Abstract
Background
The increasing incidence of hepatocellular carcinoma (HCC) coupled with rising health care costs contributes to high end-of-life expenditures. The current study aimed to characterize health care expenditures and hospice use among patients with HCC using a large, national database.
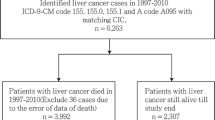
Methods
The Surveillance, Epidemiology, and End Results (SEER)-Medicare-linked database was used to identify patients with HCC. Logistic regression was used to identify factors associated with overall hospice use and end-of-life expenditures among individuals who died of HCC.
Results
Among 14,369 Medicare beneficiaries with HCC, 8069 (63.7 %) used hospice. Racial/ethnic minority patients were less likely to use hospice services during the last year of life than white patients (no hospice: n = 2034 [44.3 %] vs. hospice: n = 2513 [31.1 %]). Social vulnerability also had an impact on the likelihood of patients using hospice services; in particular, the probability of hospice use among patients declined as social vulnerability increased (P < 0.05). Hospice use was associated with an approximate $10,000 decrease in inpatient expenditures (hospice: US$7900 [IQR, US$0–26,600] vs. no hospice: US$18,000 [IQR $400-49,100]; P < 0.001) and $1300 decrease in outpatient expenditures (hospice: US$900 [IQR, US$0–4500] vs. non-hospice: US$2200 [IQR, US$200–7900; P < 0.001) compared with individuals who did not use hospice.
Conclusions
Minority patients and individuals residing in high-vulnerability areas were less likely to use hospice. Patients who used hospice at the end of life had a reduction in inpatient and outpatient Medicare claims. Patients with HCC in need of hospice services should be ensured timely referral regardless of race/ethnicity or social vulnerability.


Similar content being viewed by others
References
Balogh J, Victor D, Asham EH, et al. Hepatocellular carcinoma: a review. J Hepatocell Carcinoma. 2016;3:41–53. https://doi.org/10.2147/JHC.S61146.
Golabi P, Fazel S, Otgonsuren M, Sayiner M, Locklear CT, Younossi ZM. Mortality assessment of patients with hepatocellular carcinoma according to underlying disease and treatment modalities. Med Baltimore. 2017;96:e5904. https://doi.org/10.1097/MD.0000000000005904.
Yang JD, Hainaut P, Gores GJ, Amadou A, Plymoth A, Roberts LR. A global view of hepatocellular carcinoma: trends, risk, prevention, and management. Nat Rev Gastroenterol Hepatol. 2019;10(16):589–604. https://doi.org/10.1038/s41575-019-0186-y.
Liang TJ, Ward JW. Hepatitis C in Injection-drug users: a hidden danger of the opioid epidemic. New Engl J Med. 2018;03(378):1169–71. https://doi.org/10.1056/NEJMp1716871.
Pascual S, Miralles C, Bernabé JM, Irurzun J, Planells M. Surveillance and diagnosis of hepatocellular carcinoma: a systematic review. World J Clin Cases. 2019;7:2269–86. https://doi.org/10.12998/wjcc.v7.i16.2269.
Tejeda-Maldonado J, García-Juárez I, Aguirre-Valadez J, et al. Diagnosis and treatment of hepatocellular carcinoma: an update. World J Hepatol. 2015;7:362–76. https://doi.org/10.4254/wjh.v7.i3.362.
Bekelman JE, Halpern SD, Blankart CR, et al. Comparison of site of death, health care utilization, and hospital expenditures for patients dying with cancer in 7 developed countries. JAMA. 2016;315:272–83. https://doi.org/10.1001/jama.2015.18603.
Rice DR, Farooq A, Hyer JM, et al. Health expenditures and financial burden among patients with major gastrointestinal cancers relative to other common cancers in the United States. Surgery. 2020;167:985–90. https://doi.org/10.1016/j.surg.2020.02.029.
Tangka FK, Trogdon JG, Richardson LC, Howard D, Sabatino SA, Finkelstein EA. Cancer treatment cost in the United States: has the burden shifted over time? Cancer. 2010;116:3477–84. https://doi.org/10.1002/cncr.25150.
Elkin EB, Bach PB. Cancer’s next frontier: addressing high and increasing costs. JAMA. 2010;303:1086–7. https://doi.org/10.1001/jama.2010.283.
U. S. National Institutes of Health, National Cancer Institute. Surveillance, Epidemiology, and End Results Program (SEER) Database. Retrieved 30 September 2020.
Quan H, Sundararajan V, Halfon P, et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care. 2005;43:1130–9. https://doi.org/10.1097/01.mlr.0000182534.19832.83.
Quan H, Li B, Couris CM, et al. Updating and validating the Charlson comorbidity index and score for risk adjustment in hospital discharge abstracts using data from 6 countries. Am J Epidemiol. 2011;173:676–82. https://doi.org/10.1093/aje/kwq433.
CDC. Social Vulnerability Index (SVI). Retrieved 15 October 2020. https://www.atsdr.cdc.gov/placeandhealth/svi/index.html.
Fairfield KM, Murray KM, Wierman HR, et al. Disparities in hospice care among older women dying with ovarian cancer. Gynecol Oncol. 2012;125:14–8. https://doi.org/10.1016/j.ygyno.2011.11.041.
Enomoto LM, Schaefer EW, Goldenberg D, Mackley H, Koch WM, Hollenbeak CS. The cost of hospice services in terminally ill patients with head and neck cancer. JAMA Otolaryngol Head Neck Surg. 2015;141:1066–74. https://doi.org/10.1001/jamaoto.2015.2162.
Wachterman MW, Hailpern SM, Keating NL, Kurella Tamura M, O’Hare AM. Association between hospice length of stay, health care utilization, and medicare costs at the end of life among patients who received maintenance hemodialysis. JAMA Intern Med. 2018;178:792–9. https://doi.org/10.1001/jamainternmed.2018.0256.
Bureau of Labor Statistics Consumer Price Index. Accessed 15 October 2020. https://www.bls.gov/data/inflation_calculator.htm.
Nipp RD, Sonet EM, Guy GP. Communicating the financial burden of treatment with patients. Am Soc Clin Oncol Educ Book. 2018;38:524–31. https://doi.org/10.1200/EDBK_201051.
Wang SY, Hall J, Pollack CE, et al. Associations between end-of-life cancer care patterns and medicare expenditures. J Natl Compr Canc Netw. 2016;14:1001–8. https://doi.org/10.6004/jnccn.2016.0107.
Mariotto AB, Yabroff KR, Shao Y, Feuer EJ, Brown ML. Projections of the cost of cancer care in the United States: 2010–2020. J Natl Cancer Inst. 2011;103:117–28. https://doi.org/10.1093/jnci/djq495.
Cheraghlou S, Gahbauer EA, Leo-Summers L, Stabenau HF, Chaudhry SI, Gill TM. Restricting symptoms before and after admission to hospice. Am J Med. 2016;129:754.e7-754.e15. https://doi.org/10.1016/j.amjmed.2016.02.017.
Connor SR, Pyenson B, Fitch K, Spence C, Iwasaki K. Comparing hospice and nonhospice patient survival among patients who die within a three-year window. J Pain Symptom Manag. 2007;33:238–46. https://doi.org/10.1016/j.jpainsymman.2006.10.010.
Temel JS, Greer JA, Muzikansky A, et al. Early palliative care for patients with metastatic non-small-cell lung cancer. New Engl J Med. 2010;363:733–42. https://doi.org/10.1056/NEJMoa1000678.
Weerakkody I, Hales S, Fernandes S, et al. The quality of dying and death in a residential hospice. J Pain Symptom Manag. 2018;56:567–74. https://doi.org/10.1016/j.jpainsymman.2018.07.004.
American College of Surgeons’ Committee on Ethics. Statement on principles guiding care at the end of life. Bull Am Coll Surg. 1998;83(4):46.
Cancer care during the last phase of life. J Clin Oncol. 1998;16:1986–96. https://doi.org/10.1200/JCO.1998.16.5.1986.
Dans M, Smith T, Back A, et al. NCCN Guidelines insights: palliative care, version 2.2017. J Natl Compr Canc Netw. 2017;15:989–97. https://doi.org/10.6004/jnccn.2017.0132.
Organization NHaPC. Facts and Figures: Hospice Care in America. Retrieved 15 October 2020. https://www.nhpco.org/factsfigures/.
Wallace CL. Predictors of Timing in Hospice Utilization: The Role of Family in the Decision for Hospice Care. Arlington, TX: University of Texas; 2015.
Alcaraz KI, Wiedt TL, Daniels EC, Yabroff KR, Guerra CE, Wender RC. Understanding and addressing social determinants to advance cancer health equity in the United States: a blueprint for practice, research, and policy. CA Cancer J Clin. 2020;70:31–46. https://doi.org/10.3322/caac.21586.
Nelson A. Unequal treatment: confronting racial and ethnic disparities in health care. J Natl Med Assoc. 2002;94:666–8.
Thylur RP, Roy SK, Shrivastava A, LaVeist TA, Shankar S, Srivastava RK. Assessment of risk factors, and racial and ethnic differences in hepatocellular carcinoma. JGH Open. 2020;4:351–9. https://doi.org/10.1002/jgh3.12336.
Paredes AZ, Hyer JM, Tsilimigras DI, et al. Hospice utilization among Medicare beneficiaries dying from pancreatic cancer. J Surg Oncol. 2019;120:624–31. https://doi.org/10.1002/jso.25623.
Unroe KT, Sachs GA, Dennis ME, et al. Effect of hospice use on costs of care for long-stay nursing home decedents. J Am Geriatr Soc. 2016;64:723–30. https://doi.org/10.1111/jgs.14070.
Farooq A, Merath K, Hyer JM, et al. Financial toxicity risk among adult patients undergoing cancer surgery in the United States: an analysis of the National Inpatient Sample. J Surg Oncol. 2019;120:397–406. https://doi.org/10.1002/jso.25605.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure
There are no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Rice, D.R., Hyer, J.M., Diaz, A. et al. End-of-Life Hospice Use and Medicare Expenditures Among Patients Dying of Hepatocellular Carcinoma. Ann Surg Oncol 28, 5414–5422 (2021). https://doi.org/10.1245/s10434-021-09606-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-021-09606-7