Abstract
Background
The American Society of Clinical Oncology guidelines recommend early referral to reproductive endocrinology and infertility (REI) specialists for young women diagnosed with breast cancer. Current practice patterns demonstrate an increased utilization of neoadjuvant chemotherapy (NAC). We evaluated premenopausal women with breast cancer after consultation with a Fertility Nurse Specialist (FNS) and determine factors associated with referral to REI specialists.
Methods
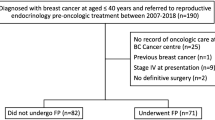
This retrospective review included all premenopausal women diagnosed at our institution with stage 0–III unilateral breast cancers between 2009 and 2015 who completed an FNS consultation. Clinicopathologic features and factors associated with referral to REI after FNS consultation were analyzed.
Results
A total of 334 women were identified. Median age was 35 years (interquartile range 32–38). The majority of women were single (n = 198, 59.3%) and nulliparous (n = 239, 71.6%). REI referrals were common (n = 237, 71.0%). The Breast Surgery service was the most frequent referring service (n = 194, 58.1%), with significantly more REI referrals compared to Breast Medicine and Genetics services (p = 0.002). Nulliparity was associated with REI referral (p < 0.0001). Adjuvant chemotherapy (p = 0.003) was associated with pursuing REI referral, whereas NAC (p < 0.001) was associated with declining REI referral.
Conclusions
Most women elected to consult with an REI specialist, confirming strong interest in fertility preservation among premenopausal women with breast cancer. However, women receiving NAC more frequently declined referral to REI, suggesting that the need to start NAC may influence decisions regarding fertility preservation. With increasing utilization of NAC, our study supports the need for further counseling and education regarding fertility preservation for women undergoing NAC.
Similar content being viewed by others
References
Hery C, Ferlay J, Boniol M, Autier P. Changes in breast cancer incidence and mortality in middle-aged and elderly women in 28 countries with Caucasian majority populations. Ann Oncol. 2008;19(5):1009–18.
Anders CK, Johnson R, Litton J, Phillips M, Bleyer A. Breast cancer before age 40 years. Semin Oncol. 2009;36(3):237–49.
Merlo DF, Ceppi M, Filiberti R, et al. Breast cancer incidence trends in European women aged 20–39 years at diagnosis. Breast Cancer Res Treat. 2012;134(1):363–70.
Murphy BL, Day CN, Hoskin TL, Habermann EB, Boughey JC. Adolescents and young adults with breast cancer have more aggressive disease and treatment than patients in their forties. Ann Surg Oncol. 2019;26(12):3920–30.
Cakmak H, Rosen MP. Random-start ovarian stimulation in patients with cancer. Curr Opin Obstet Gynecol. 2015;27(3):215–21.
Mathews TJ, Hamilton BE. Mean Age of Mothers is on the Rise: United States, 2000–2014. NCHS Data Brief. 2016;232:1–8.
Letourneau JM, Ebbel EE, Katz PP, et al. Acute ovarian failure underestimates age-specific reproductive impairment for young women undergoing chemotherapy for cancer. Cancer. 2012;118(7):1933–9.
Partridge AH, Ruddy KJ. Fertility and adjuvant treatment in young women with breast cancer. Breast. 2007;16 Suppl 2:S175–81.
Soleimani R, Heytens E, Darzynkiewicz Z, Oktay K. Mechanisms of chemotherapy-induced human ovarian aging: double strand DNA breaks and microvascular compromise. Aging (Albany NY). 2011;3(8):782–93.
Mougalian SS, Soulos PR, Killelea BK, et al. Use of neoadjuvant chemotherapy for patients with stage I to III breast cancer in the United States. Cancer. 2015;121(15):2544–52.
Murphy BL, Day CN, Hoskin TL, Habermann EB, Boughey JC. Neoadjuvant chemotherapy use in breast cancer is greatest in excellent responders: triple-negative and HER2 + subtypes. Ann Surg Oncol. 2018;25(8):2241–8.
Puig CA, Hoskin TL, Day CN, Habermann EB, Boughey JC. National trends in the use of neoadjuvant chemotherapy for hormone receptor-negative breast cancer: a national cancer data base study. Ann Surg Oncol. 2017;24(5):1242–50.
Alberro JA, Ballester B, Deulofeu P, et al. Long-term outcomes for neoadjuvant versus adjuvant chemotherapy in early breast cancer: meta-analysis of individual patient data from ten randomised trials. Lancet Oncol. 2018;19(1):27–39.
von Minckwitz G, Untch M, Blohmer JU, et al. Definition and impact of pathologic complete response on prognosis after neoadjuvant chemotherapy in various intrinsic breast cancer subtypes. J Clin Oncol. 2012;30(15):1796–804.
Chen HL, Zhou MQ, Tian W, Meng KX, He HF. Effect of age on breast cancer patient prognoses: a population-based study using the SEER 18 Database. PLoS ONE. 2016;11(10):e0165409.
Kollias J, Elston CW, Ellis IO, Robertson JF, Blamey RW. Early-onset breast cancer–histopathological and prognostic considerations. Br J Cancer. 1997;75(9):1318–23.
Mamtani A, Barrio AV, King TA, et al. How often does neoadjuvant chemotherapy avoid axillary dissection in patients with histologically confirmed nodal metastases? Results of a prospective study. Ann Surg Oncol. 2016;23(11):3467–74.
Howard-Anderson J, Ganz PA, Bower JE, Stanton AL. Quality of life, fertility concerns, and behavioral health outcomes in younger breast cancer survivors: a systematic review. J Natl Cancer Inst. 2012;104(5):386–405.
Ruddy KJ, Gelber SI, Tamimi RM, et al. Prospective study of fertility concerns and preservation strategies in young women with breast cancer. J Clin Oncol. 2014;32(11):1151–6.
Dunn J, Steginga SK. Young women’s experience of breast cancer: defining young and identifying concerns. Psychooncology. 2000;9(2):137–46.
Goldfarb SB, Kamer SA, Oppong BA, et al. Fertility preservation for the young breast cancer patient. Ann Surg Oncol. 2016;23(5):1530–6.
Lambertini M, Fontana V, Massarotti C, et al. Prospective study to optimize care and improve knowledge on ovarian function and/or fertility preservation in young breast cancer patients: Results of the pilot phase of the PREgnancy and FERtility (PREFER) study. Breast. 2018;41:51–6.
Partridge AH, Gelber S, Peppercorn J, et al. Web-based survey of fertility issues in young women with breast cancer. J Clin Oncol. 2004;22(20):4174–83.
Loren AW, Mangu PB, Beck LN, et al. Fertility preservation for patients with cancer: American Society of Clinical Oncology clinical practice guideline update. J Clin Oncol. 2013;31(19):2500–10.
Duffy CM, Allen SM, Clark MA. Discussions regarding reproductive health for young women with breast cancer undergoing chemotherapy. J Clin Oncol. 2005;23(4):766–73.
Jukkala AM, Azuero A, McNees P, Bates GW, Meneses K. Self-assessed knowledge of treatment and fertility preservation in young women with breast cancer. Fertil Steril. 2010;94(6):2396–8.
Peate M, Meiser B, Friedlander M, et al. It’s now or never: fertility-related knowledge, decision-making preferences, and treatment intentions in young women with breast cancer—an Australian fertility decision aid collaborative group study. J Clin Oncol. 2011;29(13):1670–7.
Ruddy KJ, Gelber S, Ginsburg ES, et al. Menopausal symptoms and fertility concerns in premenopausal breast cancer survivors: a comparison to age- and gravidity-matched controls. Menopause. 2011;18(1):105–8.
Moore HC, Unger JM, Phillips KA, et al. Goserelin for ovarian protection during breast-cancer adjuvant chemotherapy. N Engl J Med. 2015;372(10):923–32.
King TA, Morrow M. Surgical issues in patients with breast cancer receiving neoadjuvant chemotherapy. Nat Rev Clin Oncol. 2015;12(6):335–43.
Hershlag A, Mullin C, Bristow SL. Is fertility preservation feasible and safe with neoadjuvant therapy for breast cancer? J Glob Oncol. 2018;4:1–5.
Magno S, Carnevale S, Dentale F, Belella D, Linardos M, Masetti R. Neo-adjuvant chemotherapy and distress in breast cancer patients: The moderating role of generalized self-efficacy. 2017;35(15_suppl):e21570–70.
Crawford NM, Hoff HS, Mersereau JE. Infertile women who screen positive for depression are less likely to initiate fertility treatments. Hum Reprod. 2017;32(3):582–7.
Kim J, Oktay K, Gracia C, Lee S, Morse C, Mersereau JE. Which patients pursue fertility preservation treatments? A multicenter analysis of the predictors of fertility preservation in women with breast cancer. Fertil Steril. 2012;97(3):671–6.
Taylan E, Oktay KH. Current state and controversies in fertility preservation in women with breast cancer. World J Clin Oncol. 2017;8(3):241–8.
Joo BS, Park SH, An BM, Kim KS, Moon SE, Moon HS. Serum estradiol levels during controlled ovarian hyperstimulation influence the pregnancy outcome of in vitro fertilization in a concentration-dependent manner. Fertil Steril. 2010;93(2):442–6.
Oktay K, Taylan E, Kawahara T, Cillo GM. Robot-assisted orthotopic and heterotopic ovarian tissue transplantation techniques: surgical advances since our first success in 2000. Fertil Steril. 2019;111(3):604–6.
Azim AA, Costantini-Ferrando M, Oktay K. Safety of fertility preservation by ovarian stimulation with letrozole and gonadotropins in patients with breast cancer: a prospective controlled study. J Clin Oncol. 2008;26(16):2630–5.
Oktay K, Turan V, Bedoschi G, Pacheco FS, Moy F. Fertility preservation success subsequent to concurrent aromatase inhibitor treatment and ovarian stimulation in women with breast cancer. J Clin Oncol. 2015;33(22):2424–9.
Turan V, Bedoschi G, Moy F, Oktay K. Safety and feasibility of performing two consecutive ovarian stimulation cycles with the use of letrozole-gonadotropin protocol for fertility preservation in breast cancer patients. Fertil Steril. 2013;100(6):1681–5 e1681.
Martinez M, Rabadan S, Domingo J, Cobo A, Pellicer A, Garcia-Velasco JA. Obstetric outcome after oocyte vitrification and warming for fertility preservation in women with cancer. Reprod Biomed Online. 2014;29(6):722–8.
Cavagna F, Pontes A, Cavagna M, et al. A specific controlled ovarian stimulation (COS) protocol for fertility preservation in women with breast cancer undergoing neoadjuvant chemotherapy. Contemp Oncol (Pozn). 2017;21(4):290–4.
Cavagna F, Pontes A, Cavagna M, et al. Specific protocols of controlled ovarian stimulation for oocyte cryopreservation in breast cancer patients. Curr Oncol. 2018;25(6):e527–32.
Pereira N, Kelly AG, Stone LD, et al. Gonadotropin-releasing hormone agonist trigger increases the number of oocytes and embryos available for cryopreservation in cancer patients undergoing ovarian stimulation for fertility preservation. Fertil Steril. 2017;108(3):532–8.
Meirow D, Raanani H, Maman E, et al. Tamoxifen co-administration during controlled ovarian hyperstimulation for in vitro fertilization in breast cancer patients increases the safety of fertility-preservation treatment strategies. Fertil Steril. 2014;102(2):488–95 e483.
Moravek MB, Confino R, Smith KN, et al. Long-term outcomes in cancer patients who did or did not pursue fertility preservation. Fertil Steril. 2018;109(2):349–55.
Oktay K, Buyuk E, Libertella N, Akar M, Rosenwaks Z. Fertility preservation in breast cancer patients: a prospective controlled comparison of ovarian stimulation with tamoxifen and letrozole for embryo cryopreservation. J Clin Oncol. 2005;23(19):4347–53.
von Wolff M, Capp E, Jauckus J, Strowitzki T, Germeyer A, Ferti Psg. Timing of ovarian stimulation in patients prior to gonadotoxic therapy: an analysis of 684 stimulations. Eur J Obstet Gynecol Reprod Biol. 2016;199:146–9.
Lee S, Ozkavukcu S, Heytens E, Moy F, Oktay K. Value of early referral to fertility preservation in young women with breast cancer. J Clin Oncol. 2010;28(31):4683–6.
Lohrisch C, Paltiel C, Gelmon K, et al. Impact on survival of time from definitive surgery to initiation of adjuvant chemotherapy for early-stage breast cancer. J Clin Oncol. 2006;24(30):4888–94.
Letourneau JM, Sinha N, Wald K, et al. Random start ovarian stimulation for fertility preservation appears unlikely to delay initiation of neoadjuvant chemotherapy for breast cancer. Hum Reprod. 2017;32(10):2123–9.
Letourneau JM, Wald K, Sinha N, et al. Fertility preservation before breast cancer treatment appears unlikely to affect disease-free survival at a median follow-up of 43 months after fertility-preservation consultation. Cancer. 2019.
Davies C, Pan H, Godwin J, et al. Long-term effects of continuing adjuvant tamoxifen to 10 years versus stopping at 5 years after diagnosis of oestrogen receptor-positive breast cancer: ATLAS, a randomised trial. Lancet. 2013;381(9869):805–16.
Gray RG, Rea D, Handley K, et al. aTTom: Long-term effects of continuing adjuvant tamoxifen to 10 years versus stopping at 5 years in 6,953 women with early breast cancer. J Clin Oncol. 2013;31(15).
Rosenberg SM, Gelber S, Gelber RD, et al. Oncology physicians’ perspectives on practices and barriers to fertility preservation and the feasibility of a prospective study of pregnancy after breast cancer. J Adolesc Young Adult Oncol. 2017;6(3):429–34.
Braems G, Denys H, De Wever O, Cocquyt V, Van den Broecke R. Use of tamoxifen before and during pregnancy. Oncologist. 2011;16(11):1547–51.
Acknowledgment
This study was accepted for presentation in poster format at the 21st Annual Meeting of the American Society of Breast Surgeons, April 29–May 3, 2020, Las Vegas, NV.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure
The preparation of this manuscript was funded in part by NIH/NCI Cancer Center Support Grant No. P30 CA008748 to Memorial Sloan Kettering Cancer Center. Dr. Shari B. Goldfarb discloses research funding from Sprout Pharmaceuticals and Paxman Coolers Ltd, and consulting and advisory roles to Sermonix Pharmaceuticals, Bayer Healthcare, and Procter and Gamble. All other authors have no conflicts of interest to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Crown, A., Muhsen, S., Zabor, E.C. et al. Does Use of Neoadjuvant Chemotherapy Affect the Decision to Pursue Fertility Preservation Options in Young Women with Breast Cancer?. Ann Surg Oncol 27, 4740–4749 (2020). https://doi.org/10.1245/s10434-020-08883-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-020-08883-y