a contemporary incidence of medical inoperability in clinical stage I endometrial cancer.
Patients and Methods
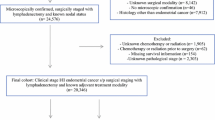
Patients diagnosed with clinical stage I endometrial cancer of any histology from April 2014 to December 2018 were included in this retrospective cohort study. The primary outcome, medical inoperability, was defined as (1) patients deemed inoperable by a gynecologic oncologist at initial consultation, (2) patients deemed inoperable during preoperative clearance, or (3) an aborted hysterectomy. Fisher’s exact or χ2, and Student’s t-test or Wilcoxon rank sum test were used, as appropriate, for data analysis. Multivariable logistic regression was also employed.
Results
Overall, 767 patients were included, of which 4.6% (35/767) were determined to be inoperable. The inoperable group had a higher body mass index (52.7 vs. 33.9, p < 0.001), and increased rates of diabetes (62.8%, 22/35 vs. 27.1%, 199/732, p < 0.001), coronary artery disease (31.4%, 11/35 vs. 7.1%, 52/732, p < 0.001), and hypertension (94.3%, 33/35 vs. 70.2%, 514/732, p < 0.001). Of those with attempted surgical staging, hysterectomy was aborted intraoperatively in 0.68% (5/737). The overall complication rate was 11.6% (86/737).
Conclusions
With maximal surgical effort and MIS, hysterectomy is possible in > 95% of patients with newly diagnosed endometrial cancer treated at a high-volume center. Complication rates were comparable to other trials evaluating the safety of MIS staging for endometrial cancer.


Similar content being viewed by others
References
Adult Obesity Facts|Overweight & Obesity | CDC. https://www.cdc.gov/obesity/data/adult.html. Accessed 15 Dec 2019.
Ward ZJ, Bleich SN, Cradock AL, et al. Projected U.S. state-level prevalence of adult obesity and severe obesity. N Engl J Med. 2019;381(25):2440–50. https://doi.org/10.1056/NEJMsa1909301.
Uterine Cancer-Cancer Stat Facts. https://seer.cancer.gov/statfacts/html/corp.html. Accessed 15 Dec 2019.
MacKintosh M, Crosbie E. Obesity-driven endometrial cancer: is weight loss the answer? BJOG An Int J Obstet Gynaecol. 2013;120(7):791–4. https://doi.org/10.1111/1471-0528.12106.
Wysham WZ, Kim KH, Roberts JM, et al. Obesity and perioperative pulmonary complications in robotic gynecologic surgery. Am J Obstet Gynecol. 2015;213(1):33.e1-33.e7. https://doi.org/10.1016/j.ajog.2015.01.033.
Giugale LE, Di Santo N, Smolkin ME, Havrilesky LJ, Modesitt SC. Beyond mere obesity: effect of increasing obesity classifications on hysterectomy outcomes for uterine cancer/hyperplasia. Gynecol Oncol. 2012;127(2):326–31. https://doi.org/10.1016/j.ygyno.2012.08.014.
Walker JL, Piedmonte MR, Spirtos NM, et al. Laparoscopy compared with laparotomy for comprehensive surgical staging of uterine cancer: Gynecologic Oncology Group Study LAP2. J Clin Oncol. 2009;27(32):5331–6. https://doi.org/10.1200/JCO.2009.22.3248.
Staples JN, Rauh L, Peach MS, Baker WD, Modesitt SC. Endometrial cancer in an increasingly obese population: exploring alternative options when surgery may not cut it. Gynecol Oncol Rep. 2018. https://doi.org/10.1016/j.gore.2018.04.009.
Obermair A, Manolitsas TP, Leung Y, Hammond IG, Mccartney AJ. Total laparoscopic hysterectomy versus total abdominal hysterectomy for obese women with endometrial cancer. Int J Gynecol Cancer. 2005;15(2):319–24. https://doi.org/10.1111/j.1525-1438.2005.15223.x.
Bige Ö, Demir A, Saatli B, Koyuncuoğlu M, Saygılı U. Laparoscopy versus laparotomy for the management of endometrial carcinoma in morbidly obese patients: a prospective study. J Turkish Ger Gynecol Assoc. 2015;16(3):164–9. https://doi.org/10.5152/jtgga.2015.15128.
Knocke TH, Kucera H, Weidinger B, Höller W, Pötter R. Primary treatment of endometrial carcinoma with high-dose-rate brachytherapy: results of 12 years of experience with 280 patients. Int J Radiat Oncol Biol Phys. 1997;37(2):359–65. https://doi.org/10.1016/S0360-3016(96)00486-5.
Coon D, Beriwal S, Heron DE, et al. High-dose-rate Rotte “Y” applicator brachytherapy for definitive treatment of medically inoperable endometrial cancer: 10-year results. Int J Radiat Oncol Biol Phys. 2008;71(3):779–83. https://doi.org/10.1016/j.ijrobp.2007.10.026.
Fishman DA, Roberts KB, Chambers JT, Kohorn EI, Schwartz PE, Chambers SK. Radiation therapy as exclusive treatment for medically inoperable patients with stage I and II endometrioid carcinoma of the endometrium. Gynecol Oncol. 1996;61(2):189–96. https://doi.org/10.1006/gyno.1996.0123.
Van Nguyen T, Petereit DG. High-dose-rate brachytherapy for medically inoperable stage I endometrial cancer. Gynecol Oncol. 1998;71(2):196–203. https://doi.org/10.1006/gyno.1998.5148.
Niazi TM, Souhami L, Portelance L, Bahoric B, Gilbert L, Stanimir G. Long-term results of high-dose-rate brachytherapy in the primary treatment of medically inoperable stage I-II endometrial carcinoma. J Radiat Oncol Biol Phys. 2005. https://doi.org/10.1016/j.ijrobp.2005.04.036.
Acharya S, Esthappan J, Badiyan S, et al. Medically inoperable endometrial cancer in patients with a high body mass index (BMI): patterns of failure after 3-D image-based high dose rate (HDR) brachytherapy. Radiother Oncol. 2016;118:167–72. https://doi.org/10.1016/j.radonc.2015.12.019.
Vandenbroucke JP, Von Elm E, Altman DG, et al. Strengthening the reporting of observational studies in epidemiology (STROBE): explanation and elaboration. Epidemiology. 2007;18(6):805–35. https://doi.org/10.1097/EDE.0b013e3181577511.
Clavien PA, Barkun J, De Oliveira ML, et al. The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg. 2009;250(2):187–96. https://doi.org/10.1097/SLA.0b013e3181b13ca2.
Alhilli MM, Podratz KC, Dowdy SC, et al. Preoperative biopsy and intraoperative tumor diameter predict lymph node dissemination in endometrial cancer. Gynecol Oncol. 2013;128:294–9. https://doi.org/10.1016/j.ygyno.2012.10.009.
Palomba S, Ghezzi F, Falbo A, et al. Conversion in endometrial cancer patients scheduled for laparoscopic staging: a large multicenter analysis: conversions and endometrial cancer. Surg Endosc. 2014;28(11):3200–9. https://doi.org/10.1007/s00464-014-3589-4.
Shalowitz DI, Epstein AJ, Buckingham L, Ko EM, Giuntoli RL. Survival implications of time to surgical treatment of endometrial cancers. Am J Obstet Gynecol. 2017;216(3):268.e1-268.e18. https://doi.org/10.1016/j.ajog.2016.11.1050.
Tseng JH, Long Roche K, Jernigan AM, Salani R, Bristow RE, Fader AN. Lifestyle and weight management counseling in uterine cancer survivors: a study of the uterine cancer action network. Int J Gynecol Cancer. 2015;25(7):1285–91. https://doi.org/10.1097/IGC.0000000000000475.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure
The authors report no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Ertel, M., Staley, S.A., Nguyen, T. et al. Contemporary Incidence of Medical Inoperability in Clinical Stage I Endometrial Cancer. Ann Surg Oncol 28, 8987–8995 (2021). https://doi.org/10.1245/s10434-021-10313-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-021-10313-6