Abstract
Background
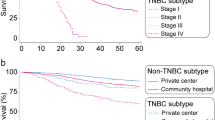
A subset of triple-negative breast cancer (TNBC) is characterized by aggressive disease, rapid relapse, and mortality within 24 months of diagnosis, termed “rapid relapse” TNBC (rrTNBC). The objective of this study is to define the association between sociodemographic variables and surgical management among rrTNBC patients in the Surveillance, Epidemiology and End Results (SEER) Program.
Methods
TNBC patients diagnosed from January 1, 2010 to December 31, 2014 with local or regional disease were identified in SEER. Patients were stratified as rrTNBC, defined as disease specific mortality ≤ 24 months after diagnosis, and non-rrTNBC. Chi-squared tests, t tests, and multivariable logistic regression were used to assess the association of rapid relapse with sociodemographic variables and surgical management.
Results
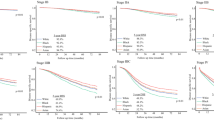
The cohort included 8% (1378/17,369) rrTNBCs. A higher proportion of rrTNBC patients had no surgery (11.7%) compared with non-rrTNBC (2.6%). Omission of axillary staging among patients who had surgery was 6.2% rrTNBC versus 4.5% non-rrTNBC. Black race (odds ratio [OR] 1.22, 95% confidence interval [CI] 1.05–1.43; p = 0.01; white ref), Medicaid or no insurance (Medicaid OR 1.53, 95% CI 1.31–1.79; p < 0.001; no insurance OR 1.74, 95% CI 1.31–2.32; p < 0.001; private ref), single status (OR 1.19, 95% CI 1.01–1.39; p = 0.03; married ref), no breast (OR 2.35, 95% CI 1.77–3.11; p < 0.001; mastectomy ref), and no axillary surgery (OR 1.44, 95% CI 1.13–1.83; p = 0.003 axillary surgery ref) were associated with rapid relapse.
Conclusions
Medicaid or no insurance, single status, black race, and no surgery are associated with higher odds of rrTNBC in SEER. These results indicate an interplay between socioeconomic factors, clinical and genomic variables may be disproportionately contributing to worse outcomes among a subset of TNBC patients.


Similar content being viewed by others
References
Bauer KR, Brown M, Cress RD, Parise CA, Caggiano V. Descriptive analysis of estrogen receptor (ER)-negative, progesterone receptor (PR)-negative, and HER2-negative invasive breast cancer, the so-called triple-negative phenotype: a population-based study from the California cancer Registry. Research Support, N.I.H., Extramural Research Support, Non-U.S. Gov't Research Support, U.S. Gov't, P.H.S. Cancer. 2007;109(9):1721–8. https://doi.org/10.1002/cncr.22618.
Lin NU, Vanderplas A, Hughes ME, et al. Clinicopathologic features, patterns of recurrence, and survival among women with triple-negative breast cancer in the National Comprehensive Cancer Network. Research Support, N.I.H., Extramural Research Support, Non-U.S. Gov't. Cancer. 2012;118(22):5463–72. https://doi.org/10.1002/cncr.27581.
Lin NU, Claus E, Sohl J, Razzak AR, Arnaout A, Winer EP. Sites of distant recurrence and clinical outcomes in patients with metastatic triple-negative breast cancer: high incidence of central nervous system metastases. Cancer. 2008;113(10):2638–45. https://doi.org/10.1002/cncr.23930.
Dent R, Trudeau M, Pritchard KI, et al. Triple-negative breast cancer: clinical features and patterns of recurrence. Clin Cancer Res. 2007;13(15 Pt 1):4429–34. https://doi.org/10.1158/1078-0432.CCR-06-3045.
Kassam F, Enright K, Dent R, et al. Survival outcomes for patients with metastatic triple-negative breast cancer: implications for clinical practice and trial design. Multicenter Study Research Support, Non-U.S. Gov't. Clin Breast Cancer. 2009;9(1):29–33. https://doi.org/10.3816/CBC.2009.n.005.
Schmid P, Adams S, Rugo HS, et al. Atezolizumab and nab-paclitaxel in advanced triple-negative breast cancer. N Engl J Med. 2018;379(22):2108–21. https://doi.org/10.1056/NEJMoa1809615.
van Roozendaal LM, Smit LHM, Duijsens G, et al. Risk of regional recurrence in triple-negative breast cancer patients: a Dutch cohort study. Breast Cancer Res Treat. 2016;156(3):465–72. https://doi.org/10.1007/s10549-016-3757-4.
Ghosh J, Agarwal S, Ganguly S, et al. Patterns of recurrence in triple negative breast cancer patients (automated IHC): an Indian Tertiary Care Center data. J Clin Oncol. 2018;36(15_suppl):e13128. https://doi.org/10.1200/JCO.2018.36.15_suppl.e13128.
Cancer Genome Atlas N. Comprehensive molecular portraits of human breast tumours. Research Support, N.I.H., Extramural Research Support, Non-U.S. Gov't Research Support, U.S. Gov't, Non-P.H.S. Nature. 2012;490(7418):61–70. https://doi.org/10.1038/nature11412.
Curtis C, Shah SP, Chin SF, et al. The genomic and transcriptomic architecture of 2000 breast tumours reveals novel subgroups. Research Support, N.I.H., Extramural Research Support, Non-U.S. Gov't. Nature. 2012;486(7403):346–52. https://doi.org/10.1038/nature10983.
Stover DG, Coloff JL, Barry WT, Brugge JS, Winer EP, Selfors LM. The role of proliferation in determining response to neoadjuvant chemotherapy in breast cancer: a gene expression-based meta-analysis. Clin Cancer Res. 2016;22(24):6039–50. https://doi.org/10.1158/1078-0432.CCR-16-0471.
Zhang Y, Nock W, Wyse M, et al. Machine learning predicts rapid relapse of triple negative breast cancer. bioRxiv. 2019:613604. https://doi.org/10.1101/613604.
Hunter CP. Epidemiology, stage at diagnosis, and tumor biology of breast carcinoma in multiracial and multiethnic populations. Cancer. 2000;88(S5):1193–202. https://doi.org/10.1002/(SICI)1097-0142(20000301)88:5+%3c1193::AID-CNCR3%3e3.0.CO;2-D.
Lantz PM, Mujahid M, Schwartz K, et al. The influence of race, ethnicity, and individual socioeconomic factors on breast cancer stage at diagnosis. Am J Public Health. 2006;96(12):2173–8. https://doi.org/10.2105/AJPH.2005.072132.
Schwartz KL, Crossley-May H, Vigneau FD, Brown K, Banerjee M. Race, socioeconomic status and stage at diagnosis for five common malignancies. Cancer Causes Control. 2003;14(8):761–6.
Harper S, Lynch J, Meersman SC, Breen N, Davis WW, Reichman MC. Trends in area-socioeconomic and race-ethnic disparities in breast cancer incidence, stage at diagnosis, screening, mortality, and survival among women ages 50 years and over (1987–2005). Cancer Epidemiol Biomark Prev. 2009;18(1):121–31. https://doi.org/10.1158/1055-9965.EPI-08-0679.
Huo D, Hu H, Rhie SK, et al. Comparison of breast cancer molecular features and survival by African and European ancestry in the cancer genome atlas. JAMA Oncol. 2017;3(12):1654–62. https://doi.org/10.1001/jamaoncol.2017.0595.
Iqbal J, Ginsburg O, Rochon PA, Sun P, Narod SA. Differences in breast cancer stage at diagnosis and cancer-specific survival by race and ethnicity in the United States. JAMA. 2015;313(2):165–73. https://doi.org/10.1001/jama.2014.17322.
Asad S, Barcenas C, Bleicher R, et al. Sociodemographic factors associated with rapid relapse in triple negative breast cancer: a multi-institution study. J Natl Compr Cancer Netw. (in press).
Institute NC. Surveillance, Epidemiology, and End Results (SEER) Program. 2020. www.seer.cancer.gov
Institute NC. SEER*Stat software version 8.3.6. www.seer.cancer.gov/seerstat
Yu M, Tatalovich Z, Gibson JT, Cronin KA. Using a composite index of socioeconomic status to investigate health disparities while protecting the confidentiality of cancer registry data. Cancer Causes Control. 2014;25(1):81–92. https://doi.org/10.1007/s10552-013-0310-1.
Yost K, Perkins C, Cohen R, Morris C, Wright W. Socioeconomic status and breast cancer incidence in California for different race/ethnic groups. Cancer Causes Control. 2001;12(8):703–11. https://doi.org/10.1023/a:1011240019516.
National Cancer Institute S, Epidemiology, and End Results Program. Census tract–level SES and rurality database (2000–2015). National Cancer Institute. Accessed 26 May 2020. https://seer-cancer-gov.proxy.lib.ohio-state.edu/seerstat/databases/census-tract/index.html.
Axelsson CK, Mouridsen HT, Zedeler K. Axillary dissection of level I and II lymph nodes is important in breast cancer classification. The Danish Breast Cancer Cooperative Group (DBCG). Eur J Cancer. 1992;28a(8–9):1415–8. https://doi.org/10.1016/0959-8049(92)90534-9.
Voduc KD, Cheang MC, Tyldesley S, Gelmon K, Nielsen TO, Kennecke H. Breast cancer subtypes and the risk of local and regional relapse. J Clin Oncol. 2010;28(10):1684–91. https://doi.org/10.1200/jco.2009.24.9284.
Dreyer MS, Nattinger AB, McGinley EL, Pezzin LE. Socioeconomic status and breast cancer treatment. Breast Cancer Res Treat. 2018;167(1):1–8. https://doi.org/10.1007/s10549-017-4490-3.
Halpern MT, Bian J, Ward EM, Schrag NM, Chen AY. Insurance status and stage of cancer at diagnosis among women with breast cancer. Cancer. 2007;110(2):403–11. https://doi.org/10.1002/cncr.22786.
Liu Y-l, Wang D-w, Yang Z-c, et al. Marital status is an independent prognostic factor in inflammatory breast cancer patients: an analysis of the surveillance, epidemiology, and end results database. Breast Cancer Res Treat. 2019;178(2):379–88. https://doi.org/10.1007/s10549-019-05385-8.
Abdel-Rahman O. Impact of NCI Socioeconomic index on the outcomes of nonmetastatic breast cancer patients: analysis of SEER Census Tract-Level Socioeconomic Database. Clin Breast Cancer. 2019;19(6):e717–22. https://doi.org/10.1016/j.clbc.2019.06.013.
Obeng-Gyasi S, Timsina L, Miller KD, Ludwig KK, Fisher CS, Haggstrom DA. The implications of insurance status on presentation, surgical management, and mortality among nonmetastatic breast cancer patients in Indiana. Surgery. 2018;164(6):1366–71. https://doi.org/10.1016/j.surg.2018.07.012.
Shi R, Taylor H, McLarty J, Liu L, Mills G, Burton G. Effects of payer status on breast cancer survival: a retrospective study. BMC Cancer. 2015;15:211. https://doi.org/10.1186/s12885-015-1228-7.
Martínez ME, Unkart JT, Tao L, et al. Prognostic significance of marital status in breast cancer survival: a population-based study. PLoS One. 2017;12(5):e0175515. https://doi.org/10.1371/journal.pone.0175515.
Daly B, Olopade OI. A perfect storm: how tumor biology, genomics, and health care delivery patterns collide to create a racial survival disparity in breast cancer and proposed interventions for change. CA Cancer J Clin. 2015;65(3):221–38. https://doi.org/10.3322/caac.21271.
DeSantis CE, Miller KD, Goding Sauer A, Jemal A, Siegel RL. Cancer statistics for African Americans, 2019. CA Cancer J Clin. 2019;69(3):211–33. https://doi.org/10.3322/caac.21555.
Newman LA, Kaljee LM. Health disparities and triple-negative breast cancer in African American women: a review. JAMA Surg. 2017;152(5):485–93. https://doi.org/10.1001/jamasurg.2017.0005.
Bickell NA, Wang JJ, Oluwole S, et al. Missed opportunities: racial disparities in adjuvant breast cancer treatment. J Clin Oncol. 2006;24(9):1357–62. https://doi.org/10.1200/jco.2005.04.5799.
Solar O. A conceptual framework for action on the social determinants of health. Social Determinants of Health Discussion Paper 2 (Policy and Practice). 2010. Accessed 11 March 2020.
Jagsi R, Pottow JA, Griffith KA, et al. Long-term financial burden of breast cancer: experiences of a diverse cohort of survivors identified through population-based registries. J Clin Oncol. 2014;32(12):1269–76. https://doi.org/10.1200/jco.2013.53.0956.
Carrera PM, Kantarjian HM, Blinder VS. The financial burden and distress of patients with cancer: understanding and stepping-up action on the financial toxicity of cancer treatment. CA Cancer J Clin. 2018;68(2):153–65. https://doi.org/10.3322/caac.21443.
Freedman RA, Virgo KS, He Y, et al. The association of race/ethnicity, insurance status, and socioeconomic factors with breast cancer care. Cancer. 2011;117(1):180–9. https://doi.org/10.1002/cncr.25542.
Network NCC. NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines), Breast Cancer. Accessed 21 June 2020. Available at https://www.nccn.org/professionals/physician_gls/pdf/breast.pdf.
Malmström P, Holmberg L, Anderson H, et al. Breast conservation surgery, with and without radiotherapy, in women with lymph node-negative breast cancer: a randomised clinical trial in a population with access to public mammography screening. Eur J Cancer. 2003;39(12):1690–7. https://doi.org/10.1016/s0959-8049(03)00324-1.
Jagsi R, Abrahamse PH, Lee KL, et al. Treatment decisions and employment of breast cancer patients: results of a population-based survey. Cancer. 2017;123(24):4791–9. https://doi.org/10.1002/cncr.30959.
Gu J, Groot G, Boden C, Busch A, Holtslander L, Lim H. Review of factors influencing women’s choice of mastectomy versus breast conserving therapy in early stage breast cancer: a systematic review. Clin Breast Cancer. 2018;18(4):e539–54. https://doi.org/10.1016/j.clbc.2017.12.013.
Greenup RA, Obeng-Gyasi S, Thomas S, et al. The effect of hospital volume on breast cancer mortality. Ann Surg. 2018;267(2):375–81. https://doi.org/10.1097/sla.0000000000002095.
Kingsmore D, Hole D, Gillis C. Why does specialist treatment of breast cancer improve survival? The role of surgical management. Br J Cancer. 2004;90(10):1920–5. https://doi.org/10.1038/sj.bjc.6601846.
Willems S, De Maesschalck S, Deveugele M, Derese A, De Maeseneer J. Socio-economic status of the patient and doctor-patient communication: does it make a difference? Patient Educ Counsel. 2005;56(2):139–46.
Sheppard VB, Isaacs C, Luta G, et al. Narrowing racial gaps in breast cancer chemotherapy initiation: the role of the patient–provider relationship. Breast Cancer Res Treat. 2013;139(1):207–16. https://doi.org/10.1007/s10549-013-2520-3.
Krieger N, Chen JT, Waterman PD, Soobader MJ, Subramanian SV, Carson R. Geocoding and monitoring of US socioeconomic inequalities in mortality and cancer incidence: does the choice of area-based measure and geographic level matter? The Public Health Disparities Geocoding Project. Am J Epidemiol. 2002;156(5):471–82.
Noone AM, Lund JL, Mariotto A, et al. Comparison of SEER treatment data with medicare claims. Med Care. 2016;54(9):e55-64. https://doi.org/10.1097/mlr.0000000000000073.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
The authors declare that they have no disclosures to report.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Obeng-Gyasi, S., Asad, S., Fisher, J.L. et al. Socioeconomic and Surgical Disparities are Associated with Rapid Relapse in Patients with Triple-Negative Breast Cancer. Ann Surg Oncol 28, 6500–6509 (2021). https://doi.org/10.1245/s10434-021-09688-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-021-09688-3